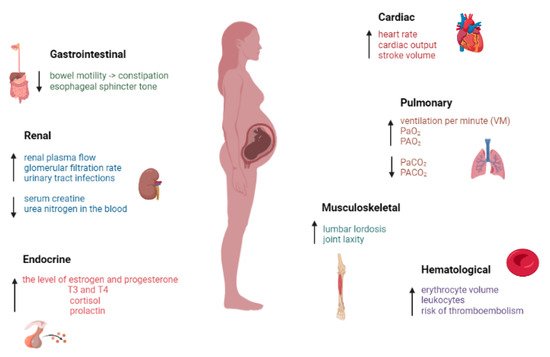
1. The Main Changes That Occur at the Organ Level
Regarding the cardiovascular system, during pregnancy heart rate can increase by up to 60% with the highest values registered from week 20 until birth. Cardiac output is required to increase and to maintain normal blood pressure. Initially, the increase in cardiac output is achieved by an increase in stroke volume, followed at the end of the third trimester by an increase in heart rhythm
[1][2][2,10]. The highest increase in cardiac output is achieved in the kidneys, uterus and skin to control the mother’s temperature and to produce nutrients needed for the fetus and to eliminate fetal and maternal waste
[3][4][5][11,12,13]. The presence of the pregnant uterus leads to the lateral movement of the heart. In the first weeks of pregnancy, the pregnant uterus begins to cause the mechanical compression of the inferior vena cava and the descending aorta. Thus, a reduction in cardiac output and venous return is observed, resulting in maternal hypotension and fetal acidemia. To correct and compensate for compression, heart rate and sympathetic tone increase. In many pregnant women, these mechanisms may be insufficient to support blood pressure and aortocaval compression syndrome may set in. This hypotensive syndrome is accompanied by symptoms such as pallor, dizziness, sweating and tachycardia, followed by bradycardia and hypotension in the supine position, while the severe form can cause death
[6][7][14,15].
During pregnancy, in the gastrointestinal tract, gastric motility is most affected. High levels of hormones, especially progesterone, cause smooth muscle relaxation and decreased bowel motility, thus prolonging gastric emptying time, leading to constipation
[8][16]. Likewise, the progesterone-mediated relaxation of the lower esophageal sphincter induces a decrease in its tone manifested as gastroesophageal reflux disease
[9][17]. Additionally, high hormone levels cause vomiting and nausea, known as morning sickness, which occur at any time of the day in more than 70% of pregnant women. However, if these conditions increase after week 20 or lead to ketosis with a massive weight loss, hyperemesis gravidarum can be reached and intravenous vitamins and fluids may be needed
[10][18].
Respiratory changes also occur in pregnant women. The diaphragm rises by about 2 cm, which leads to a 5% decrease in lung capacity. The current volume increases by up to 40% leading to a decrease in the expiratory reserve volume by 20% and an increase in ventilation per minute (VM). The increase in VM determines an increase in the level of arterial (PaO
2) and alveolar (PAO
2) pressure but also a decrease in the partial pressure of arterial carbon dioxide (PaCO
2). The decrease in PaCO
2 produces an increased gradient of carbon dioxide (CO
2) between mother and fetus, helping to deliver oxygen to the fetus and eliminate CO
2. Elevated progesterone levels create this gradient, with progesterone being a respiratory stimulant that sensitizes CO
2 receptors
[11][12][13][19,20,21]. Dyspnea in pregnancy, which occurs in about 70% of pregnant women is due to these low levels of PaCO
2 as well as decreased total lung capacity and increased VM. Thus, most often in the third trimester, the pregnant woman may experience a feeling of shortness of breath
[14][1].
In addition, renal changes were observed; renal plasma flow and glomerular filtration rate were increased. This increase in glomerular filtration rate maintains plasma sodium levels, which increase because of the activation the renin–angiotensin–aldosterone system, and also lowers serum creatine and urea nitrogen in the blood
[12][20]. At the renal level, elevated progesterone levels work to reduce peristalsis, urethral tone and contraction pressure, producing renal vasodilation. Furthermore, hormone levels, but also external mechanical compression and changes in the urethral wall, can cause hydronephrosis and hydroureter in the pregnant woman. Urinary tract infections, urinary incontinence and nocturia are common in pregnancy. All changes that occur during this period return to the previous state up to 6 weeks after birth
[5][13].
Additionally, during pregnancy, plasma volume increases by up to 50% and erythrocyte volume by up to 30%. These significant changes can lead to physiological anemia and decreased hematocrit, an effect that reduces blood viscosity and resistance to blood flow. Regarding the number of leukocytes, they increase and can reach very high values during labor, which can often explain the severity of the infection; however, these values do not make the pregnant woman more prone to infections
[15][22]. In general, the concentration of platelets is maintained at normal values, but there are some cases in which their number decreases (gestational thrombocytopenia) due to the increase in plasma volume, which disappears after birth
[16][23]. Fibrinolytic and coagulation pathways also undergo changes, and venous stasis leads to an increased risk of thromboembolism, beginning in the first trimester of pregnancy and lasting up to 3 months after birth
[12][20].
In pregnant woman, high levels of estrogen stimulate the production of the thyroid-binding globulin, leading to an increase in the total levels of triiodothyronine (T3) and thyroxine (T4) by about 50%, while free T3 and T4 levels remain constant or slightly altered. It also increases the production of hormones by the adrenal glands. Low blood pressure and vascular resistance stimulate the renin–angiotensin–aldosterone system, resulting in an up to 10-fold increase in aldosterone at the end of the third trimester of pregnancy. Moreover, there is an increase in the level of cortisol and adrenocorticotropic hormone, a corticosteroid-binding globulin, which leads to a state of hypercortisol. On the other hand, the high levels of estradiol in pregnancy result in an increase in prolactin that induces growth in the pituitary gland
[1][12][14][1,2,20].
2. Musculoskeletal Changes
Over time, it has been observed that many physiological and anatomical changes occur in pregnant women that can affect the essential organs, but the most common are those at the musculoskeletal level. Weight gain, the enlargement of the uterus with a shift in the center of gravity and hormonal and vascular changes cause a number of musculoskeletal problems. Changing the center of gravity causes lumbar lordosis with the flexion of the neck and the drooping of the shoulders
[17][18][24,25].
Mechanical pressure, elevated progesterone and relaxin levels increase joint laxity and prepare a woman’s body for childbirth. Additionally, in pregnant women, fluid retention causes the compression of soft tissues. All these changes that occur make the pregnant woman susceptible to musculoskeletal disorders. Most pregnant women complain of musculoskeletal disorders, and some of them show signs of disability. The majority conditions have been described as spinal pain, pain in the upper and lower extremities, peripheral neuropathy and muscle cramps. In addition, carpal tunnel syndrome, which results from compression of the median nerve, is quite common in pregnant women
[11][12][19][19,20,26]. Major changes that occur in the body of pregnant women at different system level are shown in
Figure 1.
Figure 1.
The main physiological and anatomical changes of pregnancy. (↑—increase, ↓—decrease).
These musculoskeletal disorders cause disabilities and loss of work capacity in pregnant women
[20][27]. Pain during pregnancy can be of various causes and is not limited only to labor pain. The non-obstetric causes of pain in pregnancy are common, from acute conditions, such as infection or injury, to secondary pain from underlying medical conditions. Pregnancy manifests physiological effects on a woman’s body, likewise influencing the endocrine, cardiovascular and renal systems as well as the musculoskeletal system. Additionally, weight gain during pregnancy and the presence of the pregnant uterus put pressure on the skeletal system. During the nine months of pregnancy, various changes occur in the body. These physiological and anatomical changes precipitate the onset of pain or may exacerbate pre-existing painful disorders.
Next, some aspects of the main imaging investigations for the diagnosis of musculoskeletal disorders will be presented.
X-rays are among the oldest types of imaging available, which use electromagnetic waves to produce an image. Bone lesions can be highlighted by radiography, but in order to diagnose muscle disorders more advanced imaging explorations are needed. The possibility that an X-ray taken during pregnancy will produce serious effects on the fetus is very small. However, the risk of affecting the child depends on the amount of radiation exposure and its gestational age. Thus, the exposure to high doses of radiation in the first two weeks after conception can cause a miscarriage; exposure up to eight weeks can increase the risk of congenital malformations; and up to week 16, high doses of radiation can lead to intellectual disability. The dose of a single exposure to radiation is far lesser than the doses associated with these risks. Another method of diagnosing musculoskeletal disorders is computed tomography (CT), which investigates bone and muscle injuries. This method offers a more detailed examination of body compared to radiography. It is not proven that the fetus is affected by the amount of radiation used in CT. However, its use on the abdomen or pelvic area is to be avoided in order to exclude any risk of developing cancer in childhood. If the examination of both the mother and the fetus is necessary, other imaging tests, such as ultrasound or magnetic resonance imaging (MRI), are used. Ultrasound uses sound waves to photograph the inside of the body. Ultrasound captures images of soft tissues, muscles and ligaments and can also diagnose musculoskeletal conditions along with MRI. Ultrasound can easily detect the signs of inflammation at the muscle and joint level. This imaging method is the most used for pregnant women, but if the images obtained do not provide a clear answer, an MRI examination can be resorted to. MRI is a method that uses radio waves and magnetic fields to capture images of the inside of the body. MRI can capture images of the body’s soft tissues, even muscles, unlike X-ray imaging. In addition, MRI can capture joint injuries, such as torn ligaments or cartilage. There are no proven adverse effects due to the MRI either in the pregnant woman nor in the fetus, and is a frequently used method today
[21][22][28,29].
The main musculoskeletal pains encountered during pregnancy can be classified into lumbar, pelvic and joint pain.
2.1. Lower Back Pain
Lower back pain occurs in about half of pregnant women and is considered a normal pain during pregnancy
[23][30]. A higher risk of lower back pain is associated with age, the presence of pain before pregnancy and especially during menstruation, and ethnicity, particularly in African American and Caucasian individuals; although individuals of Hispanic ethnicity do not show strong associations with lower back pain during pregnancy, nor do factors such as caffeine, tobacco, oral contraceptive medication, parity and exercise
[24][25][31,32]. Additionally, other factors that can contribute to lower back pain are the mechanical compressions of the pregnant uterus that modifies the center of gravity and increases the force applied to the spine, as well as the pelvic ligament laxity and vascular compression.
In addition, lower back pain encountered at night during pregnancy may be due to venous engorgement in the pelvis. The growing uterus presses on the vena cava and combined with fluid retention in pregnancy causes venous congestion and hypoxia in the lumbar spine
[26][33]. Some women experience this pain from the first trimester when the mechanical pressure is not high, in this case the hormonal level being the factor that influences the appearance of the musculoskeletal disorder
[24][31]. Most women recover easily in the first months after birth, of which only 50% seek professional medical assistance. The rapid identification of pain and the application of specific methods of treatment according to the particularities of each individual ultimately leads to total recovery. However, pregnant women who have gained more weight have a higher risk of postpartum lower back pain
[27][34].
The most affected musculoskeletal structures during pregnancy and postpartum are the pubic symphysis and the sacroiliac joints. Most of the time it is difficult to establish the exact cause of the pain based only on the anamnesis, and detailed imaging investigations are required. Non-inflammatory causes of back pain, such as mechanical stress on the pelvic area caused by pregnancy, can cause subchondral bone marrow edema that cannot be differentiated from axial spondyloarthritis
[28][35].
Bone marrow edema (BME) is a condition encountered in radiology described as a nonspecific lesion pattern, characterized by a change in marrow signal intensity at the level of the femoral head suggesting marrow infiltration through interstitial edema. Many aspects can lead to bone marrow changes, especially at the level of the sacroiliac joints, it is not yet clear whether postpartum bone marrow changes, which are mechanically induced, are different from inflammatory sacroiliitis seen on MRI. From an imaging point of view, spondyloarthropathy is characterized by BME around the sacroiliac joint (sacroiliitis) and structural changes, such as the fatty replacement of the bone marrow at the sites of inflammation, subchondral erosions and sclerosis
[29][36].
The scientific team led by Agten compared the MRI results of the sacroiliac joints subjected to mechanical stress due to pregnancy with those of a group of women known to have spondyloarthritis to make the differential diagnosis. It was found that mechanical pressure on the joints can lead to bone marrow edema, only inflammatory changes being present, while in the group with spondyloarthritis, structural changes and erosions were also evident. Thus, these findings may provide guidance to differentiate mechanically- and hormonally-induced bone marrow changes and inflammatory sacroiliitis
[30][37].
2.2. Pelvic Pain
Pelvic pain is described by pregnant women as a burning sensation, stabbing in the sacral area or as pain in the pubic symphysis. This pain may radiate to the groin or posterior thigh. The first symptoms appear during week 18 and reach a maximum intensity in week 36
[31][38]. Pelvic girdle pains are not pains that normally occur in pregnancy, so it is necessary to intervene as soon as possible in their treatment, otherwise they can lead to severe pain. If timely therapeutic measures are taken, recovery is rapid. Up to 22% of pregnant women may suffer from pelvic pain and up to 8% may experience severe symptoms
[32][39]. The causes of pelvic pain in pregnancy are multifactorial. Increased movement of the pelvic girdle causes pain due to increased ligament laxity caused by high levels of relaxin and estrogen. These high concentrations of hormones lead to enlargement of the pubic symphysis, which results in pain due to the increased mobility of the joints. Pelvic pain is amplified by mechanical exertion, anterior back pain or anterior pelvic trauma
[19][33][26,40].
Furthermore, it has been shown that high body mass index, multiparity, mental stress, physical exhaustion and smoking are factors that can accelerate the onset of pelvic pain in pregnancy
[34][41].
Lumbar disc herniation is considered the most common pathology of the spine in pregnant women; however, the condition is very rare in pregnant women compared to pelvic pain, with an estimated occurrence of 1 in 10,000 women. In recent years, an increase in the average age of women who become pregnant has been observed, a consideration that may increase the incidence of lumbar disc herniation among pregnant women. The most frequent symptoms were represented by radicular pain, along with the weakness of the muscles innervated by the root of a spinal nerve, the reduced sensation in the sensory distribution of a spinal nerve but also urinary incontinence. According to data from the literature, no more than 15% of patients suffering from this disorder develop severe neurological deficits. In terms of therapeutic management, it has been observed that the majority of lumbar disc herniation sufferers do not require surgery
[35][42].
2.3. Joint Pain
Pregnant women may experience joint pain, which often raises the suspicion of inflammatory diseases, such as rheumatoid arthritis or systemic lupus erythematosus. However, the development of new-onset inflammatory arthritis is rare during pregnancy, and there is evidence that pregnancy protects against new-onset rheumatoid arthritis
[36][43]. Soft tissue swelling as well as joint laxity are physiological changes considered predisposing factors for the development of joint pain. In addition, hormonal changes with increased levels of progesterone, estrogen, relaxin and cortisol are associated with joint symptoms, stiffness and even arthralgia
[37][44]. A study by Choi et al. aimed to establish the incidence of arthritis and arthralgia among pregnant women. Thus, of the 155 healthy pregnant women in the study, 9% developed arthritis and 16% had arthralgia. These conditions intensified in the third trimester of pregnancy, but the prognosis was generally good, with most of the disorders improving rapidly, concluding that the proximal interphalangeal joint of the hand was the most affected
[38][45].
Another common condition is carpal tunnel syndrome, which occurs in the third trimester of pregnancy and affects the wrist. Due to water retention during pregnancy, the median nerve is subject to high compression. The symptoms are characterized by pain, paresthesia and tingling in the distribution area of the median nerve, which intensify after repeated movements and during the night
[39][46]. Carpal tunnel syndrome developed in pregnancy has a benign course, most symptoms disappear after birth. However, a study of 45 pregnant women found that 49% still had symptoms 3 years postpartum
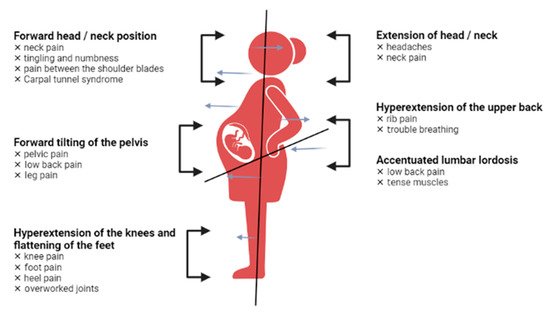
[40][47]. Pregnant women undergo changes in every part of the body, and
Figure 2 presents the most representative changes in terms of posture.
Figure 2.
Postural changes in pregnant women.