Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by George Paltoglou and Version 2 by Rita Xu.
Obesity is a multifactorial chronic impairment that further decreases quality of life and life expectancy. Worldwide, childhood obesity has become a pandemic health issue causing several comorbidities that frequently present already in childhood, including cardiovascular (hypertension, dyslipidemia), metabolic (Type 2 diabetes mellitus, fatty liver disease, metabolic syndrome), respiratory, gastrointestinal and musculoskeletal disorders.
- children
- adolescents
- childhood obesity
- treatment
1. Introduction
During the last decades, the prevalence and the severity of childhood obesity has been rising dramatically worldwide. Presently, according to epidemiological data, the prevalence of overweight/obesity in the age group under 5 years is 40 million children, while the relative prevalence for the age group between 5 and 19 years is over 340 million children [1]. Overall, it has been estimated that in the 5–19 age group the prevalence of obesity has increased from 11 million in 1975 to 124 million in 2016 [2]. However, there are reports indicating that the prevalence of childhood obesity in Western Europe, the USA, Japan and Australia has stabilized or even decreased, especially amongst girls and preschool children [3]. Nevertheless, the long-term tendency suggests that obesity in children of all ages will continue to increase [4].
Excess adiposity validly correlates with significant adverse health consequences on multiple organs/systems, including metabolic, endocrine, cardiovascular, gastrointestinal, pulmonary, neurological, psychological and skeletal complications [5].
Many studies have convincingly shown that childhood obesity is correlated with increased risk factors for cardiovascular (CV) diseases in adulthood, including hypertension, Type 2 diabetes (T2D), dyslipidemia, metabolic syndrome (MS) and early development of atherosclerosis [6][7][8][9][6,7,8,9]. Most alarming is that obesity itself and these risk factors are fairly stable in adolescents and tend to track into adulthood, unless the body mass index (BMI) improves [10]. In addition, excess weight in childhood has been found as an independent risk factor for various malignancies, such as colon, rectal and esophageal adenocarcinoma; endometrial and postmenopausal breast cancer; and sudden death [11][12][11,12]. The estimated decrease in life expectancy due to obesity is 0.8 to 7 years [13]. Moreover, the duration and severity of obesity in the pediatric population correlates positively with the risk for comorbidities and mortality in adulthood [14].
Emotional disorders related to childhood obesity include mood disorders, low self-esteem, anxiety and social isolation [15][16][15,16]. Children with excess weight are more likely to have fewer friends, lower school performance, more psychosocial problems and to be affected by bullying behaviors and social exclusion compared with their peers with normal weight [17]. In addition, unhealthy behaviors, such as alcohol or tobacco use, risky sexual behaviors, unfavorable dieting habits and physical inactivity are encountered more frequently among adolescents with excess weight [16].
Although the literature data show that lifestyle modification programs are effective only if applied intensively and continuously, they remain the cornerstone of obesity management. Pharmacotherapy has been recommended only for obese youth with serious comorbidities resistant to lifestyle changes [18]. Finally, bariatric surgery is the last alternative for adolescents with severe obesity, complicated by serious health problems, who have not been successful with lifestyle modification and medication [19].
2. Prevention
Given the difficulty of losing weight through lifestyle intervention, as well as the subsequent weight maintenance and the potential harm of medication and surgery, obesity prevention should be a public health issue. It is therefore understood that childhood is an important period for preventing the development of obesity before it begins to create serious and irreversible health problems. In general, agreements for multi-sectional collaboration from governments, the private sector (food industries, advertising organizations, the media), civil society (consumer associations, public-interest organizations, academic institutions, research foundations, professional associations) and the public is mandatory in order to prevent obesity, as no single sector is able to solve the obesity burden on their own. Public health can have a primary role in coordination among local and national units, determining the principles that will establish a framework for effective obesity prevention strategies. These include individual behavior modifications; setting changes in multiple environments like homes, schools and workplaces; and sector change within food industries, advertising industries, agriculture, education, urban planning and transportation, such as:- -
-
The development of an urban planning policy, including access to green spaces, public transportation and school facilities;
- -
-
Mass media campaigns and mobile apps to raise public consciousness of healthy eating and activity;
- -
-
Reduction in junk food and beverage marketing, especially to children;
- -
-
School-based programs combining nutrition and physical education, skill-building and policy changes;
- -
-
Removing unhealthy foods from school canteens and vending machines (for example, since 2005 France has banned all vending machines from schools);
- -
-
The provision of community-based strategies to inform people on healthy eating and physical activity, as well as support exclusive breastfeeding;
- -
-
Regularly measuring BMI, counseling on healthy habits and prescription of physical activity by primary care doctors;
- -
-
Action to alter the cost of healthy choices, such as taxes on unhealthy food products (such as sugary, energy-dense food and drinks) and subsidies for healthy choices (fruits, vegetables);
- -
-
The provision of informed choices to people by labeling food products and restaurant menus;
- -
-
Food reformulation and the development of healthier products, as occurred in 2018 in England, when Public Health England required the industry to reduce calories by 20% in foods high in sugar, salt and saturated fat by the year 2024 [20][21][20,21].
3. Treatment
Obesity is a long-lasting, relapsing disorder that necessitates longitudinal care provided by an interdisciplinary group of trained health-care professionals, including pediatricians, dieticians, psychologists, exercise instructors and social workers. The participation of families, schools, communities and health policy makers is required to ensure coordination and universal accessibility. Guidelines for the treatment of pediatric overweight/obesity take into consideration various factors, such as the patient’s age, the degree of adiposity and the presence of comorbidities. The management of obesity requires behavioral changes, diet modifications, improved quality of sleep and increased physical as well as decreased sedentary activities (Figure 1). Intervention programs often include family participation, especially for children under the age of 12 years, given that parents influence children’s eating and physical activity habits significantly [24].The most effective behavioral approaches are goal setting, positive reinforcement, self-monitoring, contingency training, stimulus control, cognitive restructuring, behavior chains, problems solving and relapse prevention. Treatments such as appetite-awareness training and the regulation of cues are considered experimental. According to the US Preventive Services Task Force, a multicomponent intervention program is usually most effective (with a reduction in the BMI z score ≥ 0.20) when it occurs in person, engages the entire family and delivers at least 26 h per year of nutrition, physical activity and behavior-change sessions over 3 to 12 months [25]. However, it is difficult to implement such interventions since they are costly and require a multidisciplinary team with specific training. Nevertheless, in severe cases of obesity, pharmacotherapy, and even bariatric surgery, may be considered as alternative treatment options [18]. Bariatric surgery is a viable option for adolescents with severe obesity and relevant medical comorbidities who have not seen weight loss with conventional lifestyle and pharmacologic interventions. However, since the majority of children with high BMI do not exhibit life-threatening comorbidities, the risk–benefit ratio of metabolic surgery is difficult to assess [19].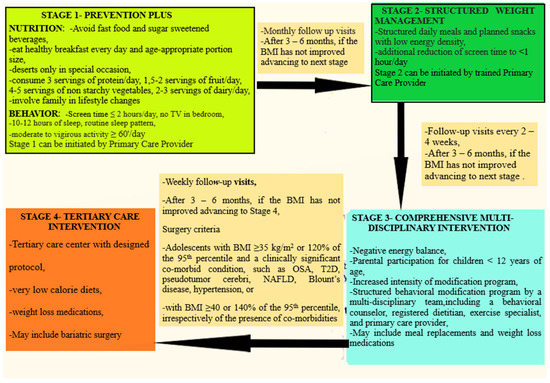 Figure 1. Clinical algorithm for childhood obesity treatment.
Figure 1. Clinical algorithm for childhood obesity treatment.3.1. Dietary Management
The mainstay of obesity treatment is dietary management. Generally, typical weight-management programs are based on the reduction of caloric intake in order to induce a moderate weight loss of 0.5 kg per week [26]. A classic example of a diet aiming at controlling calories is the Traffic Light Diet, according to which foods are color-coded so as to separate those one might eat freely (green) from those one should consume more cautiously (amber and especially red) [27]. A large research body focuses on determining the most efficient distribution of macronutrients for successful weight loss, along with other potential metabolic benefits, with conflicting results. Low-carbohydrate (10–30% of caloric intake from carbs) and low-fat (18–40% caloric intake from fat) diets have been proven efficacious in the short-term [28]. These diets presumably foster satiety, resulting in lower caloric intake. A 12-week trial showed that high-protein, low-carbohydrate (HPLC) diets had greater short-term efficacy than low-fat (LF) diets. However, by the end of the study, the efficacy of both diets was similar [29]. Furthermore, markers of cardiovascular risk and insulin resistance improved in both groups, with the HPLC diet demonstrating greater results of insulin resistance markers. The potential superiority of low-glycemic-index diets compared with energy-restricted, low-fat diets in body-weight reduction has been shown in several pediatric studies, probably due to delayed insulin secretion, which may in turn cause prolonged satiety. The DiOGenes randomized controlled trial demonstrated protective effects of the combined use of a high-protein (HP)/low-glycemic-index (L-GI) diet against obesity [30]. Very low-calorie diets or VLCDs, i.e., hypo-caloric diets that provide 800 calories or less per day, are only used with severe forms of obesity. Since VLCDs aim to achieve significant weight loss without severe electrolyte imbalance, medical supervision is recommended when the duration of treatment lasts over 3 weeks [31]. Due to expeditious results in weight loss, improvements in body composition and metabolic parameters, VLCDs could be considered as alternatives to pharmacological and/or surgical interventions for adolescents with severe obesity. Therefore, the long-term safety and comparable beneficial effects of these diets in pediatric populations merit further research. Prebiotic supplementation has shown promise in managing pediatric obesity with notable improvements in satiety and lower energy intake [32]. Diet is a well-established effective short-term intervention for achieving weight loss and improvement of the cardio metabolic profile [33][34][33,34]. Comparison of the outcome of a hypo-caloric diet vs. exercise showed improvements in BMI, blood lipids and adiponectin levels in both groups at 12 weeks and greater reductions in BMI and LDL levels in the diet-only group. Notably, both groups regained weight 9 months after the intervention [33]. Evidence suggests energy-restricted diets improve the weight status of children and adolescents, regardless of the macronutrient proportions [35][36][35,36]. Thus, focusing on the attainment of sustained adherence to a balance and varied diet is more important than the type of macronutrients’ alteration for successful weight loss. In order to help children embrace recommended eating patterns, reswearchers could involve them in meal planning, shopping, gardening and the preparation of food. However, diet modification alone is not sufficient to achieve weight loss. When caloric intake decreases, metabolism slows, resulting in decreased calorie utilization and difficulty achieving weight loss. That is why physical activity is vital for successful weight loss [37].3.2. Physical Activity
There is robust evidence regarding the benefits of regular physical activity in childhood and adolescence with a wide range of effects, such as motor skills’ development, healthy weight and body composition enhancement, and bone and muscular development. Moreover, physical activity improves cardio respiratory capacity, cardiovascular and metabolic health biomarkers, immunity and quality of life [38]. Thus, it is a main component of all weight-management programs, particularly in the phase of weight maintenance. Weight loss induced by diet escalates appetite and energy intake by increasing ghrelin and reducing insulin and leptin levels, whereas exercise adapts the metabolism and improves energy balance regulation [39]. When children and adolescents with obesity participated in a 30 to 60 min physical activity program for 3 to 7 days a week, total body fat and visceral adiposity were reduced; the same program had no effect on the body fat of normal-weight participants [40]. The results of further studies are inconclusive; some studies report a significant decrease [41] and others report no change in adiposity [42]. Although physical fitness’s (PF) role in weight loss remains uncertain, its benefits for overall health are unequivocal. Thus, the existing literature indicates that increasing the level of PF dampens the metabolic consequences associated with excess adiposity and has positive effects on mental and skeletal health [43]. Moreover, physical activity dampens the obesity-related inflammatory state, promoting an increase in adiponectin levels and a decrease in both C-reactive protein (CRP) and Interleukin-6 (IL-6) levels [7], regardless of the associated weight loss or body composition changes [44][47]. Finally, even without weight loss, exercise improves or even normalizes flow-mediated dilation (FMD) and intima media thickness (IMT). Both abnormal FMD and IMT are well-documented indicators of the initiation of atherosclerosis, reflecting arterial function and vascular wall structure, respectively [45][48]. A physically active lifestyle appears to halt subclinical atherosclerotic vascular changes in healthy adolescents and can improve arterial function and structure in children with cardiovascular risk factors [46][49]. Although aerobic and resistance training similarly decrease body fat, only resistance exercise accelerates insulin sensitivity significantly [47][50]. Notably, combined aerobic and resistance training shows superior effectiveness than either alone in improving various adiposity measures (e.g., BMI, total body fat), fasting glucose levels, metabolic profile and adiponectinemia [48][51]. Additionally, in a group of adolescent females, high-intensity exercise had a greater positive effect on blood lipids, adiponectin levels and insulin sensitivity than moderate-intensity exercise [49][52]. Thus, although the beneficial effects of exercise are indisputable, the ideal weight-loss exercise program has not been established so far.3.3. Diet Plus Exercise
Since the implementation of single-treatment options to improve weight status and BMI has limited results, exercise combined with diet and behavioral adaptations is regarded by most experts as optimal for weight loss [50][58]. Dietary restriction along with physical exercise act synergistically to decrease body mass while maintaining an unchanged resting energy expenditure [51][52][53][54][55][56][57][58][53,54,55,56,57,59,60,61]. For example, following a 12–24 month intervention, a decrease in BMI z-score ranging from 0.05 to 0.42 was observed [57][60]. On the contrary, a review of randomized controlled trials suggested that combined lifestyle modification interventions may lead to small, short-term decreases in BMI and weight in school-aged children [58][61]. However, maintenance of the same weight with linear growth in children means a reduction in BMI, as well as an improvement in cardiovascular risk factors [59][62]. Lifestyle modifications have particularly limited longer-term results among adolescents with severe obesity [60][63]. A structured, comprehensive, multidisciplinary and personalized lifestyle intervention program of healthy diet and physical exercise for one year resulted in a significant increase in leukocyte telomere length in children and adolescents, irrespective of gender, pubertal status or BMI, as well as a significant improvement in metabolic syndrome parameters, including clinical and body composition indices of obesity, inflammatory markers, hepatic enzymes, markers of insulin resistance and lipid profile [61][64]. A recent meta-analysis of lifestyle interventions outcomes confirmed the positive effects of diet and diet plus exercise on weight, blood pressure and metabolic parameters such as LDL cholesterol, triglycerides and fasting insulin for up to one year [62][65]. When diet and diet plus exercise were compared, a greater reduction in triglycerides and LDL levels with diet and a greater improvement in HDL, fasting glucose and insulin levels with diet plus exercise were shown. Favorable effects of diet plus exercise or exercise alone on endothelial function and cardiovascular risk factors, including blood pressure, lipid profile, insulin resistance, metabolic syndrome and inflammatory status, have also been reported. However, the efficacy of lifestyle interventions appears to depend on the age of the patient at initiation and the severity of obesity. Specifically, although behavioral treatment was effective for children with moderate and severe obesity, it had no significant effect for adolescents with severe obesity [63][66]. A recent study highlighted young age at treatment onset as the most important predictive factor for weight reduction, underlining the value of early interventions as the cornerstone for children’s natural growth and weight-related habits [64][67]. Importantly, lifestyle interventions do not carry the risk of serious side-effects or health inequalities [65][68]. Therefore, obesity should be addressed at the earliest time point in life.
