Uterine fibromas are the most common benign uterine tumors. Although the majority of leiomyomas remain asymptomatic, they can cause serious clinical problems, including abnormal uterine bleeding, pelvic pain, and infertility, which require effective gynecological intervention. Depending on the symptoms as well as patients’ preferences, various treatment options are available, such as medical therapy, non-invasive procedures, and surgical methods. Regardless of the extent of the surgery, the preferred option is the laparoscopic approach. To reduce the risk of spreading occult malignancy and myometrial cells associated with fragmentation of the specimen before its removal from the peritoneal cavity, special systems for laparoscopic contained morcellation have been developed.
- contained morcellation
- retrieval bag
- tissue dissemination
- myoma
- laparoscopy
1. Introduction
2. State of the Art
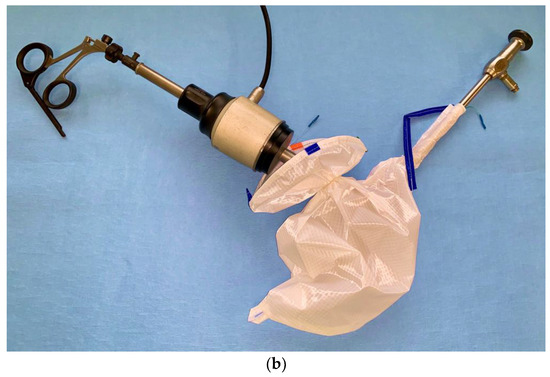
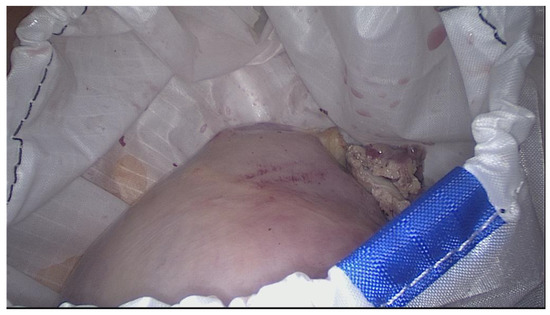
Currently, the most frequently used are the second-generation containers, called two-port or dual opening bags. They are usually made of polyurethane or polyurethane-coated nylon fabric [62,64,65][32][33][34]. This material is inflatable, impermeable for cells and water, not inflammable, and resistant to thermal effects caused by cold light exposure. The majority of the bags are transparent, which increases the safety of the procedure. Transparency allows simultaneous visual control of the bag content and the surrounding abdominal structures. Thanks to this bag wall property, the operating surgeon can continue the morcellation while being perfectly aware of the neighboring tissues and maintaining the appropriate protective distance from them [62][32]. The contemporary bags are rectangular or stomach shaped. The typical dual opening bag has two separate ports (Figure 1).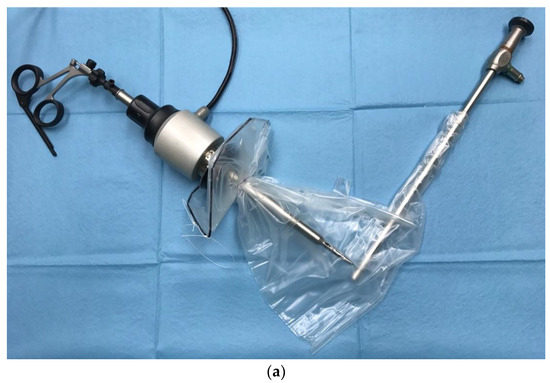

3. Impact of the Bag Use on the Course of the Operation
Introducing the new bag systems to the routine surgical practice was preceded by thorough preclinical evaluation of its ability to diminish the risk of fluid and cell dissemination during the surgical procedures. The properties of the bag material were first tested in vitro, where the morcellation of animal tissue in a laparoscopy training set was performed with the usage of typical laparoscopic instrumentarium [62][32].
To objectively assess the practical utility of a retrieval bag and the impact of contained morcellation on the entire course of the operation, numerous aspects of the procedure and its specific phases must be taken into consideration. They involve in particular:-
Insertion of the retrieval bag into the peritoneal cavity;
-
Deployment of the bag;
-
Positioning of the bag inside the abdominal cavity;
-
Positioning the specimen into the bag;
-
Large-opening exterioration;
-
Exterioration of the optic sleeve;
-
Insertion of the umbilical trocar;
-
Establishing the pseudoperitoneum;
-
Introduction of the telescope into the inflated bag;
-
Initial and continuous in-bag visualization;
-
Insertion of the morcellation device;
-
Manipulation of the specimen within the bag to find the optimal position for morcellation;
-
Course of the in-bag morcellation;
-
Morcellation-associated complications;
-
Uncontaminated closing of the optic sleeve;
-
Removal of the bag;
-
Damage of the containment bag;
-
Occurrence of any organ damage related to bag use;
-
Other intraoperative complications;
-
Time necessary to conduct particular steps of the procedure;
-
Overall satisfaction of the operating doctor.
4. Conclusions
Minimally invasive approaches, especially the laparoscopic technique, have significantly changed contemporary gynecology and are currently considered the “gold standard” in uterine fibroids surgery. Power morcellators were developed as a response to the requirement for special techniques to remove the specimen from the abdominal cavity inherent in the use of minimally invasive access. A 2014 FDA safety communication discouraged the routine use of open morcellation, given concerns for iatrogenic dissemination of a previously undiagnosed malignancy. Despite the unresolved issue of the occurrence and significance of this phenomenon, and even existing doubts whether a myoma can develop or transform into a sarcoma, all possible measures must be taken to optimize patient safety. Contained morcellation is considered to be one such solution that reduces the potential intraabdominal spread of undetected malignancy and myometrial cells, while simultaneously maintaining the benefits of a minimally invasive surgical approach.References
- Lumsden, M.-A. Modern management of fibroids. Obstet. Gynaecol. Reprod. Med. 2013, 23, 65–70.
- Marsh, E.E.; Ekpo, G.E.; Cardozo, E.R.; Brocks, M.; Dune, T.; Cohen, L.S. Racial differences in fibroid prevalence and ultrasound findings in asymptomatic young women (18–30 years old): A pilot study. Fertil. Steril. 2013, 99, 1951–1957.
- Segars, J.H.; Parrott, E.C.; Nagel, J.D.; Guo, X.C.; Gao, X.; Birnbaum, L.S.; Pinn, V.W.; Dixon, D. Proceedings from the Third National Institutes of Health International Congress on Advances in Uterine Leiomyoma Research: Comprehensive review, conference summary and future recommendations. Hum. Reprod. Update 2014, 20, 309–333.
- Leyland, N.; Leonardi, M.; Murji, A.; Singh, S.S.; Al-Hendy, A.; Bradley, L. A Call-to-Action for Clinicians to Implement Evidence-Based Best Practices When Caring for Women with Uterine Fibroids. Reprod. Sci. 2022, 29, 1188–1196.
- Downes, E.; Sikirica, V.; Gilabert-Estelles, J.; Bolge, S.C.; Dodd, S.L.; Maroulis, C.; Subramanian, D. The burden of uterine fibroids in five European countries. Eur. J. Obstet. Gynecol. Reprod. Biol. 2010, 152, 96–102.
- Pritts, E.A.; Parker, W.H.; Olive, D.L. Fibroids and infertility: An updated systematic review of the evidence. Fertil. Steril. 2009, 91, 1215–1223.
- Stewart, E.A. Clinical practice. Uterine fibroids. N. Engl. J. Med. 2015, 372, 1646–1655.
- Baumgarten, M.N.; Polanski, L.T. Modern management of fibroids. Obstet. Gynaecol. Reprod. Med. 2020, 30, 104–108.
- Kashani, B.N.; Centini, G.; Morelli, S.S.; Weiss, G.; Petraglia, F. Role of Medical Management for Uterine Leiomyomas. Best Pract. Res. Clin. Obstet. Gynaecol. 2015, 34, 85–103.
- Giuliani, E.; As-Sanie, S.; Marsh, E.E. Epidemiology and management of uterine fibroids. Int. J. Gynecol. Obstet. 2020, 149, 3–9.
- Gupta, J.K.; Sinha, A.; Lumsden, M.A.; Hickey, M. Uterine artery embolization for symptomatic uterine fibroids. Cochrane Database Syst. Rev. 2014.
- de Bruijn, A.M.; Ankum, W.M.; Reekers, J.A.; Birnie, E.; van der Kooij, S.M.; Volkers, N.A.; Hehenkamp, W.J. Uterine artery embolization vs hysterectomy in the treatment of symptomatic uterine fibroids: 10-year outcomes from the randomized EMMY trial. Am. J. Obstet. Gynecol. 2016, 215, 745.e1–745.e12.
- Han, N.-L.R.; Ong, C.L. Magnetic Resonance-Guided Focused Ultrasound Surgery (MRgFUS) of Uterine Fibroids in Singapore. Ann. Acad. Med. Singap. 2014, 43, 550–558.
- Chang, C.-T.; Jeng, C.-J.; Long, C.-Y.; Chuang, L.T.; Shen, J. High-intensity focused ultrasound treatment for large and small solitary uterine fibroids. Int. J. Hyperth. 2022, 39, 485–489.
- Huang, Y.; Zhou, S.; Wang, J.; Pang, Z. Efficacy and safety of magnetic resonance-guided focused ultrasound surgery (MRgFUS) ablation in the management of abnormal uterine bleeding due to uterine leiomyoma or adenomyosis. Am. J. Transl. Res. 2022, 14, 656–663.
- Levens, E.D.; Wesley, R.; Premkumar, A.; Blocker, W.; Nieman, L.K. Magnetic resonance imaging and transvaginal ultrasound for determining fibroid burden: Implications for research and clinical care. Am. J. Obstet. Gynecol. 2009, 200, 537.e1–537.e7.
- Steiner, R.A.; Wight, E.; Tadir, Y.; Haller, U. Electrical cutting device for laparoscopic removal of tissue from the abdominal cavity. Obstet. Gynecol. 1993, 81, 471–474.
- Bogani, G.; Cliby, W.A.; Aletti, G.D. Impact of morcellation on survival outcomes of patients with unexpected uterine leiomyosarcoma: A systematic review and meta-analysis. Gynecol. Oncol. 2015, 137, 167–172.
- Tan-Kim, J.; Hartzell, K.A.; Reinsch, C.S.; O’day, C.H.; Kennedy, J.S.; Menefee, S.A.; Harrison, T.A. Uterine sarcomas and parasitic myomas after laparoscopic hysterectomy with power morcellation. Am. J. Obstet. Gynecol. 2015, 212, 594.e1–594.e10.
- Parker, W.H.; Fu, Y.S.; Berek, J.S. Uterine sarcoma in patients operated on for presumed leiomyoma and rapidly growing leiomyoma. Obstet. Gynecol. 1994, 83, 414–418.
- Rowland, M.; Lesnock, J.; Edwards, R.; Richard, S.; Zorn, K.; Sukumvanich, P.; Krivak, T. Occult uterine cancer in patients undergoing laparoscopic hysterectomy with morcellation. Gynecol. Oncol. 2012, 127, S29.
- Multinu, F.; Casarin, J.; Tortorella, L.; Huang, Y.; Weaver, A.; Angioni, S.; Melis, G.B.; Mariani, A.; Stewart, E.A.; Laughlin-Tommaso, S.K. Incidence of sarcoma in patients undergoing hysterectomy for benign indications: A population-based study. Am. J. Obstet. Gynecol. 2018, 220, 179.e1–179.e10.
- Seidman, M.A.; Oduyebo, T.; Muto, M.G.; Crum, C.P.; Nucci, M.R.; Quade, B.J. Peritoneal Dissemination Complicating Morcellation of Uterine Mesenchymal Neoplasms. PLoS ONE 2012, 7, e50058.
- Food and Drug Administration. Quantitative assessment of the prevalence of unsuspected uterine sarcoma in women undergoing treatment of uterine fibroids. Summ. Key Find. 2014, 17.
- Siedhoff, M.T.; Wheeler, S.B.; Rutstein, S.E.; Geller, E.J.; Doll, K.M.; Wu, J.M.; Clarke-Pearson, D.L. Laparoscopic hysterectomy with morcellation vs abdominal hysterectomy for presumed fibroid tumors in premenopausal women: A decision analysis. Am. J. Obstet. Gynecol. 2015, 212, 591.e1–591.e8.
- Chen, Q.; Shi, H.; Lu, W.; Lu, B. Unexpected uterine sarcomas in 4478 patients with electric power morcellation for leiomyomas. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 230, 85–89.
- Einstein, M.H.; Barakat, R.R.; Chi, D.S.; Sonoda, Y.; Alektiar, K.M.; Hensley, M.L.; Abu-Rustum, N.R. Management of uterine malignancy found incidentally after supracervical hysterectomy or uterine morcellation for presumed benign disease. Int. J. Gynecol. Cancer 2008, 18, 1065–1070.
- Oduyebo, T.; Rauh-Hain, A.J.; Meserve, E.E.; Seidman, M.A.; Hinchcliff, E.; George, S.; Quade, B.; Nucci, M.R.; Del Carmen, M.G.; Muto, M.G. The value of re-exploration in patients with inadvertently morcellated uterine sarcoma. Gynecol. Oncol. 2013, 132, 360–365.
- Anupama, R.; Ahmad, S.Z.; Kuriakose, S.; Vijaykumar, D.; Pavithran, K.; Seethalekshmy, N. Disseminated Peritoneal Leiomyosarcomas After Laparoscopic “Myomectomy” and Morcellation. J. Minim. Invasive Gynecol. 2011, 18, 386–389.
- Della Badia, C.; Karini, H. Endometrial Stromal Sarcoma Diagnosed after Uterine Morcellation in Laparoscopic Supracervical Hysterectomy. J. Minim. Invasive Gynecol. 2010, 17, 791–793.
- Rekha, W.; Amita, M.; Sudeep, G.; Hemant, T. Unexpected complication of uterine myoma morcellation. Aust. N. Z. J. Obstet. Gynaecol. 2005, 45, 248–249.
- Rimbach, S.; Holzknecht, A.; Nemes, C.; Offner, F.; Craina, M. A new in-bag system to reduce the risk of tissue morcellation: Development and experimental evaluation during laparoscopic hysterectomy. Arch. Gynecol. Obstet. 2015, 292, 1311–1320.
- Steller, C.; Cholkeri-Singh, A.; Sasaki, K.; Miller, C.E. Power Morcellation Using a Contained Bag System. JSLS J. Soc. Laparosc. Robot. Surg. 2017, 21, e2016.00095.
- Devassy, R.; Cezar, C.; Krentel, H.; Verhoeven, H.C.; Devassy, R.; de Wilde, M.S.; Torres-de la Roche, L.A.; de Wilde, R.L. Feasibility of myomatous tissue extraction in laparoscopic surgery by contained in–bag morcellation: A retrospective single arm study. Int. J. Surg. 2019, 62, 22–27.
- Rimbach, S.; Holzknecht, A.; Schmedler, C.; Nemes, C.; Offner, F. First clinical experiences using a new in-bag morcellation system during laparoscopic hysterectomy. Arch. Gynecol. Obstet. 2015, 294, 83–93.
- Rimbach, S.; Schempershofe, M. In-Bag Morcellation as a Routine for Laparoscopic Hysterectomy. BioMed Res. Int. 2017, 2017, 6701916.
- Anapolski, M.; Panayotopoulos, D.; Alkatout, I.; Soltesz, S.; Mettler, L.; Schiermeier, S.; Hatzmann, W.; Noé, G. Power morcellation inside a secure endobag: A pilot study. Minim. Invasive Ther. Allied Technol. 2016, 25, 203–209.
- Feghali, E.J.; Laganà, A.S.; Daccache, A.; Bitar, R.; Garzon, S.; Uccella, S.; Petousis, S.; Sleiman, Z. Endobag use in laparoscopic gynecological surgeries: A systematic review. Minim. Invasive Ther. Allied Technol. 2021, 31, 698–703.
- Obrzut, B.; Wasyluk, T.; Obrzut, M.; Sozanski, B.; Darmochwal-Kolarz, D.; Rimbach, S. Laparoscopic in-bag morcellation—A comparison of two tissue extraction systems. Ginekol. Polska 2022, 93, 369–373.
- Paul, P.; Thomas, M.; Das, T.; Patil, S.; Garg, R. Contained Morcellation for Laparoscopic Myomectomy Within a Specially Designed Bag. J. Minim. Invasive Gynecol. 2016, 23, 257–260.
- Gil-Gimeno, A.; Laberge, P.Y.; Lemyre, M.; Gorak, E.; Maheux-Lacroix, S. Morcellation During Total Laparoscopic Hysterectomies: Implications of the Use of a Contained Bag System. J. Obstet. Gynaecol. Can. 2020, 42, 839–845.
- Trivedi, P.H.; Trivedi, S.; Patil, S. Laparoscopic In-Bag Morcellation Compared with Conventional Morcellation of Myomas and Uterus with Myomas. J. Obstet. Gynecol. India 2019, 70, 69–77.
- Krentel, H.; Tchartchian, G.; de la Roche, L.T.; De Wilde, R. Total surgical time in laparoscopic supracervical hysterectomy with laparoscopic in-bag-morcellation compared to laparoscopic supracervical hysterectomy with uncontained morcellation. Facts, Views Vis. ObGyn 2022, 14, 59–68.
 Encyclopedia
Encyclopedia
