Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Lindsay Dong and Version 3 by Lindsay Dong.
Wireless implantable biomedical devices (IBDs) are emerging technologies used to enhance patient treatment and monitoring. The performance of wireless IBDs mainly relies on their antennas. Concerns have emerged regarding the potential of wireless IBDs to unintentionally cause tissue heating, leading to potential harm to surrounding tissue. The previous literature examined temperature estimations and specific absorption rates (SAR) related to IBDs, mainly within the context of thermal therapy applications. Often, these studies consider system parameters such as frequency, input power, and treatment duration without isolating their individual impacts.
- antenna
- bioheat transfer
- electromagnetic heating
- finite element method (FEM)
- safety
1. Introduction
Wireless implanted biomedical devices (IBDs) are highlighted as essential components of the modern-day healthcare industry. They are a promising modality for various diagnostic [1][2] and therapeutic [3] clinical applications. Such applications include pacemakers [4], blood–glucose sensors [5], temperature monitoring [6], retinal implants [7], and imaging devices [8]. Examples of available commercial IBDs for different medical purposes are shown in Figure 1. In addition, IBDs are widely used for thermal therapies such as hyperthermia and microwave ablation (MWA) for tumor treatment in the lung [9], liver [10], breast [11], bone [12], prostate [13], and kidney [14]. Those therapies offer various advantages over traditional treatments, including (1) minimal invasiveness: involving incisions of approximately 3 mm, hence the recovery process can be accelerated; (2) effective heating: breaking the hydrogen bonds within the natural structure of proteins, leading to the impairment their functionality and causing cellular destruction [15]; and (3) ease of functionality: particularly for patients who are not surgical removal candidates due to limitations such as multiple tumor sites, tumor located in proximity to critical blood vessels, and tumor size [16]. In the case of hyperthermia treatment, the temperature is maintained within the range of 41 °C to 45 °C, while in the case of MWA treatment, the temperature exceeds 60 °C. Despite these potential benefits of IBDs, it is important to note that the constant communication between the human body and the external world is via electromagnetic (EM) radiation using an antenna. EM fields interacting with the human body could result in power dissipation within healthy tissues and, in turn, an undesired increase in temperature. In healthy tissue, for every 1 °C rise beyond 37 °C, the basal metabolic rate increases by approximately 10–12%. As a result, the heart rate accelerates, and there is an augmented need for water and calories [17]. Healthy tissues when exposed to EM radiation are at risk of various health hazards, including brain tumors, childhood leukemia, and the escape of albumin across the blood–brain barrier [18]. Furthermore, the electric conduction via IBDs can lead to tissue burns, affecting the surrounding tissues of both active and passive IBDs. The greatest risk is generally associated with small exposed regions that are in direct contact with the device [19]. Electrosurgery serves as an example of IBDs that is often associated with reports of adverse incidents and was included in the Emergency Care Research Institute’s (ECRI) report as one of the top 10 patient-related safety events in 2012. Sparks generated during electrosurgery have the potential to cause surgical fires occurring within the operating room, with the risk elevated when the tissue is saturated with high levels of oxygen or when combined with flammable substances such as alcohol [19].
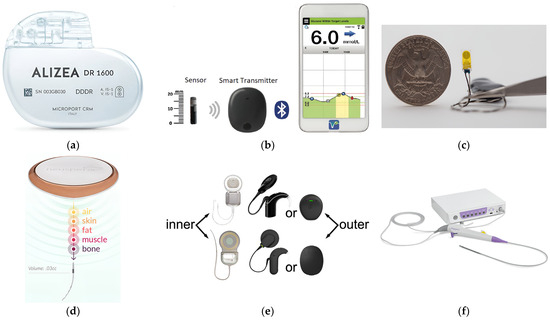
Figure 1. Examples of available commercial IBDs: (a) Pacemaker [20]; (b) blood–glucose sensor [21]; (c) temperature sensor [22]; (d) neurostimulation therapy implant [23]; (e) hearing aids [24]; and (f) imaging device [25].
The concern regarding the potential adverse effects of EM radiation on human healthy tissues has been extensively debated for over a decade. To estimate the level of EM absorption by a unit mass of the human tissue, a metric known as specific absorption rate (SAR) is utilized. Institutions such as ICNIRP and IEEE [26][27] formulated guidelines that rely on SAR values to regulate the interaction with EM radiation. However, the absorption of EM radiation in tissues leads to an increase in temperature, which is recognized as the primary cause of biological hazards in healthy tissues. Studies have emphasized the significance of studying SAR [28], as well as temperature elevation [19] in healthy tissues when exposed to EM radiations [29]. It is worth mentioning that most of the previous studies primarily focused on SAR optimization while using IBDs and often neglected the consideration of heat transfer and ensuring the absence of hot spots within the targeted biological tissue [26], leading to an incomplete assessment of the study outcomes. Moreover, the safety of the implanted antenna relies more on the temperature change induced within the tissue rather than the actual power density value [30][31]. In the study reported in [19], using an in vitro model, the tissue temperature adjacent to metal implants during electro-surgery was estimated to have a thermal coefficient of 0.088 °C/W/min. At a power level of 60 W, the temperature could rise to over 43 °C in just 1 min. Consequently, there is a notable risk of elevated tissue temperature when using extended activation durations or high-power values, which increases the potential risk of patient injury. Therefore, there is a need for heat transport modeling to comprehensively explain the actual process of IBD activation inside the human body.
The major method to reduce tissue heating (i.e., including SAR) is to reduce the input power. However, there are some other works around, such as the structure and placement of the implanted antenna. There might be some occasions where there is a choice of placing the implant in different tissue materials to reduce the heating and SAR. In most cases, there is no such option. Another factor to control is the gain and radiation patterns. One may use an antenna with an omnidirectional or as close as possible to an isotropic pattern to distribute the power around the tissue and not cause any hot spots. Some papers reported the use of ground plane or periodic structures such as electronic band gap structure to minimize the radiation toward the inner part of the body and increase the gain toward the outside; therefore, a reduced power combined with the higher gain can be used to reduce SAR. The other option is to use a layer of insolating heat-absorbing material around the antenna to insulate the antenna from the tissue. Reducing the discontinuities of the near E field using a Ferrite sheet and the use of metasurface techniques were also proposed in the literature to reduce SAR levels [28][29][30][31][32].
Many parameters influence the thermal rise observed during the IBD’s operation. Moreover, each individual possesses distinct biological characteristics, including tissue density, mechanical and electrical properties, and physiological characteristics [33]. Consequently, there is a significant need to conduct parametric studies to evaluate the impact of different parameters on the heat dissipation of IBDs and, subsequently, their overall efficiency [34]. Numerical modeling plays a crucial role in conducting parametric studies, as it allows for assessing the significance of underlying phenomena and facilitates improved optimization approaches of new IBD designs. Hence, it serves as a fast, convenient, and cost-effective means of evaluating and refining the device during the prototyping phase. In addition, numerical modeling offers a highly fast and controlled environment for simulating and evaluating device performance. A prime example is the clinical treatment involving MWA and hyperthermia procedures, where precise temperature control is necessary to ensure the selective elimination of cancer cells while minimizing harm to healthy biological tissues. Hence, both numerical and experimental models have been extensively employed as informative tools to investigate IBD activation within biological tissues. These models play a crucial role in offering essential treatment planning information to clinical practitioners for practical treatment strategies. They assist in determining the optimal placement of the device and the appropriate amount of microwave power to be delivered via the antenna. In addition, in the case of thermal therapy treatment procedures, by predicting the transient temperature profiles and the extent of damage within the target tissue while minimizing harm to the surrounding healthy tissue, these models define the duration of irradiation necessary for achieving complete tumor necrosis [35]; thus, they will enable precise and optimized treatment outcome.
23. Antenna Parameters
Numerous previous studies demonstrated encouraging outcomes of IBDs used for various treatment purposes. However, these studies often rely on several simplifying assumptions that do not represent the complex treatment environment [36]. These studies are often carried out utilizing either a two-dimensional (2D) model or ideal sources for the implanted antenna element, disregarding the actual radiation characteristics of a realistic implanted antenna that determine the actual direction and shape of traveling waves within the targeted body tissue [37][38]. Hence, the performance of optimized IBDs is closely linked to the antenna design, making its improvement an ongoing area of interest. An ideal implanted antenna should possess high-energy transmission efficiency for a long duration without damaging it, be noninvasive to patients, and maintain minimum heat dissipation levels to the healthy biological tissues, thus not causing hazardous effects. In addition to these requirements, in hyperthermia and ablation technologies, the antenna not only dictates the distribution of the produced heating but also influences the shape of the resulting ablation pattern (i.e., size and shape). Hence, it is important to consider the effect of the selected antenna’s structure, material, and size on the achieved thermal performance. The presented discussion focuses on the effect of changing these parameters on the antenna’s temperature profile during the IBD’s activation time and consequently, the heat dissipation inside the tissue and the comfort and safety of patients. On the other hand, when temperatures reach high levels, vaporization and carbonization take place, leading to changes in the complex permittivity of tissues, which affects the performance of the implanted antenna [39]. The number of slots included in the structure of the implanted slot antenna, such as single- [40], double- [41], triple- [42], and multiple-slot [43], in addition to the spacing between the slots was found to have a significant impact on the obtained temperature profile of the implanted antenna. In [6], the influence of single-slot and double-slot antennas on the temperature distribution inside the liver was investigated. The highest temperature values were achieved using a single-slot antenna. In [41], it was reported that after 240 s of activation time, the maximum localized temperature values inside the breast tumor reached over 60° C for three different antenna configurations: a single-slot antenna, a double-slot antenna with a slot’s spacing of 4.05 mm, and a double-slot antenna with a slot’s spacing of 0.4 mm.Antenna Size
A rechargeable neuromodulation system was investigated in [17] using a layered body model. The proposed system consists of an implanted antenna (i.e., implanted inside fat tissue) and a wearable antenna (i.e., placed on skin tissue). A parametric study was carried out on the implant thickness and radius of the antenna to determine the optimum size of the proposed system, resulting in minimal heat dissipation. Higher temperature values were observed within the tissue as the antenna radius was increased, while the implant size was found to be the least influential design parameter. In [44], the performance of two implanted double-slot antenna, which was designed using semi-rigid coaxial cables with different diameters was compared. The thick antenna of 6.35 mm diameter produced less maximum localized temperature of 191.8 °C and reduced heating along the antenna shaft when compared to the smaller antenna size of 2.21 mm. The value of the temperature in the case of the smaller antenna was 227.1 °C. It is worth mentioning the input power was set to 50 W at 2.45 GHz in all cases. In [45], the performance of three implanted coaxial microwave antennas with outer diameters of 1.03 mm, 1.6 mm, and 2.0 mm implanted inside ex vivo porcine lung were evaluated. The temperature profile of the 1.03 mm diameter antenna was the same as those of the 1.6 mm and 2.0 mm diameter. This reduced the incidence of health complications when the antenna was implanted in lung tissue due to the smaller antenna size. The invasiveness of the wireless IBDs may be increased due to the use of rigid implanted antennas and their percutaneous insertion. An example where these limitations become pronounced is in the case of lung tumors. The placement of such tumors and their proximity to nearby organs such as the heart, blood vessels, and diaphragm may restrict the feasibility of using rigid implanted antennas [46].34. System Parameters
A higher operating frequency of IBDs results in smaller sizes of implanted antennas as compared to implanted antenna operating at a lower frequency, resulting in less invasive IBDs and opening up possibilities for creating more compact multielement devices that can provide heating and biotelemetry properties that cannot be achieved using single-element antennas [47]. However, with higher wireless IBDs’ operating frequency, the absorbed EM power tends to concentrate more in the vicinity of the skin tissue. This outcome is predictable because the penetration depth of waves decreases with an increase in frequency. Thus, the heating effect at the skin layer, the temperature rise, and safety requirements require careful examination of the effect of IBDs’ operating frequency [36]. In general, changes in frequency can alter the electrical conductivity and the permittivity of the biological material, while a higher applied power would result in increased input energy. Consequently, these variations have a significant influence on the quantity of heat being delivered to biological tissues [48]. To the best of the authors’ knowledge, only a limited number of previous studies that were related to thermal therapy applications have taken into consideration the effect of operational parameters of wireless IBDs, such as frequency, applied microwave power, and treatment time in the optimization of the relevant parameters. It is worth mentioning that, in most of the reported studies in the literature, analysis was carried out considering the combined impact of system parameters (i.e., frequency, applied power, and treatment time) on the treatment procedure and outcomes rather than an independent variation of system parameters. As an example, to achieve an ablation zone size of 5 cm diameter using a 915 MHz system that consists of three implanted antennas, approximately 45 W of input power was delivered via each of the antennas and required approximately 10 min of application time. In contrast, by using a 2.45 GHz system, the input power had to be set to 100 W using a single antenna and an application time of approximately 4 min to 6 min [49][50].34.1. Operating Frequency
In [51], two commercial systems were employed to distinguish the differences between 915 MHz and 2.45 GHz systems utilized for hepatic tumor ablation. The comparison was based on the required amount of input power for lesion treatment. The 2.45 GHz system utilizes a single implanted antenna, while the 915 MHz system utilizes three implanted antennas [50].34.2. Applied Power
In [52], numerical investigations showed that temperature distribution in liver tissue was significantly affected by the input power to the coaxial implanted antenna. It was observed that high input power resulted in increased temperature values (i.e., above 50 °C), which may destroy healthy tissues. On the other hand, with a power of 10 W, the tumor tissues could be effectively destroyed without causing harm to the adjacent healthy tissue.34.3. Operating Frequency, Applied Power, and Treatment Time
In [48], the major parameters involved in EM heating inside healthy and tumor tissue types were investigated. Namely, parameters such as blood perfusion, metabolic heating rate, frequency, and input voltage were investigated. The findings showed that the applied voltage had the most significant impact on the maximum localized temperature, followed by the frequency of EM radiation, identified as the second significant factor. In fact, both input voltage and frequency were found to contribute to approximately 90% of the impact on the maximum attainable localized temperature. Interestingly, the interaction between all studied parameters was found to be insignificant. In [36], the impact of the frequency and input power on the focusing temperature during hyperthermia for breast cancer was investigated. The main goal of the study was to achieve the intended temperature at the targeted tissue after a given period of irradiation while preventing the occurrence of any elevated temperature zones within the healthy breast tissues. The study focused on the frequency band from 3 GHz to 7 GHz. This selection was made as a practical balance between the depth of penetration and the precision of effective treatment. Investigations suggest that depending on the breast density, the optimum frequency range for breast hyperthermia treatment is from 3.5 GHz to 4.5 GHz. In addition, shaping the temperature distribution inside targeted tissue can affect the treatment outcome, ultimately enhancing treatment efficacy. The heating pattern can be controlled and shaped by optimizing the excitation signal of the implanted antenna in terms of power amplitude and phase.45. Testing Environment Parameters
Considering all the essential facts presented earlier, from a medical practitioner’s perspective, the influence of each factor during IBD activation for different treatment purposes is crucial and can affect the heat dissipation inside the biological tissue, consequently affecting the treatment outcome. It is important to identify the impact of each parameter utilized in the treatment procedure before performing and assessing actual clinical treatment [48]. Clinical trials were conducted to evaluate IBDs for different medical purposes. It is worth mentioning that the safety considerations in these clinical trials were limited to SAR standards without considering the actual heat dissipation due to IBD activation. The reported studies in the literature were conclusive on the success of using both ex vivo and in vivo experiments in IBD evaluation and realization [53]. The numerical method can be used to define the temperature distribution of targeted biological tissue [23]. For example, finite element method (FEM), finite integration technique (FIT), finite difference time domain (FDTD), and method of moments (MoM) are commonly employed to discretize the partial differential equations in both time and spatial domains. Different simulation programs, including Abaqus (Dassault Systems), Icepak (ANSYS), COMSOL Multiphysics, FEKO (Altair), and CST Studio Suite (Dassault Systems) were equipped to offer comprehensive tools used to build and perform simulation applications related to antenna modeling, mimicking biological materials, mesh generation, selection of various physics components (i.e., EM and heat transfer modeling), and offering a good platform for evaluating results [54]. To confirm the feasibility of the proposed IBDs, investigating the robustness of the device against errors in tissue modeling is a crucial step in the design process. In addition, it ensures that heat dissipation in healthy biological tissues is kept at minimum levels [55]. Hence, conducting a closed-loop procedure that combines both EM and thermal simulations is important to ensure the absence of localized overheating inside the healthy tissues.45.1. Implantation Depth
In [56], temperatures in the range of 55 °C to 100 °C were reached inside porcine bone tissue using different levels of antenna insertion depths (i.e., 3.5 cm and 5 cm). The experimental results showed that the insertion of an implanted antenna equal to or less than 3.5 cm was not recommended. This is because such insertion depths modified the temperatures that could be reached inside bone tissue. The temperature distributions exhibited a concentration of heat in proximity to the antenna structure with a uniformly distributed thermal pattern.45.2. Phantom Type
In [36], various numerical breast models were employed for the hyperthermia treatment of breast cancer, as classified by the American College of Radiology [57]. These models represent a simple case of fatty tissue type in older women and a more complex case of younger women with very dense breast tissue. The employed models accurately replicate the physical form and structure of the human breast, consisting of eight distinct tissue types. These tissues include fat-1,2,3, glandular-1,2,3, skin, and muscle characterized by their specific levels of water content. It was found that to effectively focus the power on the targeted tumor inside a dense breast tissue, the optimal frequency is 4.2 GHz. This frequency is lower than the optimal value used for breasts of a fatty type because microwave signals experience higher attenuation when penetrating a dense breast. In both cases, the desired temperature is attained at the tumor location without causing any overheating in the surrounding healthy tissues.45.3. Phantom Size
In [41], the temperature distribution of different implanted antenna types inside breast phantoms of different sizes was evaluated. Spherical tumors with diameters of 1 cm and 1.5 cm were placed and tested inside the breast phantom. These scenarios were considered to simulate the use of MWA in early-stage breast cancer, which refers to stage 1 tumors with diameters less than 2 cm. Results demonstrated that when testing the tumor phantom with a 1 cm diameter, ablation temperatures (i.e., above 60 °C) were achieved in all tumor tissue areas using all tested antenna types. In contrast, when experimenting with a phantom tumor measuring 1.5 cm in diameter, the high-temperature profile extended over a 0.55 mm radius when using a single-slot antenna and 0.31 mm when employing a double-slot antenna. According to these results, in addition to the antenna geometry, the tumor dimensions modified the thermal pattern.45.4. Phantom Shape
In [58], the thermal profile of different-slot antennas was evaluated when inserted inside tumor tissue of three varying shapes (i.e., prolate, oblate, and spherical) and sizes. The study aimed to identify the most effective method for achieving the best treatment outcome while minimizing collateral damage. Results indicated that as the tumor size increased, a smaller size of cancerous cells was eliminated, and a higher level of side effects was noticed. Additionally, the tumor shape affected treatment efficiency. Elliptical tumors such as oblate and prolate were proved to be more challenging during treatment procedures compared to spherical tumors. Moreover, side effects were more noticeable in the scenario of oblate-shaped tumors than those obtained in the scenario of prolate-shaped tumors.56. Thermal Model Parameter
Electromagnetic heating in biological tissue represents a bioelectromagnetic problem that involves the coupling of thermal models represented by bioheat equations and electromagnetic waves, both of which include variables that possess temperature sensitivity [59]. Various thermal models have been suggested in the existing literature [60][61] in order to calculate the temperature distribution due to IBD implantation within the biological tissue. To analyze heat transfer in tissues, the widely recognized Pennes’s bioheat equation [62] has been widely used. This equation is recognized for its relatively straightforward application and effectiveness in the majority of scenarios. It captures the impact of blood flow on the heat distribution in the biological tissue, including diffusion and cooling effects arising from the blood circulation represented as volumetrically distributed heat sinks or sources [63]. Biological tissues generate heat via metabolic processes, and this heat production is an important factor in the thermal model. Metabolic heat generation depends on factors such as tissue type, activity level, and overall health. A reduction in the metabolic heat generation rate would increase the input energy. In addition, blood perfusion is a crucial parameter responsible for energy transfer via convection. If blood perfusion is elevated during IBD activation, it could potentially reduce the supplied energy from the implantation area, thereby hindering the creation of thermal lesions.56.1. Blood Perfusion and Metabolic Rate
In [48], blood perfusion and metabolic heat generation parameters in healthy tissue and tumors were varied for three levels (i.e., high, medium, and low). The maximum achieved temperature was considered the response variable of the studied cases. Findings indicated that a reduction in the blood perfusion rate would result in a higher temperature value. This result holds significant importance for treatment planning purposes. A tumor is an intricate and irregular structure resulting from the uncontrolled proliferation of cells with distinct characteristics. Commonly, there is a major vein responsible for the primary blood supply to the tumor. If, before treatment, a reduced blood supply to the tumor is achieved via this major vein, it will be possible to achieve a higher temperature in a shorter period of time using the same treatment arrangement. The same conclusion was highlighted in [64] for the MWA of liver tissue. The effects of different blood perfusion rates (i.e., 0, 1, 1.5, and 3 kg/(m3.s)) on temperature distribution were systematically simulated and analyzed. The results suggested that if the blood perfusion is elevated, the achieved temperature can be decreased.56.2. Temperature-Dependent Tissue Properties
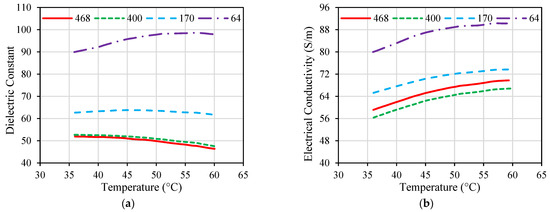
While many implanted antennas were proposed in the literature, the majority of them were designed and evaluated based on the assumption of normal ambient tissue. Hence, they have not taken into account the changes in the tissue property that may occur [43]. Electrical and thermal parameters of biological material can change with the temperature variations, as shown in Figure 2 and Figure 3 for porcine liver tissue. When the temperature of liver tissue is increased from 37 °C to above 100 °C, a 5% change in tissue permittivity will take place [40]. In addition, the frequent changes in tissue properties can influence the temperature distribution in the proximity of the implanted antenna [65]. These variations are anticipated to shift the location of the absorbed microwave energy in the biological tissue. Hence, the accuracy of the numerical model employed to evaluate the microwave heating and hazardous effects due to IBD implantation is crucial for the success of the optimization approach based on the temperature factor. Temperature-dependent electrical and thermal parameters of the biological tissues should be considered during the design and evaluation phases of the IBDs to describe the actual variations of these parameters. There have been different mathematical models utilized in the literature to represent temperature-dependent electrical and thermal properties.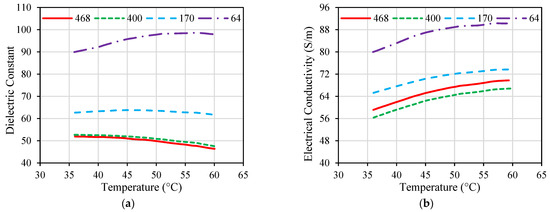
Figure 2. Dielectric properties of porcine liver tissue influenced by temperature at different frequencies given in MHz; (a) dielectric constant and (b) electrical conductivity. Data were recreated from [66].
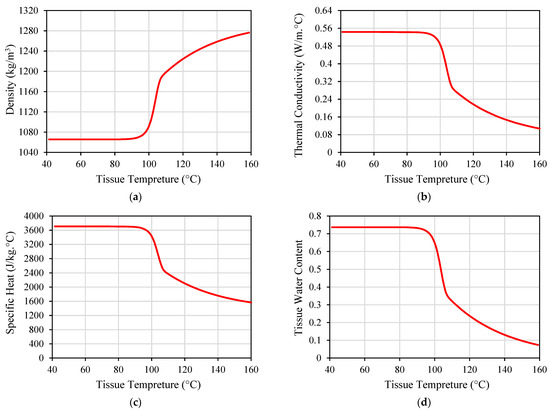
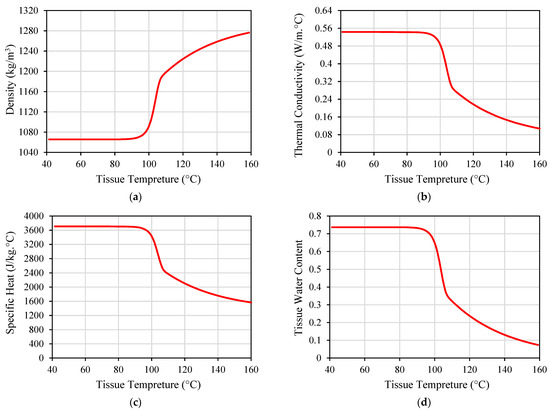
Figure 3. Thermal properties of porcine liver tissue influenced by temperature: (a) tissue density; (b) thermal conductivity; (c) specific heat; and (d) tissue water content. Data were recreated from [52].
References
- Li, P.; Lee, G.H.; Kim, S.Y.; Kwon, S.Y.; Kim, H.R.; Park, S. From Diagnosis to Treatment: Recent Advances in Patient-Friendly Biosensors and Implantable Devices. ACS Nano 2021, 15, 1960–2004.
- Alemaryeen, A. Compact Wideband Antenna for Wireless Capsule Endoscopy System. Appl. Phys. A Mater. Sci. Process. 2021, 127, 271.
- Joo, H.; Lee, Y.; Kim, J.; Yoo, J.S.; Yoo, S.; Kim, S.; Arya, A.K.; Kim, S.; Choi, S.H.; Lu, N.; et al. Soft Implantable Drug Delivery Device Integrated Wirelessly with Wearable Devices to Treat Fatal Seizures. Sci. Adv. 2021, 7, eabd4639.
- Sharma, D.; Kanaujia, B.K.; Kaim, V.; Mittra, R.; Arya, R.K.; Matekovits, L. Design and Implementation of Compact Dual-Band Conformal Antenna for Leadless Cardiac Pacemaker System. Sci. Rep. 2022, 12, 3165.
- Satish; Sen, K.; Anand, S. Demonstration of Microstrip Sensor for the Feasibility Study of Non-Invasive Blood-Glucose Sensing. Mapan—J. Metrol. Soc. India 2021, 36, 193–199.
- Zhang, Y.; Liu, C.; Zhang, K.; Cao, H.; Liu, X. Design and In-Vivo Testing of a Low-Cost Miniaturized Capsule System for Body Temperature Monitoring. Int. J. RF Microw. Comput. Eng. 2019, 29, e21793.
- Cehajic Kapetanovic, J.; Troelenberg, N.; Edwards, T.L.; Xue, K.; Ramsden, J.D.; Stett, A.; Zrenner, E.; MacLaren, R.E. Highest Reported Visual Acuity after Electronic Retinal Implantation. Acta Ophthalmol. 2020, 98, 736–740.
- Hayat, S.; Shah, S.A.A.; Yoo, H. Miniaturized Dual-Band Circularly Polarized Implantable Antenna for Capsule Endoscopic System. IEEE Trans. Antennas Propag. 2021, 69, 1885–1895.
- Healey, T.T.; March, B.T.; Baird, G.; Dupuy, D.E. Microwave Ablation for Lung Neoplasms: A Retrospective Analysis of Long-Term Results. J. Vasc. Interv. Radiol. 2017, 28, 206–211.
- Izzo, F.; Granata, V.; Grassi, R.; Fusco, R.; Palaia, R.; Delrio, P.; Carrafiello, G.; Azoulay, D.; Petrillo, A.; Curley, S.A. Radiofrequency Ablation and Microwave Ablation in Liver Tumors: An Update. Oncologist 2019, 24, e990–e1005.
- Zhou, W.; Zha, X.; Liu, X.; Ding, Q.; Chen, L.; Ni, Y.; Zhang, Y.; Xu, Y.; Chen, L.; Zhao, Y.; et al. US-Guided Percutaneous Microwave Coagulation of Small Breast Cancers: A Clinical Study. Radiology 2012, 263, 364–373.
- Geyikoglu, M.D.; Cavusoglu, B. Non-Invasive Microwave Hyperthermia for Bone Cancer Treatment Using Realistic Bone Models and Flexible Antenna Arrays. Electromagn. Biol. Med. 2021, 40, 353–360.
- Albarqi, H.A.; Demessie, A.A.; Sabei, F.Y.; Moses, A.S.; Hansen, M.N.; Dhagat, P.; Taratula, O.R.; Taratula, O. Systemically Delivered Magnetic Hyperthermia for Prostate Cancer Treatment. Pharmaceutics 2020, 12, 1020.
- ATEŞ, Ö.F. Effectiveness and Reliability of Percutaneous Microwave Ablation Therapy in Early Stage Renal Cell Cancer: Intermediate Term Results. J. Surg. Med. 2020, 4, 1068–1072.
- Shamekhi, L.; Sayehvand, H.O.; Karami, H. Tumour Shape-Dependent Microwave Hyperthermia Using a Novel Coaxial Micro-Cut Slot Antenna. J. Therm. Biol. 2020, 88, 102473.
- Peng, T.; O’Neill, D.P.; Payne, S.J. A Two-Equation Coupled System for Determination of Liver Tissue Temperature during Thermal Ablation. Int. J. Heat Mass Transf. 2011, 54, 2100–2109.
- Celik, N.; Turgut, E.; Bayazit, Y. Design Analysis of an Implant and Antenna System by Using Taguchi Method. Heat Mass Transf. 2018, 54, 403–413.
- Kim, J.H.; Lee, J.K.; Kim, H.G.; Kim, K.B.; Kim, H.R. Possible Effects of Radiofrequency Electromagnetic Field Exposure on Central Nerve System. Biomol. Ther. 2019, 27, 265–275.
- Martinsen, T.; Pettersen, F.J.; Kalvøy, H.; Tronstad, C.; Kvarstein, G.; Bakken, A.; Høgetveit, J.O.; Martinsen, Ø.G.; Grimnes, S.; Frich, L. Electrosurgery and Temperature Increase in Tissue with a Passive Metal Implant. Front. Surg. 2019, 6, 8.
- Alizea Pacemaker System, USA. Available online: https://www.medicaldevice-network.com/projects/alizea-pacemaker-system-usa/ (accessed on 15 September 2023).
- Tardo, A.M.; Irace, C.; Del Baldo, F.; Foglia, A.; Fracassi, F. Clinical Use of a 180-Day Implantable Glucose Monitoring System in Dogs with Diabetes Mellitus: A Case Series. Animals 2022, 12, 860.
- Implanted Tempreture Sensor. Available online: https://medicalxpress.com/news/2023-09-device-transplanted-early.html (accessed on 15 September 2023).
- Neurostimulation Therapy Implant. Available online: https://neuspera.com/technology/ (accessed on 15 September 2023).
- Hearing Aids. Available online: https://www.cochlearimplants.co.za/learn-about-cochlear-implants/ (accessed on 15 September 2023).
- Imaging Device. Available online: https://www.med-technews.com/medtech-insights/latest-medtech-insights/state-of-the-art-endoscopy-and-imaging-scivita-medical-s-g/ (accessed on 15 September 2023).
- IEEE. IEEE Standard for Safety Levels With Respect to Human Exposure to Radio Frequency Electromagnetic Fields, 3 KHz to 300 GHz; IEEE: New York, NY, USA, 2006; Volume 2005.
- Ahlbom, A.; Bergqvist, U.; Bernhardt, J.H.; Cesarini, J.P.; Court, L.A.; Grandolfo, M.; Hietanen, M.; McKinlay, A.F.; Repacholi, M.H.; Sliney, D.H.; et al. Guidelines for Limiting Exposure to Time-Varying Electric, Magnetic, and Electromagnetic Fields (up to 300 GHz). Health Phys. 1998, 74, 494–521.
- Das, S.; Mitra, D.; Chezhian, A.S.; Mandal, B.; Augustine, R. A Novel SAR Reduction Technique for Implantable Antenna Using Conformal Absorber Metasurface. Front. Med. Technol. 2022, 4, 924433.
- Bhargava, D.; Rattanadecho, P.; Wessapan, T. The Effect of Metal Objects on the SAR and Temperature Increase in the Human Head Exposed to Dipole Antenna (Numerical Analysis). Case Stud. Therm. Eng. 2020, 22, 100789.
- Karthik, V.; Rao, T.R. SAR Investigations on the Exposure Compliance of Wearable Wireless Devices Using Infrared Thermography. Bioelectromagnetics 2018, 39, 451–459.
- Thotahewa, K.M.S.; Redoute, J.-M.; Yuce, M.R. Propagation, Power Absorption, and Temperature Analysis of UWB Wireless Capsule Endoscopy Devices Operating in the Human Body. IEEE Trans. Microw. Theory Tech. 2015, 63, 3823–3833.
- Guido, K.; Kiourti, A. Wireless Wearables and Implants: A Dosimetry Review. Bioelectromagnetics 2020, 41, 3–20.
- Kumar, J.; Repaka, R. Numerical Investigation on the Effect of Different Physiological Cancerous Breast Parameters on the Output of Microwave Ablation. ASME J. Med. Diagn. 2020, 3, 031001.
- Lazzi, G. Thermal Effects of Bioimplants. IEEE Eng. Med. Biol. Mag. 2005, 24, 75–81.
- Singh, S.; Repaka, R.; Al-Jumaily, A. Sensitivity Analysis of Critical Parameters Affecting the Efficacy of Microwave Ablation Using Taguchi Method. Int. J. RF Microw. Comput. Eng. 2019, 29, e21581.
- Nguyen, P.T.; Abbosh, A.; Crozier, S. Microwave Hyperthermia for Breast Cancer Treatment Using Electromagnetic and Thermal Focusing Tested on Realistic Breast Models and Antenna Arrays. IEEE Trans. Antennas Propag. 2015, 63, 4426–4434.
- Converse, M.; Bond, E.J.; Van Veen, B.D.; Hagness, S.C. A Computational Study of Ultra-Wideband versus Narrowband Microwave Hyperthermia for Breast Cancer Treatment. IEEE Trans. Microw. Theory Tech. 2006, 54, 2169–2180.
- Zastrow, E.; Hagness, S.C.; Van Veen, B.D.; Medow, J.E. Time-Multiplexed Beamforming for Noninvasive Microwave Hyperthermia Treatment. IEEE Trans. Biomed. Eng. 2011, 58, 1574–1584.
- Brace, C. Thermal Tumor Ablation in Clinical Use. IEEE Pulse 2011, 2, 28–38.
- Keangin, P.; Rattanadecho, P.; Wessapan, T. An Analysis of Heat Transfer in Liver Tissue during Microwave Ablation Using Single and Double Slot Antenna. Int. Commun. Heat Mass Transf. 2011, 38, 757–766.
- Ortega-Palacios, R.; Trujillo-Romero, C.J.; Cepeda-Rubio, M.F.J.; Leija, L.; Vera Hernández, A. Heat Transfer Study in Breast Tumor Phantom during Microwave Ablation: Modeling and Experimental Results for Three Different Antennas. Electronics 2020, 9, 535.
- Jiang, Y.; Zhao, J.; Li, W.; Yang, Y.; Liu, J.; Qian, Z. A Coaxial Slot Antenna with Frequency of 433 MHz for Microwave Ablation Therapies: Design, Simulation, and Experimental Research. Med. Biol. Eng. Comput. 2017, 55, 2027–2036.
- Wang, T.; Zhao, G.; Qiu, B. Theoretical Evaluation of the Treatment Effectiveness of a Novel Coaxial Multi-Slot Antenna for Conformal Microwave Ablation of Tumors. Int. J. Heat Mass Transf. 2015, 90, 81–91.
- Ibitoye, A.Z.; Bose Adedokun, M.; Nwoye, E.; Ogese, O.C.; Adedokun, M.B.; Habeebu, M.Y.; Nwoye, E.O.; Aweda, A.M. Evaluation of the Performance of Designed Coaxial Antennas for Hyperthermia Using Simulation and Experimental Methods. Pol. J. Med. Phys. Eng. 2021, 27, 109–117.
- Cai, H.; Tian, H.; Wei, Z.; Ye, X. Microwave Ablation of the Lung: Comparison of 19G with 14G and 16G Microwave Antennas in Ex Vivo Porcine Lung. J. Cancer Res. Ther. 2022, 18, 1876–1883.
- Pfannenstiel, A.; Keast, T.; Kramer, S.; Wibowo, H.; Prakash, P. Flexible Microwave Ablation Applicator for the Treatment of Pulmonary Malignancies. In Proceedings of the Energy-Based Treatment of Tissue and Assessment IX, San Francisco, CA, USA, 29–30 January 2017; Volume 10066.
- Luyen, H.; Gao, F.; Hagness, S.C.; Behdad, N. Microwave Ablation at 10.0 GHz Achieves Comparable Ablation Zones to 1.9 GHz in Ex Vivo Bovine Liver. IEEE Trans. Biomed. Eng. 2014, 61, 1702–1710.
- Jamil, M.; Yin-Kwee Ng, E. Ranking of Parameters in Bioheat Transfer Using Taguchi Analysis. Int. J. Therm. Sci. 2013, 63, 15–21.
- Padma, S.; Martinie, J.B.; Iannitti, D.A. Liver Tumor Ablation: Percutaneous and Open Approaches. J. Surg. Oncol. 2009, 100, 619–634.
- Martin, R.C.G.; Scoggins, C.R.; McMasters, K.M. Safety and Efficacy of Microwave Ablation of Hepatic Tumors: A Prospective Review of a 5-Year Experience. Ann. Surg. Oncol. 2010, 17, 171–178.
- Simo, K.A.; Tsirline, V.B.; Sindram, D.; McMillan, M.T.; Thompson, K.J.; Swan, R.Z.; McKillop, I.H.; Martinie, J.B.; Iannitti, D.A. Microwave Ablation Using 915-MHz and 2.45-GHz Systems: What Are the Differences? HPB 2013, 15, 991–996.
- Selmi, M.; Bin Dukhyil, A.A.; Belmabrouk, H. Numerical Analysis of Human Cancer Therapy Using Microwave Ablation. Appl. Sci. 2020, 10, 211.
- Singh, S.K.; Yadav, A.N. Design of a Novel Externally-Tapped Intertwining Helical Antenna for Microwave Ablation and Its Statistical Analysis on Tissue Model. Int. J. RF Microw. Comput. Eng. 2021, 31, e22905.
- Ibitoye, A.Z.; Orotoye, T.; Nwoye, E.O.; Aweda, M.A. Analysis of Efficiency of Different Antennas for Microwave Ablation Using Simulation and Experimental Methods. Egypt. J. Basic Appl. Sci. 2018, 5, 24–30.
- Alemaryeen, A.; Noghanian, S. Effect of Thermal Design Considerations of Implanted Antenna on Tissue Heating. In Proceedings of the 2023 International Applied Computational Electromagnetics Society Symposium (ACES), Monterey, CA, USA, 26–30 March 2023.
- Jessica Trujillo-Romero, C.; Leija-Salas, L.; Vera-Hernández, A.; Rico-Martínez, G.; Gutiérrez-Martínez, J. Double Slot Antenna for Microwave Thermal Ablation to Treat Bone Tumors: Modeling and Experimental Evaluation. Electronics 2021, 10, 761.
- Zastrow, E.; Davis, S.K.; Lazebnik, M. Database of 3D Grid-Based Numerical Breast Phantoms for Use in Computational Electromagnetics Simulations; University of Wisconsin: Madison, WI, USA, 2007.
- Tehrani, M.H.H.; Soltaniid, M.; Soltaniid, M.; Soltaniid, M.; Soltaniid, M.; Soltaniid, M.; Kashkooli, F.M.; Raahemifar, K.; Raahemifar, K.; Raahemifar, K. Use of Microwave Ablation for Thermal Treatment of Solid Tumors with Different Shapes and Sizes-A Computational Approach. PLoS ONE 2020, 15, e0233219.
- Kernot, D.; Yang, J.; Williams, N.; Thomas, T.; Ledger, P.; Arora, H.; van Loon, R. Transient Changes during Microwave Ablation Simulation: A Comparative Shape Analysis. Biomech. Model. Mechanobiol. 2023, 22, 271–280.
- Waterman, F.M.; Tupchong, L.; Nerlinger, R.E.; Matthews, J. Blood Flow in Human Tumors during Local Hyperthermia. Int. J. Radiat. Oncol. Biol. Phys. 1991, 20, 1255–1262.
- Silva, M.; Freitas, B.; Andrade, R.; Espregueira-Mendes, J.; Silva, F.; Carvalho, Ó.; Flores, P. Computational Modelling of the Bioheat Transfer Process in Human Skin Subjected to Direct Heating and/or Cooling Sources: A Systematic Review. Ann. Biomed. Eng. 2020, 48, 1616–1639.
- Pennes, H.H. Analysis of Tissue and Arterial Blood Temperatures in the Resting Human Forearm. J. Appl. Physiol. 1998, 85, 5–34.
- Karampatzakis, A.; Kühn, S.; Tsanidis, G.; Neufeld, E.; Samaras, T.; Kuster, N. Antenna Design and Tissue Parameters Considerations for an Improved Modelling of Microwave Ablation in the Liver. Phys. Med. Biol. 2013, 58, 3191–3206.
- Wang, J.; Huang, S.; Gao, H.; Liu, J.; Zhang, Y.; Wu, S. Computer Simulations of Dual-Antenna Microwave Ablation and Comparison to Experimental Measurements. Appl. Sci. 2022, 13, 26.
- Curto, S.; Taj-Eldin, M.; Fairchild, D.; Prakash, P. Microwave Ablation at 915 MHz vs 2.45 GHz: A Theoretical and Experimental Investigation. Med. Phys. 2015, 42, 6152–6161.
- Fu, F.; Xin, S.X.; Chen, W. Temperature-and Frequency-Dependent Dielectric Properties of Biological Tissues within the Temperature and Frequency Ranges Typically Used for Magnetic Resonance Imaging-Guided Focused Ultrasound Surgery. Int. J. Hyperth. 2014, 30, 56–65.
More
