In summary, treatment of GBMs with MRLs is associated with improvements in dosimetry and treatment planning due to its ability to detect subtle soft tissue changes and facilitate plan adaptation. Additionally, MRLs can account for changes in the tumor and tumor bed throughout treatment to ensure better target coverage while minimizing unnecessary dose to normal brain parenchyma. Future studies are needed to determine if this translates into better disease control durability and if better normal tissue sparing results in quality-of-life improvements for these patients.
2.2. Stereotactic Radiation Therapy for Intracranial Tumors
SRT is an important modality in the management of brain metastases and other intracranial tumors
[21][45]. An MRL offers several advantages over conventional linear accelerators, including enhanced target delineation, real-time tumor tracking, and adaptive treatment planning
[10]. The superior soft-tissue contrast provided by MRI allows for improved identification of tumor boundaries, while real-time imaging enables accurate monitoring of tumor motion during treatment, potentially reducing unnecessary radiation exposure to healthy brain tissue
[22][46].
Several studies have explored the dosimetric feasibility of MRgRT for intracranial SRT
[23][24][25][26][27][16,17,18,19,20]. One early study investigated the dosimetric feasibility of MRL for brain metastases and the impact of the magnetic field, concluding that MRL-generated stereotactic radiation plans meeting clinical requirements were feasible, and that the dosimetric impact of the magnetic field, including the electron return effect (ERE) at tissue–air boundaries, was minor and did not negatively affect target conformity or dose gradient
[23][16]. Another study evaluated the systematic localization accuracy, treatment planning capability, and delivery accuracy of an MRL platform for stereotactic radiosurgery (SRS), finding that excellent plan quality and delivery accuracy was achievable for concurrent treatment of multiple brain metastases with a single isocenter
[24][17].
Collectively, the above studies indicate that MRgRT using an MRL has the potential to offer dosimetric and logistical advantages over conventional linear accelerators for intracranial SRT treatment. However, further clinical investigations are necessary to evaluate the clinical benefit of this technology.
2.3. Stereotactic Radiation Therapy for Spine Tumors
Spine SRT plays a critical role in managing metastatic disease by alleviating pain, preventing pathological fractures, and reducing neurological morbidity. Stereotactic body radiotherapy (SBRT) has been shown to provide improved efficacy compared with conventional radiotherapy methods
[28][50]. For spine SBRT, fusion with either a planning MRI or CT myelogram is necessary to accurately delineate the spinal cord and establish a 1–2 mm planning organ-at-risk volume (PRV), potentially reducing disease coverage
[29][51]. CTgRT relies on bony structures for daily setup; however, it cannot visualize the spinal cord, leading to the requirement of a cord PRV for daily motion management.
MRLs offer several advantages over CTgRT, including MR imaging in treatment position to allow for easier fusion with the planning CT and superior spinal cord delineation during setup compared with cone-beam CT (CBCT)
[30][31][21,23]. Dosimetric feasibility studies indicate that daily MRgRT can lower the dose to the spinal cord
[32][22]. MRLs enable daily direct registration to the spinal cord, eliminating the need for cord PRVs while also allowing for improved tumor coverage with reduced margin size. In addition, low-field MRLs suffer from less image distortion from implanted metallic devices
[33][52]. MRI protocols outside of the radiation oncology department can often create challenges to performing an accurate fusion due to differences in slice thicknesses and patient positions
[34][53]; simulation and treatment planning using MRLs may address these issues
[31][23]. These advantages increase the therapeutic ratio and may allow for dose escalation.
2.4. Hippocampal Avoidance Whole Brain Radiotherapy
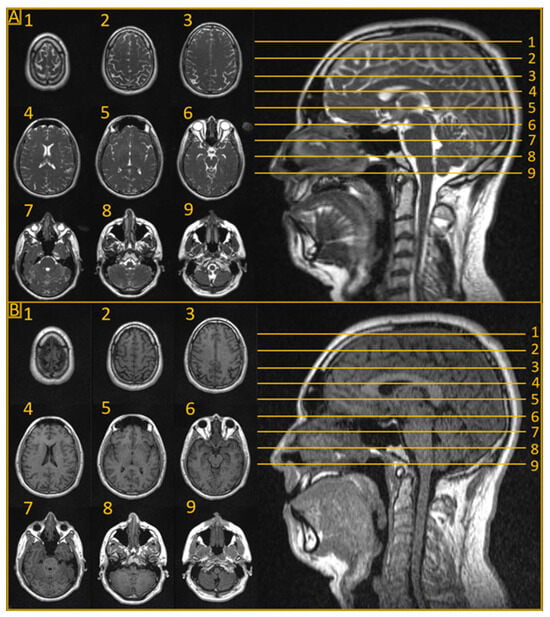
HA-WBRT is a promising technique that aims to achieve the local control benefits of whole brain RT for both macro- and micro-metastatic lesions, while reducing neurotoxicity by specifically avoiding the hippocampus
[35][54]. HA-WBRT requires fusion of a planning MRI with CT simulation imaging to create a hippocampal avoidance structure, while ensuring a homogenous treatment plan for the remaining brain parenchyma
[36][55]. HA-WBRT using MRgRT could facilitate adaptive treatment based on the intra-therapeutic tumor response, potentially improving the local control probability with sequential stereotactic boosts to nonresponding lesions. A dosimetric feasibility study compared twelve HA-WBRT volumetric modulated arc therapy (VMAT) plans versus intensity modulated radiation therapy (IMRT) plans created using the 0.35 T MRL treatment planning system (TPS)
[37][27]. In all cases, the researchers were able to generate plans that met RTOG 0933 treatment plan standards. As anticipated, the VMAT plans exhibited superior homogeneity and delivery times compared with the IMRT plans.
Particularly for patients with numerous brain metastases of radioresistant histology, HA-WBRT with a simultaneous integrated boost to gross disease may be an effective strategy
[14][38][14,56], one that may be further facilitated using MRgRT. Additional investigation through clinical trials is necessary to determine the clinical feasibility and safety of HA-WBRT. This approach could optimize the balance between effective tumor control and minimizing neurotoxicity for patients undergoing whole brain radiotherapy.
3. Summary
One of the fundamental goals of radiotherapy is maximizing the dose to target tissue while minimizing the dose to surrounding OARs. In a significant first step towards this aim, MRLs have facilitated treatment plan adaptation to observable anatomic changes throughout therapy. MRLs, however, may be able to enable biological plan adaptation by leveraging MRI’s capability to track biological and physiological changes through advanced mpMRI techniques. These techniques may allow radiation oncologists further insight into a tumor’s biology as it responds to RT over the course of treatment.
The treatment paradigm of radiotherapy has traditionally been based on empirical large cohort data rather than individual biology, resulting in a one-size-fits-all approach. However, recent advancements in genomics and radiomics have begun to pave the way towards a more personalized approach based upon individual tumor biology. The synergy between genomically informed radiotherapy, treatment of high-risk sub-volumes based on extraction of radiographic data, and daily mpMRI-guided plan adaptation has the potential to usher in a new treatment paradigm in radiation oncology. Pre-treatment genomic and radiomic analyses of the tumor may improve patient selection for MRL-based dose escalation
[39][40][41][30,57,58]. Daily mpMRI delta radiomic analysis can then be used to detect subtle biomarkers of treatment response in tumors, which hint at radiation-induced genomic plasticity, thereby allowing for even greater personalized adaptive treatment strategies
[42][43][44][45][59,60,61,62].
The currently active phase II Habitat Escalated Adaptive Therapy (HEAT), With Neoadjuvant Radiation for Soft Tissue Sarcoma (NCT05301283) is an example of a cutting-edge study utilizing genomic and mpMRI radiomic biomarkers to guide the initial treatment and adaptive treatment approach for high-grade soft tissue sarcomas. Utilizing a similar approach for CNS tumors appears to be technically feasible currently. For example, genomic-adjusted radiation therapy (GARD) could be similarly utilized to identify GBM patients who could benefit from higher doses
[46][63] with MRI perfusion
[47][64] and FLAIR
[48][49][65,66] sequences, which could identify tumor subpopulations to target with simultaneous integrated boosts.
MRL is poised to take a central role at the forefront of this paradigm shift to allow for plan adaptation based not only upon geometric shifts but also on a tumor’s evolving treatment response throughout therapy. An ultra-personalized treatment approach like this allows for total dose, dose distribution (i.e., dose painting), and fractionation changes throughout the course of therapy to improve clinical outcomes for patients.
Radiomic- and Genomic-Guided Adaptive Radiation Therapy for CNS Tumors
Historically, daily MRgRT plan adaptation has been utilized to manage interfractional geometric changes. However, MRI is also capable of assessing biological and physiological information using advanced mpMRI techniques
[50][51][52][53][28,67,68,69]. These techniques have the potential to be particularly beneficial for CNS tumors treated on an MRL.
One such technique is diffusion-weighted imaging (DWI), which enables the detection of water mobility changes
[54][70]. These alterations are associated with tumor growth
[55][71] or necrosis
[56][72]. By mapping a parameter known as the apparent diffusion coefficient (ADC), clinicians can monitor the response to radiation therapy
[57][73]. ADC mapping is especially appealing in adaptive radiotherapy, as changes in ADC can be observed before morphological alterations in the tumor
[58][74]. This feature could guide dose escalation strategies or biologically driven radiation plan adaptation
[41][59][58,75]. DWI has been applied on a 1.5 T MRI-guided linear accelerator
[60][61][62][76,77,78] and on a 0.35 T tri-cobalt system
[63][64][79,80].
Dynamic contrast-enhanced (DCE) MRI is another functional imaging technique that investigates perfusion by dynamically evaluating changes in the T
1 relaxation time following a bolus injection of gadolinium
[65][66][82,83]. This process allows for the examination of gadolinium transport across the capillary endothelium
[52][68]. DCE has demonstrated prognostic value in identifying patient subpopulations with hypoxia-related resistance to chemoradiation in cervical cancer
[67][84]. As a result, DCE has the potential to provide information that may aid in personalizing radiation dose delivery for CNS tumors
[61][77]. DCE has been implemented on the 1.5 T MRL, although its quantification was shown to be less reproducible than that of T
1, T
2, and ADC
[60][76]. While DCE has not yet been implemented on a 0.35 T MRL, initial experiences have demonstrated the feasibility of gadolinium injection on the tri-cobalt version of this system
[68][85].
Additional MR-based techniques, such as magnetic resonance spectroscopic imaging (MRSI)
[69][86], chemical exchange saturation transfer (CEST)
[70][71][87,88], and hyperpolarized dynamic magnetic resonance spectroscopy
[72][89], can interrogate metabolic processes in tumors
[73][90]. These techniques could potentially offer valuable information for the adaptive radiotherapy of CNS tumors on an MRL. MRSI has been applied to create high-resolution metabolite maps in gliomas
[74][91] and to map lactate in GBM
[75][92].
Genomics provides another powerful avenue towards personalized radiation treatment, which when combined with the advances in image guidance listed above, may provide an even more sophisticated approach for challenging malignancies such as GBM. Several such signatures have been introduced as a potential means for genomically guided RT
[40][46][76][77][78][79][80][57,63,106,107,108,109,110]. Genomics offers a biological framework for guiding RT, giving better context to the radiomic changes observed during treatment, and fostering research into predictive biomarkers. This combination may allow for novel advanced and better-informed approaches to dose escalation in high-grade glioma, a strategy which has been largely unsuccessful in the past
[81][82][83][84][111,112,113,114].
In summary, MRL can be leveraged by incorporating genomically guided RT and mpMRI radiomics to enable a biologically adaptive RT paradigm. Various mpMRI techniques, including DWI, DCE, MRSI, and CEST, have the potential to offer valuable insights into tumor biology and physiology, ultimately leading to more personalized and effective treatment strategies. Using these technologies to identify intratumoral heterogeneity and tumoral sub-volumes at risk may allow for focal dose escalation or avoidance, respectively. As research and development continues in this area, we expect significant advancements in the application of these techniques, potentially revolutionizing the management of CNS tumors.