Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Buddhika Sampath Kumara and Version 2 by Jessie Wu.
Bacterial infections and antibiotic resistance remain significant contributors to morbidity and mortality worldwide. Despite recent advances in biomedical research, a substantial number of medical devices and implants continue to be plagued by bacterial colonisation, resulting in severe consequences, including fatalities. The development of nanostructured surfaces with mechano-bactericidal properties has emerged as a promising solution to this problem. These surfaces employ a mechanical rupturing mechanism to lyse bacterial cells, effectively halting subsequent biofilm formation on various materials and, ultimately, thwarting bacterial infections.
- antibacterial surfaces
- nanofabrication
- antimicrobial
- polymeric implants
1. Introduction
Bacterial cells usually attach to surfaces, colonise, and form a matrix of polysaccharide material called biofilms. Bacteria can adhere to many different surfaces, including human tissues, metals, and polymeric surfaces [1]. The bacteria that form biofilms are highly resistant to disinfectants, antiseptics, and other antimicrobial agents that are normally effective in their planktonic state [2][3][4][2,3,4]. Moreover, overuse of antibiotics has led to an era where bacteria are becoming increasingly resistant to antibacterial agents, making it more difficult to treat infections [4][5][4,5]. The discovery of the mechano-bactericidal response to nano-topography found on insect wings, such as cicadas and dragonflies, has inspired the development of nanostructured topography on synthetic materials, which can reduce or inhibit the growth of bacteria on their surfaces. Most of the studies on artificial antibacterial micro/nanostructured surfaces were based on materials like ceramics, metals, and alloys, because of their superior mechanical and thermal properties that lead to potential applications in medical and industrial sectors. Metals are among the most used engineering materials and are employed extensively as biomaterials [6][7][6,7]. However, they can cause inflammation, bone loss, and imaging artifacts in computed tomography (CT) scans and magnetic resonance imaging (MRI) due to their magnetic properties, low flexibility, and low biocompatibility compared to biocompatible polymers [8][9][8,9]. High cost and density characteristics also make them less effective in specific medical implants such as cardiovascular implants, absorbable implants, paediatric implants, and cochlear implants [9][10][11][12][13][14][15][9,10,11,12,13,14,15]. Biocompatible polymers are attractive alternatives that can be used in such applications due to ease of processing, low weight, high biocompatibility, and biodegradability [16][17][18][19][16,17,18,19]. The methods for developing nanostructured bactericidal surfaces have been reviewed in the recent literature [20][21][22][23][24][20,21,22,23,24]. However, a comprehensive and critical overview of the techniques developed for polymers is yet missing.
2. Polymers Used in Biomedical Applications
Many biocompatible polymers are used in medical implants with some demonstrating high biocompatibility [25]. The most commonly used biocompatible polymers are polyglycolic acid (PGA) [26][27][26,27], poly(lactic-co-glycolic acid) (PLGA) [26][28][29][30][26,28,29,30], polycaprolactone (PCL) [26][31][32][26,31,32], polyurethane (PU) [33], polyvinyl alcohol (PVA) [34][35][36][34,35,36], silicone [33][37][38][33,37,38], polylactic acid (PLA) [26][39][40][41][42][43][44][26,39,40,41,42,43,44], polypropylene (PP) [45][46][45,46], and polymethyl methacrylate (PMMA) [47][48][49][47,48,49]. Each polymer has distinct advantages and limitations in various biomedical applications, as mentioned in Table 1. For instance, PMMA is a frequently used polymer for dental implants due to its non-degradability and high strength while PLA is used in bone tissue engineering applications due to its biodegradability and osteoblast stimulation [39][50][39,50]. Moreover, polyetheretherketone (PEEK) and polyetherketoneketone (PEKK) are emerging biomedical materials with high biocompatibility, thermal stability, and non-degradability with excellent mechanical properties which are suitable for various biomedical applications [51][52][51,52]. In such applications, one of the most concerning issues is implant failures due to bacterial infections as described in the Introduction section. Bacteria colonise various implant surfaces, such as dental implants, catheters, and orthopaedic implants [53]. Furthermore, antibiotic resistance directly contributes to implant failures due to the formation of biofilms on these surfaces [54][55][54,55]. In response to this concern, numerous studies have been undertaken to develop physical and chemical methods aimed at reducing bacterial colonisation [56][57][56,57]. To implement these strategies successfully, the choice of implant material plays a pivotal role in developing surfaces that are bactericidal and/or antifouling. Among various materials, polymers offer advantageous characteristics for biomedical implant applications. These attributes are highly considered in the biomedical field, particularly for ensuring a successful implant surgery in in vivo conditions (Figure 1).Table 1.
Polymers used in biomedical applications. Table abbreviations: Polydimethylsiloxane—PDMS; Polyethylene terephthalate—PET; Polytetrafluoroethylene—PTFE.
| Polymer | Characteristics, Physical, and Mechanical Properties | Biomedical Applications |
Advantages | Limitations | Ref. |
|---|---|---|---|---|---|
| PGA | Biodegradable, biocompatible, tensile stress: 890 MPa, density: 1.5 g/cm3, melting point: 225–230 °C, glass transition temperature: 35–40 °C | Tissue engineering applications in bone, tendon, cartilage, tooth, and spinal regeneration; nerve grafts; absorbable sutures | Stimulates cartilage regeneration; 3D-printability; high tensile strength | High friction coefficient and “binds and snags” when wet, high brittleness, high degradation causes inflammatory response | [26][27][[60][2658][59],27,58,59,60] |
| PLGA | Biodegradable, bioadsorbable, biocompatible, tensile stress: 3.4 MPa, density: 1.2 g/cm3, melting point: dependent on the percent composition (PLA, PGA), glass transition temperature: 40–60 °C | Therapeutic tools; drug delivery; tissue engineering | Stimulates osteoblasts; 3D-printability | Release of acidic byproducts leads to inflammation, degrade due to hydrolysis, poor strength | [26][28][29][30][61][26,28,29,30,61] |
| PCL | Biodegradable, bioadsorbable, biocompatible, tensile stress: 12.8 MPa, density: 1.15 g/cm3, melting point: 60 °C, glass transition temperature: −60 °C | Dental splints; drug delivery; tissue engineering | Stimulates osteoblasts; 3D printable; slow degradation rate; low cost in 3D printing due to low melting point; high biocompatibility | Poor mechanical properties; low cell adhesion | [26][31][62][26,31,62] |
| PU | Can be biodegradable or non-biodegradable based on chemical composition, non-bioabsorbable, biocompatible, tensile strength: 34.5–56 MPa, density: 1.23 g/cm3, melting point: 163 °C, glass transition temperature: −35 °C | Drug delivery; catheters, pacemaker leads insulation, vascular prostheses, heart valves, cardiac assist devices (cardiovascular applications) | High durability; high toughness; good biostability; low cost | Environmental stress cracking; material degradation in vivo; metal ion oxidation | [16][63][64][65][16,63,64,65] |
| PP | Non-biodegradable, non-bioabsorbable, biocompatible, tensile stress: 28 MPa, density: 0.9 g/cm3, melting point: 170 °C, glass transition temperature: −25 °C | Sutures; scaffolds (ligament or tendon repair); meshes for hernia and pelvic organ repair; heart valve structure, oxygenator and plasmapheresis membranes, finger joint prosthesis |
High melting point; less toxic; low cost | Limited biocompatibility; poor strength | [16][33][66][67][68][16,33,66,67,68] |
| PVA | Biodegradable, biocompatible, tensile stress: 40–90 MPa, density: 1.26 g/cm3, melting point: 228 °C, glass transition temperature: 85 °C | Wound dressings, drug delivery, targeted-tissue transportation systems; soft biomaterial implants. | High chemical and thermal stability; non-toxic | Weak hydrogel endurance in high temperature; relatively weak polymer; limited biocompatibility; degrades due to hydrolysis | [34][69]69[70],70[71],71[72][34,,72] |
| Silicone or PDMS | Non-absorbable, non-biodegradable, biocompatible, hydrophobic, tensile stress: 2–10 MPa, density: 0.97 g/cm3, melting point: 228 °C glass transition temperature: ~120–123 °C |
Oxygenator membrane; tubing; shunts; prostheses; heart peacemaker leads; heart valve structures; burn dressing | Chemically inert; low toxicity; thermal stability; high biocompatibility | Prone to damage; non-durable; contamination of monomers; low mechanical strength | [16][47][63][16,47,63] |
| PLA | Biodegradable, bioabsorbable, biocompatible, tensile stress: 21–60 MPa, density: 1.21–1.25 g/cm3, melting point: 150–160 °C, glass transition temperature: 60–65 °C | Bone tissue engineering; drug delivery; plates, screws, pins, and wires in bone fixation; bio-absorbable implants; sutures in dermatology; drug-eluting stents | High biocompatibility; stimulates osteoblasts; less brittle; one of the highly used 3D-printable materials; degradation products are also non-toxic to humans and the environment. | Low mechanical strength | [26][33]33[39][40][66],39[,4067,66][,6773][26,,73] |
| PMMA | Non-degradable, biocompatible, tensile stress: 48–76 MPa, density: 1.2 g/cm3, melting point: 130–180 °C, glass transition temperature: 80 °C | Dental implants; bone cement; lenses; drug delivery | One of the hardest thermoplastics with high scratch resistance; high mechanical strength | Less biocompatibility; high curing temperature; does not support osteointegration; causes necrosis effect | [16][74][75][16,74,75] |
| PEEK | Non-degradable, biocompatible, tensile stress: 84 MPa, density: 1.4 g/cm3, melting point: 343 °C, glass transition temperature: 143 °C | Dental implants; knee implants; spine implants; cranioplasticity; hip replacement; anterior plate fixation; heart valves; face reconstructions | High biocompatibility; 3D-printable; light weight; compatible with hydroxyapatite (natural bone tissue materials) hence substitute to metallic implants; stable at high temperatures; mechanical stability | Low thermoformability; bioinert (does not promote tissue integration); complex and costly manufacturing process | [76][77][78][76,77,78] |
| PEKK | Non-degradable, biocompatible, tensile stress: 115 MPa, density: 1.3 g/cm3, melting point: 363–386 °C, glass transition temperature: 162 °C | Dental implants; crown and bridge in dentistry; endodontic post; removable denture framework; restorative and prosthetic applications | High biocompatibility; 3D-printable; light weight; high mechanical strength; excellent chemical resistance | Bioinert (does not promote tissue integration); more complex and costly manufacturing process than PEEK | [52][79][52,79] |
| PET | Non-degradable, high biocompatibility, tensile stress: 75–100 MPa, density:1.38 g/cm3, melting point: 255–265 °C, glass transition temperature: 85 °C | Sutures; heart valves; surgical meshes; scaffolds; urinary and bloodstream catheters; commercial vascular prosthesis | 3D-printable; cost effective; excellent chemical resistance | Bioinert (does not promote tissue integration) | [80][81][82][80,81,82] |
| PTFE | Non-degradable, biocompatible, tensile stress: 30.5 MPa, density: 2.175 g/cm3, melting point: 327 °C, glass transition temperature: 127 °C | Vascular graft prostheses; heart patches; stapes prosthesis | High mechanical strength; chemically inert | Difficult to 3D-print | [16][83][16,83] |
| Chitosan | Biodegradable, biocompatible, tensile stress: 32.2 MPa, density: 0.20–0.38 g/cm3, melting point:105 °C, glass transition temperature: 75 °C | Antitumor drug delivery; protein and peptide drug delivery; gene delivery; antibiotic delivery; polyphenol delivery; wound healing applications | Antimicrobial; anti-inflammatory; antifungal; nontoxicity; antitumor activity; antioxidant activity | Low mechanical strength; significant variations of properties based on the source of material | [84][85][86][87][88][89][90][84,85,86,87,88,89,90] |
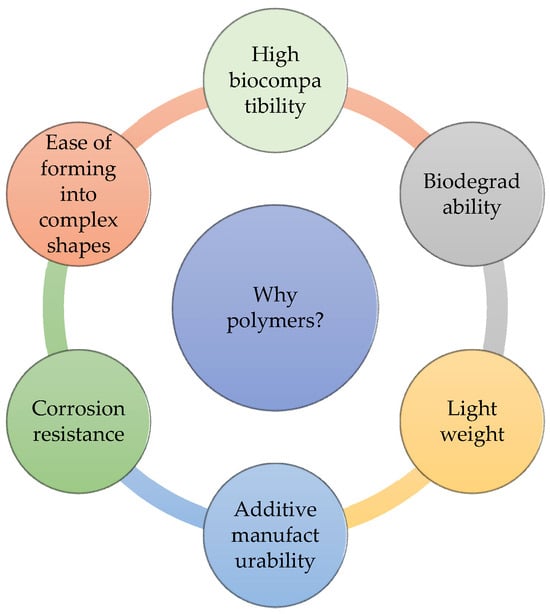
Figure 1. Driving factors to choose a polymer as implant material. Compared to other materials polymers provide some favourable characteristics for biomedical implant applications, which is essential in the biomedical field for successful implant in in vivo applications.
