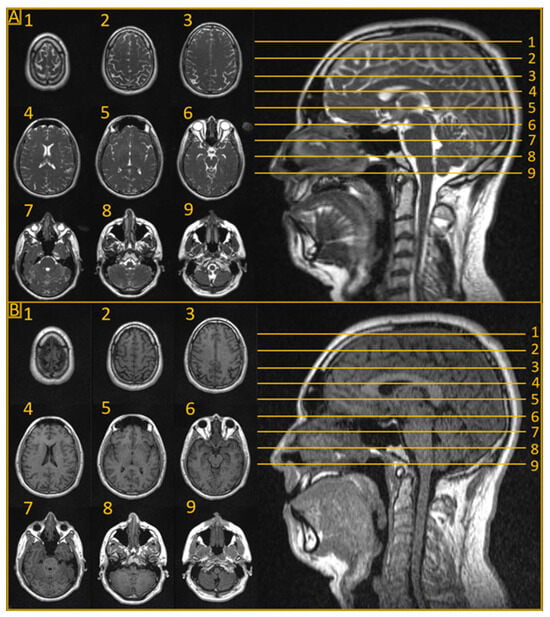
Magnetic resonance imaging (MRI) provides excellent visualization of central nervous system (CNS) tumors due to its superior soft tissue contrast. Magnetic resonance-guided radiotherapy (MRgRT) has historically been limited to use in the initial treatment planning stage due to cost and feasibility. MRI-guided linear accelerators (MRLs) allow clinicians to visualize tumors and organs at risk (OARs) directly before and during treatment, a process known as online MRgRT. This novel system permits adaptive treatment planning based on anatomical changes to ensure accurate dose delivery to the tumor while minimizing unnecessary toxicity to healthy tissue. These advancements are critical to treatment adaptation in the brain and spinal cord, where both preliminary MRI and daily computerized tomography (CT) guidance have typically had limited benefit.
- radiation therapy
- RT
- ultra-hypofractionated radiation therapy
- ablative radiation therapy
- adaptive radiation therapy
- image-guided radiotherapy
- magnetic resonance imaging
- MRI
1. Introduction
2. Clinical Applications
2.1. Glioblastoma
2.2. Stereotactic Radiation Therapy for Intracranial Tumors
SRT is an important modality in the management of brain metastases and other intracranial tumors [45][21]. An MRL offers several advantages over conventional linear accelerators, including enhanced target delineation, real-time tumor tracking, and adaptive treatment planning [10]. The superior soft-tissue contrast provided by MRI allows for improved identification of tumor boundaries, while real-time imaging enables accurate monitoring of tumor motion during treatment, potentially reducing unnecessary radiation exposure to healthy brain tissue [46][22]. Several studies have explored the dosimetric feasibility of MRgRT for intracranial SRT [16,17,18,19,20][23][24][25][26][27]. One early study investigated the dosimetric feasibility of MRL for brain metastases and the impact of the magnetic field, concluding that MRL-generated stereotactic radiation plans meeting clinical requirements were feasible, and that the dosimetric impact of the magnetic field, including the electron return effect (ERE) at tissue–air boundaries, was minor and did not negatively affect target conformity or dose gradient [16][23]. Another study evaluated the systematic localization accuracy, treatment planning capability, and delivery accuracy of an MRL platform for stereotactic radiosurgery (SRS), finding that excellent plan quality and delivery accuracy was achievable for concurrent treatment of multiple brain metastases with a single isocenter [17][24]. Collectively, the above studies indicate that MRgRT using an MRL has the potential to offer dosimetric and logistical advantages over conventional linear accelerators for intracranial SRT treatment. However, further clinical investigations are necessary to evaluate the clinical benefit of this technology.2.3. Stereotactic Radiation Therapy for Spine Tumors
Spine SRT plays a critical role in managing metastatic disease by alleviating pain, preventing pathological fractures, and reducing neurological morbidity. Stereotactic body radiotherapy (SBRT) has been shown to provide improved efficacy compared with conventional radiotherapy methods [50][28]. For spine SBRT, fusion with either a planning MRI or CT myelogram is necessary to accurately delineate the spinal cord and establish a 1–2 mm planning organ-at-risk volume (PRV), potentially reducing disease coverage [51][29]. CTgRT relies on bony structures for daily setup; however, it cannot visualize the spinal cord, leading to the requirement of a cord PRV for daily motion management. MRLs offer several advantages over CTgRT, including MR imaging in treatment position to allow for easier fusion with the planning CT and superior spinal cord delineation during setup compared with cone-beam CT (CBCT) [21,23][30][31]. Dosimetric feasibility studies indicate that daily MRgRT can lower the dose to the spinal cord [22][32]. MRLs enable daily direct registration to the spinal cord, eliminating the need for cord PRVs while also allowing for improved tumor coverage with reduced margin size. In addition, low-field MRLs suffer from less image distortion from implanted metallic devices [52][33]. MRI protocols outside of the radiation oncology department can often create challenges to performing an accurate fusion due to differences in slice thicknesses and patient positions [53][34]; simulation and treatment planning using MRLs may address these issues [23][31]. These advantages increase the therapeutic ratio and may allow for dose escalation.2.4. Hippocampal Avoidance Whole Brain Radiotherapy
HA-WBRT is a promising technique that aims to achieve the local control benefits of whole brain RT for both macro- and micro-metastatic lesions, while reducing neurotoxicity by specifically avoiding the hippocampus [54][35]. HA-WBRT requires fusion of a planning MRI with CT simulation imaging to create a hippocampal avoidance structure, while ensuring a homogenous treatment plan for the remaining brain parenchyma [55][36]. HA-WBRT using MRgRT could facilitate adaptive treatment based on the intra-therapeutic tumor response, potentially improving the local control probability with sequential stereotactic boosts to nonresponding lesions. A dosimetric feasibility study compared twelve HA-WBRT volumetric modulated arc therapy (VMAT) plans versus intensity modulated radiation therapy (IMRT) plans created using the 0.35 T MRL treatment planning system (TPS) [27][37]. In all cases, the researchers were able to generate plans that met RTOG 0933 treatment plan standards. As anticipated, the VMAT plans exhibited superior homogeneity and delivery times compared with the IMRT plans. Particularly for patients with numerous brain metastases of radioresistant histology, HA-WBRT with a simultaneous integrated boost to gross disease may be an effective strategy [14[14][38],56], one that may be further facilitated using MRgRT. Additional investigation through clinical trials is necessary to determine the clinical feasibility and safety of HA-WBRT. This approach could optimize the balance between effective tumor control and minimizing neurotoxicity for patients undergoing whole brain radiotherapy.3. Summary
One of the fundamental goals of radiotherapy is maximizing the dose to target tissue while minimizing the dose to surrounding OARs. In a significant first step towards this aim, MRLs have facilitated treatment plan adaptation to observable anatomic changes throughout therapy. MRLs, however, may be able to enable biological plan adaptation by leveraging MRI’s capability to track biological and physiological changes through advanced mpMRI techniques. These techniques may allow radiation oncologists further insight into a tumor’s biology as it responds to RT over the course of treatment. The treatment paradigm of radiotherapy has traditionally been based on empirical large cohort data rather than individual biology, resulting in a one-size-fits-all approach. However, recent advancements in genomics and radiomics have begun to pave the way towards a more personalized approach based upon individual tumor biology. The synergy between genomically informed radiotherapy, treatment of high-risk sub-volumes based on extraction of radiographic data, and daily mpMRI-guided plan adaptation has the potential to usher in a new treatment paradigm in radiation oncology. Pre-treatment genomic and radiomic analyses of the tumor may improve patient selection for MRL-based dose escalation [30,57,58][39][40][41]. Daily mpMRI delta radiomic analysis can then be used to detect subtle biomarkers of treatment response in tumors, which hint at radiation-induced genomic plasticity, thereby allowing for even greater personalized adaptive treatment strategies [59,60,61,62][42][43][44][45]. The currently active phase II Habitat Escalated Adaptive Therapy (HEAT), With Neoadjuvant Radiation for Soft Tissue Sarcoma (NCT05301283) is an example of a cutting-edge study utilizing genomic and mpMRI radiomic biomarkers to guide the initial treatment and adaptive treatment approach for high-grade soft tissue sarcomas. Utilizing a similar approach for CNS tumors appears to be technically feasible currently. For example, genomic-adjusted radiation therapy (GARD) could be similarly utilized to identify GBM patients who could benefit from higher doses [63][46] with MRI perfusion [64][47] and FLAIR [65,66][48][49] sequences, which could identify tumor subpopulations to target with simultaneous integrated boosts. MRL is poised to take a central role at the forefront of this paradigm shift to allow for plan adaptation based not only upon geometric shifts but also on a tumor’s evolving treatment response throughout therapy. An ultra-personalized treatment approach like this allows for total dose, dose distribution (i.e., dose painting), and fractionation changes throughout the course of therapy to improve clinical outcomes for patients.Radiomic- and Genomic-Guided Adaptive Radiation Therapy for CNS Tumors
Historically, daily MRgRT plan adaptation has been utilized to manage interfractional geometric changes. However, MRI is also capable of assessing biological and physiological information using advanced mpMRI techniques [28,67,68,69][50][51][52][53]. These techniques have the potential to be particularly beneficial for CNS tumors treated on an MRL. One such technique is diffusion-weighted imaging (DWI), which enables the detection of water mobility changes [70][54]. These alterations are associated with tumor growth [71][55] or necrosis [72][56]. By mapping a parameter known as the apparent diffusion coefficient (ADC), clinicians can monitor the response to radiation therapy [73][57]. ADC mapping is especially appealing in adaptive radiotherapy, as changes in ADC can be observed before morphological alterations in the tumor [74][58]. This feature could guide dose escalation strategies or biologically driven radiation plan adaptation [58,75][41][59]. DWI has been applied on a 1.5 T MRI-guided linear accelerator [76,77,78][60][61][62] and on a 0.35 T tri-cobalt system [79,80][63][64]. Dynamic contrast-enhanced (DCE) MRI is another functional imaging technique that investigates perfusion by dynamically evaluating changes in the T1 relaxation time following a bolus injection of gadolinium [82,83][65][66]. This process allows for the examination of gadolinium transport across the capillary endothelium [68][52]. DCE has demonstrated prognostic value in identifying patient subpopulations with hypoxia-related resistance to chemoradiation in cervical cancer [84][67]. As a result, DCE has the potential to provide information that may aid in personalizing radiation dose delivery for CNS tumors [77][61]. DCE has been implemented on the 1.5 T MRL, although its quantification was shown to be less reproducible than that of T1, T2, and ADC [76][60]. While DCE has not yet been implemented on a 0.35 T MRL, initial experiences have demonstrated the feasibility of gadolinium injection on the tri-cobalt version of this system [85][68]. Additional MR-based techniques, such as magnetic resonance spectroscopic imaging (MRSI) [86][69], chemical exchange saturation transfer (CEST) [87,88][70][71], and hyperpolarized dynamic magnetic resonance spectroscopy [89][72], can interrogate metabolic processes in tumors [90][73]. These techniques could potentially offer valuable information for the adaptive radiotherapy of CNS tumors on an MRL. MRSI has been applied to create high-resolution metabolite maps in gliomas [91][74] and to map lactate in GBM [92][75]. Genomics provides another powerful avenue towards personalized radiation treatment, which when combined with the advances in image guidance listed above, may provide an even more sophisticated approach for challenging malignancies such as GBM. Several such signatures have been introduced as a potential means for genomically guided RT [57,63,106,107,108,109,110][40][46][76][77][78][79][80]. Genomics offers a biological framework for guiding RT, giving better context to the radiomic changes observed during treatment, and fostering research into predictive biomarkers. This combination may allow for novel advanced and better-informed approaches to dose escalation in high-grade glioma, a strategy which has been largely unsuccessful in the past [111,112,113,114][81][82][83][84]. In summary, MRL can be leveraged by incorporating genomically guided RT and mpMRI radiomics to enable a biologically adaptive RT paradigm. Various mpMRI techniques, including DWI, DCE, MRSI, and CEST, have the potential to offer valuable insights into tumor biology and physiology, ultimately leading to more personalized and effective treatment strategies. Using these technologies to identify intratumoral heterogeneity and tumoral sub-volumes at risk may allow for focal dose escalation or avoidance, respectively. As research and development continues in this area, we expect significant advancements in the application of these techniques, potentially revolutionizing the management of CNS tumors.References
- Ostrom, Q.T.; Gittleman, H.; Truitt, G.; Boscia, A.; Kruchko, C.; Barnholtz-Sloan, J.S. CBTRUS Statistical Report: Primary Brain and Other Central Nervous System Tumors Diagnosed in the United States in 2011–2015. Neuro. Oncol. 2018, 20 (Suppl. S4), iv1–iv86.
- Bogdanov, A., Jr.; Mazzanti, M.L. Molecular magnetic resonance contrast agents for the detection of cancer: Past and present. Semin. Oncol. 2011, 38, 42–54.
- Jena, R.; Price, S.J.; Baker, C.; Jefferies, S.J.; Pickard, J.D.; Gillard, J.H.; Burnet, N.G. Diffusion tensor imaging: Possible implications for radiotherapy treatment planning of patients with high-grade glioma. Clin. Oncol. 2005, 17, 581–590.
- Paulson, E.S.; Schmainda, K.M. Comparison of dynamic susceptibility-weighted contrast-enhanced MR methods: Recommendations for measuring relative cerebral blood volume in brain tumors. Radiology 2008, 249, 601–613.
- Lagendijk, J.J.; Raaymakers, B.W.; van Vulpen, M. The magnetic resonance imaging-linac system. Semin. Radiat. Oncol. 2014, 24, 207–209.
- Mutic, S.; Dempsey, J.F. The ViewRay system: Magnetic resonance-guided and controlled radiotherapy. Semin. Radiat. Oncol. 2014, 24, 196–199.
- Keall, P.J.; Barton, M.; Crozier, S.; Australian MRI-Linac Program, including contributors from the Ingham Institute, Illawarra Cancer Care Centre, Liverpool Hospital, Stanford University, Universities of Newcastle, Queensland, Sydney, Western Sydney, and Wollongong. The Australian magnetic resonance imaging-linac program. Semin. Radiat. Oncol. 2014, 24, 203–206.
- Raaymakers, B.W.; Jurgenliemk-Schulz, I.M.; Bol, G.H.; Glitzner, M.; Kotte, A.; van Asselen, B.; de Boer, J.C.J.; Bluemink, J.J.; Hackett, S.L.; Moerland, M.A.; et al. First patients treated with a 1.5 T MRI-Linac: Clinical proof of concept of a high-precision, high-field MRI guided radiotherapy treatment. Phys. Med. Biol. 2017, 62, L41–L50.
- Finazzi, T.; Palacios, M.A.; Spoelstra, F.O.B.; Haasbeek, C.J.A.; Bruynzeel, A.M.E.; Slotman, B.J.; Lagerwaard, F.J.; Senan, S. Role of On-Table Plan Adaptation in MR-Guided Ablative Radiation Therapy for Central Lung Tumors. Int. J. Radiat. Oncol. Biol. Phys. 2019, 104, 933–941.
- Bryant, J.M.; Weygand, J.; Keit, E.; Cruz-Chamorro, R.; Sandoval, M.L.; Oraiqat, I.M.; Andreozzi, J.; Redler, G.; Latifi, K.; Feygelman, V.; et al. Stereotactic Magnetic Resonance-Guided Adaptive and Non-Adaptive Radiotherapy on Combination MR-Linear Accelerators: Current Practice and Future Directions. Cancers 2023, 15, 2081.
- Chin, S.; Eccles, C.L.; McWilliam, A.; Chuter, R.; Walker, E.; Whitehurst, P.; Berresford, J.; Van Herk, M.; Hoskin, P.J.; Choudhury, A. Magnetic resonance-guided radiation therapy: A review. J. Med. Imaging Radiat. Oncol. 2020, 64, 163–177.
- Kluter, S. Technical design and concept of a 0.35 T MR-Linac. Clin. Transl. Radiat. Oncol. 2019, 18, 98–101.
- Raaymakers, B.W.; Lagendijk, J.J.; Overweg, J.; Kok, J.G.; Raaijmakers, A.J.; Kerkhof, E.M.; van der Put, R.W.; Meijsing, I.; Crijns, S.P.; Benedosso, F.; et al. Integrating a 1.5 T MRI scanner with a 6 MV accelerator: Proof of concept. Phys. Med. Biol. 2009, 54, N229–N237.
- Scheffler, K.; Lehnhardt, S. Principles and applications of balanced SSFP techniques. Eur. Radiol. 2003, 13, 2409–2418.
- Cabrera, A.R.; Kirkpatrick, J.P.; Fiveash, J.B.; Shih, H.A.; Koay, E.J.; Lutz, S.; Petit, J.; Chao, S.T.; Brown, P.D.; Vogelbaum, M.; et al. Radiation therapy for glioblastoma: Executive summary of an American Society for Radiation Oncology Evidence-Based Clinical Practice Guideline. Pract. Radiat. Oncol. 2016, 6, 217–225.
- Burger, P.C.; Dubois, P.J.; Schold, S.C., Jr.; Smith, K.R., Jr.; Odom, G.L.; Crafts, D.C.; Giangaspero, F. Computerized tomographic and pathologic studies of the untreated, quiescent, and recurrent glioblastoma multiforme. J. Neurosurg. 1983, 58, 159–169.
- Earnest, F.t.; Kelly, P.J.; Scheithauer, B.W.; Kall, B.A.; Cascino, T.L.; Ehman, R.L.; Forbes, G.S.; Axley, P.L. Cerebral astrocytomas: Histopathologic correlation of MR and CT contrast enhancement with stereotactic biopsy. Radiology 1988, 166, 823–827.
- Champ, C.E.; Siglin, J.; Mishra, M.V.; Shen, X.; Werner-Wasik, M.; Andrews, D.W.; Mayekar, S.U.; Liu, H.; Shi, W. Evaluating changes in radiation treatment volumes from post-operative to same-day planning MRI in High-grade gliomas. Radiat. Oncol. 2012, 7, 220.
- Yang, Z.; Zhang, Z.; Wang, X.; Hu, Y.; Lyu, Z.; Huo, L.; Wei, R.; Fu, J.; Hong, J. Intensity-modulated radiotherapy for gliomas:dosimetric effects of changes in gross tumor volume on organs at risk and healthy brain tissue. OncoTargets Ther. 2016, 9, 3545–3554.
- Stewart, J.; Sahgal, A.; Lee, Y.; Soliman, H.; Tseng, C.L.; Detsky, J.; Husain, Z.; Ho, L.; Das, S.; Maralani, P.J.; et al. Quantitating Interfraction Target Dynamics during Concurrent Chemoradiation for Glioblastoma: A Prospective Serial Imaging Study. Int. J. Radiat. Oncol. Biol. Phys. 2021, 109, 736–746.
- Chin, L.S.; Regine, W.F. Principles and Practice of Stereotactic Radiosurgery, 2nd ed.; Springer: New York, NY, USA, 2014.
- Derks, S.; van der Veldt, A.A.M.; Smits, M. Brain metastases: The role of clinical imaging. Br. J. Radiol. 2022, 95, 20210944.
- Tseng, C.L.; Eppinga, W.; Seravalli, E.; Hackett, S.; Brand, E.; Ruschin, M.; Lee, Y.K.; Atenafu, E.G.; Sahgal, A. Dosimetric feasibility of the hybrid Magnetic Resonance Imaging (MRI)-linac System (MRL) for brain metastases: The impact of the magnetic field. Radiother. Oncol. 2017, 125, 273–279.
- Wen, N.; Kim, J.; Doemer, A.; Glide-Hurst, C.; Chetty, I.J.; Liu, C.; Laugeman, E.; Xhaferllari, I.; Kumarasiri, A.; Victoria, J.; et al. Evaluation of a magnetic resonance guided linear accelerator for stereotactic radiosurgery treatment. Radiother. Oncol. 2018, 127, 460–466.
- Slagowski, J.M.; Redler, G.; Malin, M.J.; Cammin, J.; Lobb, E.C.; Lee, B.H.; Sethi, A.; Roeske, J.C.; Flores-Martinez, E.; Stevens, T.; et al. Dosimetric feasibility of brain stereotactic radiosurgery with a 0.35 T MRI-guided linac and comparison vs a C-arm-mounted linac. Med. Phys. 2020, 47, 5455–5466.
- Seravalli, E.; Sierts, M.; Brand, E.; Maspero, M.; David, S.; Philippens, M.E.P.; Voormolen, E.H.J.; Verhoeff, J.J.C. Dosimetric feasibility of direct post-operative MR-Linac-based stereotactic radiosurgery for resection cavities of brain metastases. Radiother. Oncol. 2023, 179, 109456.
- Tan, H.; Stewart, J.; Ruschin, M.; Wang, M.H.; Myrehaug, S.; Tseng, C.L.; Detsky, J.; Husain, Z.; Chen, H.; Sahgal, A.; et al. Inter-fraction dynamics during post-operative 5 fraction cavity hypofractionated stereotactic radiotherapy with a MR LINAC: A prospective serial imaging study. J. Neuro-Oncol. 2022, 156, 569–577.
- Sahgal, A.; Myrehaug, S.D.; Siva, S.; Masucci, G.L.; Maralani, P.J.; Brundage, M.; Butler, J.; Chow, E.; Fehlings, M.G.; Foote, M.; et al. Stereotactic body radiotherapy versus conventional external beam radiotherapy in patients with painful spinal metastases: An open-label, multicentre, randomised, controlled, phase 2/3 trial. Lancet Oncol. 2021, 22, 1023–1033.
- Redmond, K.J.; Robertson, S.; Lo, S.S.; Soltys, S.G.; Ryu, S.; McNutt, T.; Chao, S.T.; Yamada, Y.; Ghia, A.; Chang, E.L.; et al. Consensus Contouring Guidelines for Postoperative Stereotactic Body Radiation Therapy for Metastatic Solid Tumor Malignancies to the Spine. Int. J. Radiat. Oncol. Biol. Phys. 2017, 97, 64–74.
- Noel, C.E.; Parikh, P.J.; Spencer, C.R.; Green, O.L.; Hu, Y.; Mutic, S.; Olsen, J.R. Comparison of onboard low-field magnetic resonance imaging versus onboard computed tomography for anatomy visualization in radiotherapy. Acta Oncol. 2015, 54, 1474–1482.
- Spieler, B.; Samuels, S.E.; Llorente, R.; Yechieli, R.; Ford, J.C.; Mellon, E.A. Advantages of Radiation Therapy Simulation with 0.35 Tesla Magnetic Resonance Imaging for Stereotactic Ablation of Spinal Metastases. Pract. Radiat. Oncol. 2020, 10, 339–344.
- Redler, G.; Stevens, T.; Cammin, J.; Malin, M.; Green, O.; Mutic, S.; Pitroda, S.; Aydogan, B. Dosimetric Feasibility of Utilizing the ViewRay Magnetic Resonance Guided Linac System for Image-guided Spine Stereotactic Body Radiation Therapy. Cureus 2019, 11, e6364.
- Stradiotti, P.; Curti, A.; Castellazzi, G.; Zerbi, A. Metal-related artifacts in instrumented spine. Techniques for reducing artifacts in CT and MRI: State of the art. Eur. Spine J. 2009, 18 (Suppl. S1), 102–108.
- Paulson, E.S.; Erickson, B.; Schultz, C.; Allen Li, X. Comprehensive MRI simulation methodology using a dedicated MRI scanner in radiation oncology for external beam radiation treatment planning. Med. Phys. 2015, 42, 28–39.
- Caine, C.; Deshmukh, S.; Gondi, V.; Mehta, M.; Tome, W.; Corn, B.W.; Kanner, A.; Rowley, H.; Kundapur, V.; DeNittis, A.; et al. CogState computerized memory tests in patients with brain metastases: Secondary endpoint results of NRG Oncology RTOG 0933. J. Neurooncol. 2016, 126, 327–336.
- Andreas, J.J.M.; Kundapur, V. Hippocampus Avoidance Whole-brain Radiation Therapy: A Practical Intensity-modulated Radiation Therapy Planning and Delivery Approach to RTOG 0933. J. Med. Imaging Radiat. Sci. 2015, 46, 78–84.
- Graham, J.A.; Redler, G.; Delozier, K.B.; Yu, H.M.; Oliver, D.E.; Rosenberg, S.A. Dosimetric feasibility of hippocampal avoidance whole brain radiotherapy with an MRI-guided linear accelerator. J. Appl. Clin. Med. Phys. 2022, 23, e13587.
- Popp, I.; Grosu, A.L.; Fennell, J.T.; Fischer, M.; Baltas, D.; Wiehle, R. Optimization of hippocampus sparing during whole brain radiation therapy with simultaneous integrated boost-tutorial and efficacy of complete directional hippocampal blocking. Strahlenther. Onkol. 2022, 198, 537–546.
- Scott, J.G.; Sedor, G.; Ellsworth, P.; Scarborough, J.A.; Ahmed, K.A.; Oliver, D.E.; Eschrich, S.A.; Kattan, M.W.; Torres-Roca, J.F. Pan-cancer prediction of radiotherapy benefit using genomic-adjusted radiation dose (GARD): A cohort-based pooled analysis. Lancet Oncol. 2021, 22, 1221–1229.
- Scott, J.G.; Berglund, A.; Schell, M.J.; Mihaylov, I.; Fulp, W.J.; Yue, B.; Welsh, E.; Caudell, J.J.; Ahmed, K.; Strom, T.S.; et al. A genome-based model for adjusting radiotherapy dose (GARD): A retrospective, cohort-based study. Lancet Oncol. 2017, 18, 202–211.
- Park, J.E.; Kim, H.S.; Jo, Y.; Yoo, R.E.; Choi, S.H.; Nam, S.J.; Kim, J.H. Radiomics prognostication model in glioblastoma using diffusion- and perfusion-weighted MRI. Sci. Rep. 2020, 10, 4250.
- Gillies, R.J.; Kinahan, P.E.; Hricak, H. Radiomics: Images Are More than Pictures, They Are Data. Radiology 2016, 278, 563–577.
- Kocher, M.; Ruge, M.I.; Galldiks, N.; Lohmann, P. Applications of radiomics and machine learning for radiotherapy of malignant brain tumors. Strahlenther. Onkol. 2020, 196, 856–867.
- Nardone, V.; Reginelli, A.; Grassi, R.; Boldrini, L.; Vacca, G.; D’Ippolito, E.; Annunziata, S.; Farchione, A.; Belfiore, M.P.; Desideri, I.; et al. Delta radiomics: A systematic review. Radiol. Med. 2021, 126, 1571–1583.
- Persi, E.; Wolf, Y.I.; Horn, D.; Ruppin, E.; Demichelis, F.; Gatenby, R.A.; Gillies, R.J.; Koonin, E.V. Mutation-selection balance and compensatory mechanisms in tumour evolution. Nat. Rev. Genet. 2021, 22, 251–262.
- Ahmed, K.A.; Chinnaiyan, P.; Fulp, W.J.; Eschrich, S.; Torres-Roca, J.F.; Caudell, J.J. The radiosensitivity index predicts for overall survival in glioblastoma. Oncotarget 2015, 6, 34414–34422.
- Cao, Y.; Tsien, C.I.; Nagesh, V.; Junck, L.; Ten Haken, R.; Ross, B.D.; Chenevert, T.L.; Lawrence, T.S. Survival prediction in high-grade gliomas by MRI perfusion before and during early stage of RT . Int. J. Radiat. Oncol. Biol. Phys. 2006, 64, 876–885.
- Chang, P.D.; Chow, D.S.; Yang, P.H.; Filippi, C.G.; Lignelli, A. Predicting Glioblastoma Recurrence by Early Changes in the Apparent Diffusion Coefficient Value and Signal Intensity on FLAIR Images. AJR Am. J. Roentgenol. 2017, 208, 57–65.
- Rathore, S.; Akbari, H.; Doshi, J.; Shukla, G.; Rozycki, M.; Bilello, M.; Lustig, R.; Davatzikos, C. Radiomic signature of infiltration in peritumoral edema predicts subsequent recurrence in glioblastoma: Implications for personalized radiotherapy planning. J. Med. Imaging 2018, 5, 021219.
- Maziero, D.; Straza, M.W.; Ford, J.C.; Bovi, J.A.; Diwanji, T.; Stoyanova, R.; Paulson, E.S.; Mellon, E.A. MR-Guided Radiotherapy for Brain and Spine Tumors. Front. Oncol. 2021, 11, 626100.
- Wang, J.; Weygand, J.; Hwang, K.P.; Mohamed, A.S.; Ding, Y.; Fuller, C.D.; Lai, S.Y.; Frank, S.J.; Zhou, J. Magnetic Resonance Imaging of Glucose Uptake and Metabolism in Patients with Head and Neck Cancer. Sci. Rep. 2016, 6, 30618.
- Salzillo, T.C.; Mawoneke, V.; Weygand, J.; Shetty, A.; Gumin, J.; Zacharias, N.M.; Gammon, S.T.; Piwnica-Worms, D.; Fuller, G.N.; Logothetis, C.J.; et al. Measuring the Metabolic Evolution of Glioblastoma throughout Tumor Development, Regression, and Recurrence with Hyperpolarized Magnetic Resonance. Cells 2021, 10, 2621.
- Dutta, P.; Perez, M.R.; Lee, J.; Kang, Y.; Pratt, M.; Salzillo, T.C.; Weygand, J.; Zacharias, N.M.; Gammon, S.T.; Koay, E.J.; et al. Combining Hyperpolarized Real-Time Metabolic Imaging and NMR Spectroscopy To Identify Metabolic Biomarkers in Pancreatic Cancer. J. Proteome Res. 2019, 18, 2826–2834.
- Sugahara, T.; Korogi, Y.; Kochi, M.; Ikushima, I.; Shigematu, Y.; Hirai, T.; Okuda, T.; Liang, L.; Ge, Y.; Komohara, Y.; et al. Usefulness of diffusion-weighted MRI with echo-planar technique in the evaluation of cellularity in gliomas. J. Magn. Reson. Imaging 1999, 9, 53–60.
- Ellingson, B.M.; Malkin, M.G.; Rand, S.D.; Connelly, J.M.; Quinsey, C.; LaViolette, P.S.; Bedekar, D.P.; Schmainda, K.M. Validation of functional diffusion maps (fDMs) as a biomarker for human glioma cellularity. J. Magn. Reson. Imaging 2010, 31, 538–548.
- Hein, P.A.; Eskey, C.J.; Dunn, J.F.; Hug, E.B. Diffusion-weighted imaging in the follow-up of treated high-grade gliomas: Tumor recurrence versus radiation injury. AJNR Am. J. Neuroradiol. 2004, 25, 201–209.
- Decker, G.; Murtz, P.; Gieseke, J.; Traber, F.; Block, W.; Sprinkart, A.M.; Leitzen, C.; Buchstab, T.; Lutter, C.; Schuller, H.; et al. Intensity-modulated radiotherapy of the prostate: Dynamic ADC monitoring by DWI at 3.0 T. Radiother. Oncol. 2014, 113, 115–120.
- Bains, L.J.; Zweifel, M.; Thoeny, H.C. Therapy response with diffusion MRI: An update. Cancer Imaging 2012, 12, 395–402.
- McGarry, S.D.; Hurrell, S.L.; Kaczmarowski, A.L.; Cochran, E.J.; Connelly, J.; Rand, S.D.; Schmainda, K.M.; LaViolette, P.S. Magnetic Resonance Imaging-Based Radiomic Profiles Predict Patient Prognosis in Newly Diagnosed Glioblastoma before Therapy. Tomography 2016, 2, 223–228.
- Kooreman, E.S.; van Houdt, P.J.; Nowee, M.E.; van Pelt, V.W.J.; Tijssen, R.H.N.; Paulson, E.S.; Gurney-Champion, O.J.; Wang, J.; Koetsveld, F.; van Buuren, L.D.; et al. Feasibility and accuracy of quantitative imaging on a 1.5 T MR-linear accelerator. Radiother. Oncol. 2019, 133, 156–162.
- Thorwarth, D.; Ege, M.; Nachbar, M.; Monnich, D.; Gani, C.; Zips, D.; Boeke, S. Quantitative magnetic resonance imaging on hybrid magnetic resonance linear accelerators: Perspective on technical and clinical validation. Phys. Imaging Radiat. Oncol. 2020, 16, 69–73.
- Habrich, J.; Boeke, S.; Nachbar, M.; Nikolaou, K.; Schick, F.; Gani, C.; Zips, D.; Thorwarth, D. Repeatability of diffusion-weighted magnetic resonance imaging in head and neck cancer at a 1.5 T MR-Linac. Radiother. Oncol. 2022, 174, 141–148.
- Yang, Y.; Cao, M.; Sheng, K.; Gao, Y.; Chen, A.; Kamrava, M.; Lee, P.; Agazaryan, N.; Lamb, J.; Thomas, D.; et al. Longitudinal diffusion MRI for treatment response assessment: Preliminary experience using an MRI-guided tri-cobalt 60 radiotherapy system. Med. Phys. 2016, 43, 1369–1373.
- Shaverdian, N.; Yang, Y.; Hu, P.; Hart, S.; Sheng, K.; Lamb, J.; Cao, M.; Agazaryan, N.; Thomas, D.; Steinberg, M.; et al. Feasibility evaluation of diffusion-weighted imaging using an integrated MRI-radiotherapy system for response assessment to neoadjuvant therapy in rectal cancer. Br. J. Radiol. 2017, 90, 20160739.
- Tofts, P.S.; Kermode, A.G. Measurement of the blood-brain barrier permeability and leakage space using dynamic MR imaging. 1. Fundamental concepts. Magn. Reson. Med. 1991, 17, 357–367.
- Tofts, P.S.; Brix, G.; Buckley, D.L.; Evelhoch, J.L.; Henderson, E.; Knopp, M.V.; Larsson, H.B.; Lee, T.Y.; Mayr, N.A.; Parker, G.J.; et al. Estimating kinetic parameters from dynamic contrast-enhanced T(1)-weighted MRI of a diffusable tracer: Standardized quantities and symbols. J. Magn. Reson. Imaging 1999, 10, 223–232.
- Halle, C.; Andersen, E.; Lando, M.; Aarnes, E.K.; Hasvold, G.; Holden, M.; Syljuasen, R.G.; Sundfor, K.; Kristensen, G.B.; Holm, R.; et al. Hypoxia-induced gene expression in chemoradioresistant cervical cancer revealed by dynamic contrast-enhanced MRI. Cancer Res. 2012, 72, 5285–5295.
- Wojcieszynski, A.P.; Rosenberg, S.A.; Brower, J.V.; Hullett, C.R.; Geurts, M.W.; Labby, Z.E.; Hill, P.M.; Bayliss, R.A.; Paliwal, B.; Bayouth, J.E.; et al. Gadoxetate for direct tumor therapy and tracking with real-time MRI-guided stereotactic body radiation therapy of the liver. Radiother. Oncol. 2016, 118, 416–418.
- Posse, S.; Otazo, R.; Dager, S.R.; Alger, J. MR spectroscopic imaging: Principles and recent advances. J. Magn. Reson. Imaging 2013, 37, 1301–1325.
- van Zijl, P.C.; Yadav, N.N. Chemical exchange saturation transfer (CEST): What is in a name and what isn’t? Magn. Reson. Med. 2011, 65, 927–948.
- Wu, B.; Warnock, G.; Zaiss, M.; Lin, C.; Chen, M.; Zhou, Z.; Mu, L.; Nanz, D.; Tuura, R.; Delso, G. An overview of CEST MRI for non-MR physicists. EJNMMI Phys. 2016, 3, 19.
- Ardenkjaer-Larsen, J.H.; Fridlund, B.; Gram, A.; Hansson, G.; Hansson, L.; Lerche, M.H.; Servin, R.; Thaning, M.; Golman, K. Increase in signal-to-noise ratio of >10,000 times in liquid-state NMR. Proc. Natl. Acad. Sci. USA 2003, 100, 10158–10163.
- Weygand, J.; Carter, S.; Salzillo, T.; Moussalli, M.; Dai, B.; Zuo, X.; Flemming, J.; Shureiqi, I.; Bhattacharya, P. Can an Organoid Recapitulate the Metabolome of its Parent Tissue? A Pilot NMR Spectroscopy Study. J. Cancer Prev. Curr. Res. 2017, 8, 00307.
- Hangel, G.; Cadrien, C.; Lazen, P.; Furtner, J.; Lipka, A.; Heckova, E.; Hingerl, L.; Motyka, S.; Gruber, S.; Strasser, B.; et al. High-resolution metabolic imaging of high-grade gliomas using 7T-CRT-FID-MRSI. Neuroimage Clin. 2020, 28, 102433.
- De Feyter, H.M.; Behar, K.L.; Corbin, Z.A.; Fulbright, R.K.; Brown, P.B.; McIntyre, S.; Nixon, T.W.; Rothman, D.L.; de Graaf, R.A. Deuterium metabolic imaging (DMI) for MRI-based 3D mapping of metabolism in vivo. Sci. Adv. 2018, 4, eaat7314.
- Torres-Roca, J.F.; Eschrich, S.; Zhao, H.; Bloom, G.; Sung, J.; McCarthy, S.; Cantor, A.B.; Scuto, A.; Li, C.; Zhang, S.; et al. Prediction of radiation sensitivity using a gene expression classifier. Cancer Res. 2005, 65, 7169–7176.
- Speers, C.; Zhao, S.; Liu, M.; Bartelink, H.; Pierce, L.J.; Feng, F.Y. Development and Validation of a Novel Radiosensitivity Signature in Human Breast Cancer. Clin. Cancer Res. 2015, 21, 3667–3677.
- Sjöström, M.; Staaf, J.; Edén, P.; Wärnberg, F.; Bergh, J.; Malmström, P.; Fernö, M.; Niméus, E.; Fredriksson, I. Identification and validation of single-sample breast cancer radiosensitivity gene expression predictors. Breast Cancer Res. 2018, 20, 64.
- Ferrandon, S.; Saultier, P.; Carras, J.; Battiston-Montagne, P.; Alphonse, G.; Beuve, M.; Malleval, C.; Honnorat, J.; Slatter, T.; Hung, N.; et al. Telomere profiling: Toward glioblastoma personalized medicine. Mol. Neurobiol. 2013, 47, 64–76.
- Luxton, J.J.; McKenna, M.J.; Lewis, A.M.; Taylor, L.E.; Jhavar, S.G.; Swanson, G.P.; Bailey, S.M. Telomere Length Dynamics and Chromosomal Instability for Predicting Individual Radiosensitivity and Risk via Machine Learning. J. Pers. Med. 2021, 11, 188.
- Souhami, L.; Seiferheld, W.; Brachman, D.; Podgorsak, E.B.; Werner-Wasik, M.; Lustig, R.; Schultz, C.J.; Sause, W.; Okunieff, P.; Buckner, J.; et al. Randomized comparison of stereotactic radiosurgery followed by conventional radiotherapy with carmustine to conventional radiotherapy with carmustine for patients with glioblastoma multiforme: Report of Radiation Therapy Oncology Group 93-05 protocol. Int. J. Radiat. Oncol. Biol. Phys. 2004, 60, 853–860.
- Chan, J.L.; Lee, S.W.; Fraass, B.A.; Normolle, D.P.; Greenberg, H.S.; Junck, L.R.; Gebarski, S.S.; Sandler, H.M. Survival and failure patterns of high-grade gliomas after three-dimensional conformal radiotherapy. J. Clin. Oncol. 2002, 20, 1635–1642.
- Laperriere, N.J.; Leung, P.M.; McKenzie, S.; Milosevic, M.; Wong, S.; Glen, J.; Pintilie, M.; Bernstein, M. Randomized study of brachytherapy in the initial management of patients with malignant astrocytoma. Int. J. Radiat. Oncol. Biol. Phys. 1998, 41, 1005–1011.
- Selker, R.G.; Shapiro, W.R.; Burger, P.; Blackwood, M.S.; Arena, V.C.; Gilder, J.C.; Malkin, M.G.; Mealey, J.J., Jr.; Neal, J.H.; Olson, J.; et al. The Brain Tumor Cooperative Group NIH Trial 87-01: A randomized comparison of surgery, external radiotherapy, and carmustine versus surgery, interstitial radiotherapy boost, external radiation therapy, and carmustine. Neurosurgery 2002, 51, 343–355; discussion 355–347.
