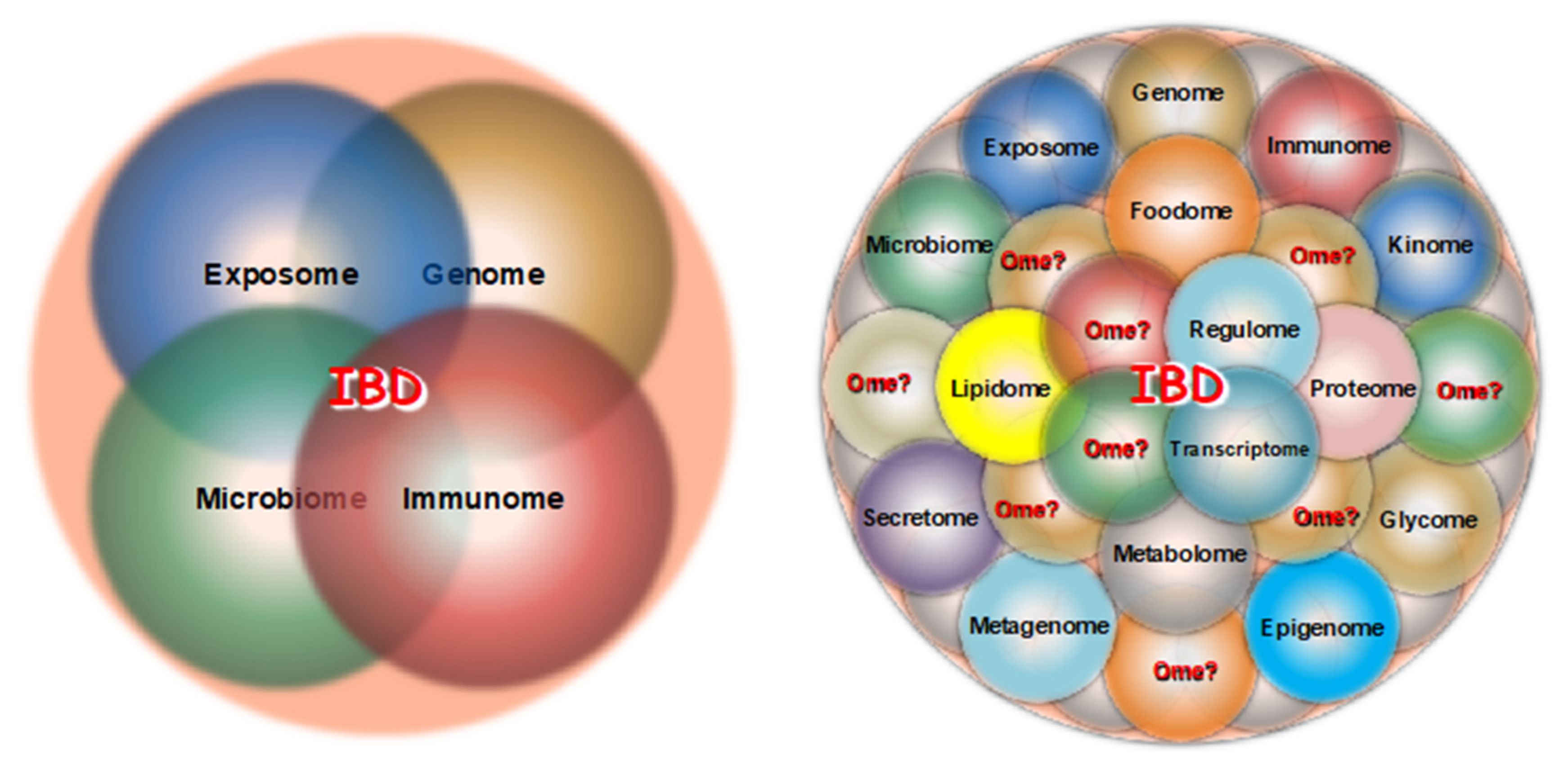
The notion and importance of omes, omics and multi-omics in both health and complex diseases like inflammatory bowel disease (IBD) is introduced, followed by a discussion of the various omics believed to be relevant to IBD pathogenesis, and how multi-omics “big data” can generate new insights translatable into useful clinical tools in IBD such as biomarker identification, prediction of remission and relapse, response to therapy, and precision medicine.
- inflammatory bowel disease
- ulcerative colitis
- Crohn’s disease
- omics
- multi-omics
- systems biology
- network medicine
- artificial intelligence
1. Introduction
2. Omes, Omics and Multi-Omics
Essentially all diseases, even those not formally pertaining to the category of “complex diseases”, are multifaceted because of the huge amount of varied interconnected biological components and events involved in their pathophysiology [7]. With the appreciation of the innumerable components of any disease came the realization that the study of any single component in isolation would never solve the intricacies of the underlying biology. From the above realization emerged the need to study all components in a far more comprehensive way, hence the emphasis on “omes” and “omics”, defined, respectively, as the totality of any particular field and their study. Although the analysis of single omics can provide relevant information, the integration of several omics, i.e., “multi-omics”, allows a much more comprehensive view of the mechanisms underlying any disease [8,9][8][9]. All of the omes believe to be involved in inflammatory bowel disease (IBD) are highly complex and variable [10[10][11],11], and the investigation of any ome alone can barely open a narrow window into the intricate mechanisms underlying ulcerative colitis (UC) or Crohn’s disease (CD). This is as well exemplified by the numerous but insular genomics studies of IBD, where early and subsequent massive DNA sequencing analysis from several thousand patients identified hundreds of common and rare genetic variants associated with CD or UC without generating clear-cut or definitive clues to their etiology, pathogenesis, classification, diagnosis or therapy [12,13,14][12][13][14]. In fact, no clinically useful IBD genetic markers have been identified so far, not even for the variants of NOD2 that are closely associated with ileal CD at the clinical level without influencing the response to therapy [15,16,17][15][16][17]. After a plethora of reports on the genetics of IBD, there is still no evidence that assessing genetic factors independently of other contributing factors can provide a practical guide for diagnosis or therapy of CD or UC [17]. Given this evidence, and the vast amount of literature available to the reader, the topic of genomics will not be specifically addressed in this revisewarch. However, to gain a truly comprehensive understanding of IBD, it is still mandatory to include the genome in combination with other omes, hence the need for “multi-omics” studies carried out with integrative computational methodologies [18].3. Multi-Omics in Health
While the complexity of any disease status is an accepted reality, it is often forgotten that health is also an extremely complex condition [19]. The maintenance of health, with all the endless challenges imposed by growth, environmental factors, adaptation, nutrition, metabolism, immunity, behavior, and mental and physical demands, requires a perfect coordination of innumerous physiological functions and their respective omes [9]. However, the study of health multi-omics lags far behind that of disease multi-omics, hindering and delaying a better understanding of pathophysiological events resulting from the derangements of healthy omes [20,21,22][20][21][22]. The advent of multi-omics is connected to and strictly dependent on new technologies that allow a detailed molecular analysis of omes [23]. The best example is the use of next-generation sequencing (NGS) of DNA with the purpose of defining the complete human genome with its many variants [24]. Sequencing platforms are now used to dissect the epigenome, transcriptome and metagenome, while mass spectroscopy platforms are used to study the proteome and the metabolome [25]. However, it is essential that all omes relevant to both health and disease are studied in a coordinated and integrated way, a fundamental point that will be discussed in greater detail later on in this revisewarch.4. Multi-Omics in Complex Diseases
The field of oncology has pioneered most of the omics technologies used for the investigation of complex diseases. Starting in 2006, The Cancer Genome Atlas (TCGA) research network, with the participation of investigators worldwide, has profiled 33 different types of human tumors and discovered numerous molecular abnormalities at the DNA, RNA, protein and epigenetic level associated with distinct cancer types [26]. This landmark approach launched what has now become the conventional approach to studying multiple non-cancerous complex diseases in various human organs and systems. Regrettably, progress with these autoimmune or chronic inflammatory diseases has been much slower than with cancer due to lack of universal coordination and collaboration and more limited resources. Nonetheless, numerous reports of omics or multi-omics studies have been published for a variety of diseases, like rheumatoid arthritis, systemic lupus erythematosus, asthma, chronic obstructive pulmonary disease, and even irritable bowel syndrome and autism [27,28,29,30,31,32][27][28][29][30][31][32]. It should be kept in mind that these complex diseases occur in vastly different organs and tissues that have their own tissue-specific regulatory circuits in both health and disease, and these differences will be reflected in the respective multi-omics analyses [33].5. Multi-Omics in IBD
The importance of omics in intestinal inflammation and their potential for advancing disease understanding, biomarker discovery and new therapies have been recognized since the mid-2000s [34], but the appreciation of omics by the medical community has been sluggish and only recently have studies begun to be undertaken and generate some tangible results. Though not to the same degree of the TCGA network, efforts to create working groups for the global study of omics and multi-omics in IBD have also been made, like the 1000IBD project (https://1000ibd.org, accessed on 10 August 2023) [35]. The project recruits and prospectively follows adult patients with new or existing IBD of different phenotypes and collects information about several omes (exposome, genome, transcriptome and metagenome, drug response, etc.). The 1000IBD project has generated a number of publications on various topics, like the modulation of intestinal gene expression by inflammation [36], the association of dietary patterns with selective features of the gut microbiota [37], the impact of drugs on gut microbiota composition and function [38], the identification of environmental factors linked to IBD development [39], the association of IBD genotypes and phenotypes with the plasma proteome [40], as well as reviews on multi-omic data availability in IBD [41], and several other aspects of IBD pathophysiology. Another similar but more recent group initiative is the European ImmUniverse Consortium (https://www.imi.europa.eu/projects-results/project-factsheets/immuniverse, accessed on 8 January 2019) which was formed to create a multi-omics integrative approach to personalized medicine in immune-mediated inflammatory diseases, including IBD [42]. Several other IBD omics-oriented initiatives are also under way worldwide [43]. However, the vast majority of reports on IBD multi-omics are still the result of work carried out by individual investigators and, whether as reviews or original reports, have substantially expanded UC and CD omics information on a wide variety of topics. Reviews tend to emphasize the importance of multi-omics in IBD for the goal of delivering more effective treatment [44] or precision medicine to UC and CD patients [45[45][46],46], or the potential of multi-omics to identify predictive biomarkers for the discovery of IBD risk factors [47], while other reviews call attention to the numerous challenges of designing and analyzing multi-omics IBD data [48]. The number of omics reported in the literature at large or listed in formal databases is large (Table 1). However, what omics are relevant to IBD, to what degree, which ones should be prioritized for study, which ones should be functionally integrated, and which omes research should be ourthe main focus is a critical and unresolved issue.|
Type of Ome |
Field of Study (Omics) |
Type of Ome |
Field of Study (Omics) |
Type of Ome |
Field of Study (Omics) |
|---|---|---|---|---|---|
|
Allergernome |
Allergernomics |
Immunome |
Immunomics |
Pharmacogenetics |
Pharmacogenetics |
|
Bibliome |
Bibliomics |
Interferome |
Interferomics |
Phenome |
Phenomics |
|
Connectome |
Connectomics |
Interactome |
Interactomics |
Physiome |
Physiomics |
|
Cytome |
Cytomics |
Ionome |
Ionomics |
Phytochemome |
Phytochemomics |
|
Diseasome |
Medicine |
Kinome |
Kinomics |
Proteome |
Proteomics |
|
Editome |
RNA editing |
Lipidome |
Lipidomics |
Regulome |
Regulomics |
|
Embryome |
Embryomics |
Mechanome |
Mechanomics |
Researchsome |
Research areas |
|
Envirome |
Enviromics |
Metabolome |
Metabolomics |
Secretome |
Secretomics |
|
Epigenome |
Epigenomics |
Metagenome |
Metagenomics |
Speechome |
Speechomics |
|
Exposome |
Exposomics |
Metallome |
Metallomics |
Toponome |
Toponomics |
|
Foodome |
Foodomics |
Microbiome |
Microbiomics |
Transcriptome |
Transcriptomics |
|
Genome |
Genomics |
Obesidome |
Obesidomics |
Trihalome |
Medicine |
|
Glycome |
Glycomics |
ORFeome |
ORFeomics |
Volatilome |
Volatilomics |
|
Holgenome |
Holgenomics |
Organome |
Organomics |
Etc. |
Etc. |
5.1. Exposomics
The study of the environmental factors (the exposome) as they related to IBD overall, or IBD pathogenesis in particular, is the most difficult and problematic because of the endless number of factors involved, their multiplicity of actions, the constant generation of new man-made substances that permeate the environment at large and modify the exposome, the individuality of the exposure process by humans and the unique response of each person [49,50,51][49][50][51]. Reports and reviews on the assumed or demonstrable impact of environmental risk factors in IBD are plentiful [39,52[39][52][53],53], but it is logistically and practically impossible to identify all relevant factors in each IBD patient and derive usable omics data to be factored in for multi-omics integration.5.2. Microbiomics
The importance of the gut microbiome to IBD pathogenesis has been long established [54] and progressively explored in greater depth with the adoption of metagenomic analyses [55]. Studies analyzing the composition and function of the gut microbiota in UC or CD patients are numerous, but when performed in isolation they have generated unclear and inconsistent results [56]. However, metagenomic analyses of the gut microbiome combined with other omes can result in more relevant information about the role of microbes in the pathobiology of IBD. For instance, a study performed as part of the Human Functional Genomics Project explored the combination and functional relationship of multi-omic microbial and cytokine profiles and found a link between the human gut microbiome and inflammatory cytokine production [57]. Using longitudinally collected blood, stools and biopsy samples, an IBD multi-omics (metagenome, metatranscriptome, proteome, metabolome, and virome) database has been created, revealing that patient disease activity is marked by temporal increases and shifts in taxonomy, as well as functional and biochemical composition [58]. The combination of metagenomics, metatranscriptomics and metaproteomics can uncover multiple microbial bioactive molecules likely to interact with the host immune system in IBD, and inform us about the broad and dynamic host–microbial interactions involved in IBD pathogenesis [59]. While enlightening and exciting, all results of microbiomics reports must be interpreted with caution in view of the extensive impact of genetics [60], lifestyle [61], nutrition [62], immunity [63], common drugs or drugs used to treat IBD patients [38,64][38][64] on gut microbiota composition and function.5.3. Immunomics
Immunology has dominated the study of IBD for a long time, and only in the last decade or so has its dominance partially diminished due to a growing interest in the gut microbiota and other non-immune factors in IBD pathogenesis [65]. The key role of the immune response in IBD is unquestionable, but this response is influenced by a myriad of factors such as the host, environment, genes, microbes, nutrition, behavior, season of the year, stress, etc. [51,57,63,66,67][51][57][63][66][67]. This multiplicity of unpredictable and uncontrollable factors puts constant demands on the immune system, which responds by continuously adapting in a vigorous way, leading to both beneficial and harmful effects [68]. This multidimensional response makes it unrealistic to expect that the immune system alone can provide reproducible and reliable markers or omics that define specific biological states in multifactorial diseases like CD or UC. A good example is a report which claimed that the transcriptional signature of circulating CD8+ T cells could predict the disease course of patients with CD and UC [69], a claim that could not be reproduced in a subsequent study [70]. These contrasting results are likely be due to the plasticity of CD8+ T cells in IBD [71], a quality inherent to all immune cells residing in specific tissue microenvironments [72], which makes them and their products, like cytokines, essentially impossible to use as predictable and reproducible qualitative or quantitative measurements of any immune response [73]. Fundamental abnormalities of the immune response are clearly involved in the pathogenesis of UC and CD and, considering the variability and unpredictability of the immune response, such abnormalities cannot be evaluated in isolation, but integrated with multiple other omes under the umbrella of the modern comprehensive notion of the IBD interactome [74].5.4. Epigenomics
The field of epigenetics, variably defined as DNA-independent changes in gene expression or the transgenerational effects and/or inherited expression states [75], is a more recently and relatively less investigated omic in IBD [76], but it is of crucial importance because of the link it establishes between genes and the exposome [77]. Intestinal biopsies obtained from pediatric CD and UC patients submitted to combined DNA methylation and transcription analyses were able to identify disease subtypes and an association with clinical outcome [78]. A study by Kalla et al. performed multi-omic integration of the methylome, genome and transcriptome measured in the peripheral blood of UC and CD patients and identified multiple differentially methylated positions in IBD with an association with treatment escalation or need for surgery [79]. The latter group of investigators recently reported a differential and variable methylation in CD patients developing clinical recurrence after surgery [80]. The study of epigenetics in IBD is now attracting more and more attention, but it also must be considered in the context of interactions with the genome and the exposome [81].5.5. Proteomics, Metabolomics, Lipidomics
The possibility of using serum proteomics for biomarker discovery in IBD has been considered for a long time [82], and this approach, particularly when combined with metabolomics and lipidomics, could help us to discover complementary biomarkers, monitor and predict response to therapy and promote personalized medicine [83,84][83][84]. The combined alterations in serum lipids, amino acids and energy metabolites have been reported to distinguish UC from CD and healthy controls [85], while a study by Fan et al. compared plasma lipid profiles in UC vs. CD patients and found that a number of ether lipids were negatively associated with CD [86]. Another study reported that neither metagenomic or host genetics could distinguish ileal and colonic CD, but this could be accomplished via metabolomics and metaproteomics analyses using mass spectroscopy [87].5.6. Single-Cell Technologies, Omics, Multi-Omics and Spatial Multi-Omics
With the progress prompted by the development of many new cellular and molecular tools complemented by the even more rapid deployment of artificial intelligence, machine and deep learning analytical methods, the possibility of studying omics and multiomics at the single-cell level has become an exciting reality [88]. An enormous amount of literature has rapidly accumulated on single cell omics, multi-omics and spatial transcriptomics in different cells and organs. Initial studies focused primarily on single-cell transcriptomics [89[89][90],90], resulting in the universal and fundamental discovery of an unsuspected extreme degree of cell heterogeneity of both immune [91,92][91][92] and non-immune cells [93,94][93][94] in essentially all tissues, including the gastrointestinal tract [95,96,97][95][96][97]. These reports were then followed by single-cell multi-omics studies in which the genome, epigenome, transcriptome, proteome, or other omes could be assessed in the same cells [88] and the subsequent investigation of single-cell multi-omics, i.e., the detection and topographical mapping of multiple omes in specific tissue types [98] in both normal and inflamed tissues [99]. The field of single cell analysis, omics and multi-omics is still evolving very rapidly and in the near future, reference maps of the whole human body will become available with an unprecedented level of cellular and molecular precision [100]. In the field of gastroenterology and IBD in particular, similar studies have emerged that also show vast single cell heterogeneity in immune and epithelial cells in both UC and CD [101,102,103][101][102][103]. Recently, additional studies have appeared describing fibroblast heterogeneity and cellular interactions of a full thickness single-cell transcriptomic atlas of the strictured CD intestine [104], and the single-cell spatial proteomics and transcriptomics analysis of colonic biopsies of patients with UC receiving treatment with vedolizumab [105].6. Clinical Applications of Multi-Omics Analyses
The primary goal behind the study of multi-omics in IBD is the discovery of novel tools that afford more precise diagnostic and management means at the bedside. Based on this very desirable goal, a large and growing number of studies have been and are still being published which claim that the utilization of multi-omics and their different combinations can help with the discovery of basic, translational, and clinical elements of UC and CD. The execution of these studies is justifiable and the results are of interest. However, most of the claims so far made must be carefully assessed and interpreted in the light of more stringent criteria, as discussed later under the subtitle Pitfalls and Limitations of Current IBD Multi-omics Studies.6.1. Biomarker Identification
The quest to identify disease biomarkers is as old as the field of medicine. The popular biomarkers commonly used for the evaluation of UC and CD patents, like C reactive protein and fecal calprotectin, are not true disease biomarkers as they simply reflect the process of inflammation and its degree, but are not specific and their levels increase as a result of many other conditions [106]. The same can be said for serological biomarkers, whose combined evaluation is of uncertain value for the prediction of disease progression or response to treatment [107]. In 2016, the National Institutes of Health (NIH) and the Food and Drug Administration (FDA) created the FDA-NIH Biomarker Working Group with the goal of better defining what is intended for “biomarker” and their many types; this was last updated in 2021 [108]. The FDA-NIH working group identified the following types of biomarkers: susceptibility/risk, predictive, diagnostic, monitoring, pharmacodynamic/response, safety, prognostic as well as “reasonably likely surrogate endpoints” [108]. In principle, all of them are of interest in IBD and the topic has generated a great deal of attention and a huge volume of publications [109]. The possibility of biomarker discovery using omics and multi-omics approaches has been a goal for multiple inflammatory and neoplastic conditions [110,111[110][111][112][113][114],112,113,114], including IBD [115], but so far precise and definitive biomarkers have yet to be found.6.2. Prediction of Remission and Relapse
The identification of biomarkers that predict clinical relapse or clinical remission of IBD patients using multi-omics profiling has been the target of numerous studies. One study based on profiling of the blood proteome, metabolome and microbiome claimed that a proinflammatory state predisposing to clinical relapse could be identified in UC and CD patients [116], while another study carried out tissue and blood plasma proteome and plasma metabolomics profiling of UC patients and concluded that biomarkers indicative of functional remission could be identified [117]. A very recent report found that certain blood protein profiles were associated with the risk of clinical relapse in patients who stopped infliximab therapy [118], a potentially useful solution to the vexing issue of when to stop this common form of biological therapy. None of these studies have been replicated or validated until now and their value remains unclear.6.3. Response to Therapy
In an early pilot study, serum proteomics were used to establish a model to predict response to infliximab treatment, with the results suggesting that response was associated with platelet metabolism [119]. A subsequent study based on prospectively collected blood and stool samples carried out metagenomic, serum metabolomic and serum proteomic measurements and found that some microbial factors affected the response of IBD patients receiving biological therapies [120]. A more recent study by Mishra et al. performed a longitudinal, blood-based multi-omics (RNAseq and genome-wide DNA methylation) study in two prospective IBD cohorts given TNF antagonists to predict therapy response, but no consistent predictive molecular signatures could be found [121]. Thus, the prediction of response to therapy in IBD patients based on results of multi-omics analyses appears to be at a preliminary stage and the results vary depending on the number and combination of the omics included in the prediction modeling. Perhaps more importantly, it still remains to be verified whether any of the newly described omics-based biomarkers are indeed better than traditional ones, like C-reactive protein [122].6.4. Precision Medicine
The implementation of precision medicine is the ultimate goal behind the study of multi-omics in complex diseases [123]. Precision medicine has many definitions, the one officially released by the NIH being one of the most comprehensive and commonly cited: “An emerging approach for disease treatment and prevention that takes into account individual variability in genes, environment, and lifestyle for each person” (www.nih.gov/precisionmedicine, accessed on 10 August 2023). The need for and importance of developing precision medicine are undeniable and have an enormous potential, but they require the integration of clinical data with multiple molecular profiles, and this is only possible with the most advanced computational methods and a close collaboration of clinicians, researchers and bioinformaticians [124]. With the advent of NGS and various other technologies that allow molecular characterization of health and disease, the quest for precision medicine in IBD has also been relying on omics and multi-omics studies for its fulfilment. This goal is extremely challenging and has yet to be achieved [125], but various publications reinforce the fundamental importance of pursuing multi-omics studies [126[126][127],127], including a recent series of state-of-the-art reports by the European Crohn’s & Colitis Organization (ECCO) [11,128,129,130][11][128][129][130].References
- Weinstein, J.N. Fishing expeditions. Science 1998, 282, 628–629.
- Amara, R. Available online: https://thevirtulab.com/what-is-amaras-law/ (accessed on 10 August 2023).
- Auffray, C.; Balling, R.; Barroso, I.; Bencze, L.; Benson, M.; Bergeron, J.; Bernal-Delgado, E.; Blomberg, N.; Bock, C.; Conesa, A.; et al. Making sense of big data in health research: Towards an EU action plan. Genome Med. 2016, 8, 71.
- Gligorijevic, V.; Malod-Dognin, N.; Przulj, N. Integrative methods for analyzing big data in precision medicine. Proteomics 2016, 16, 741–758.
- Subramanian, I.; Verma, S.; Kumar, S.; Jere, A.; Anamika, K. Multi-omics Data Integration, Interpretation, and Its Application. Bioinform. Biol. Insights 2020, 14, 1177932219899051.
- Torkamani, A.; Andersen, K.G.; Steinhubl, S.R.; Topol, E.J. High-Definition Medicine. Cell 2017, 170, 828–843.
- Iyengar, R. Complex diseases require complex therapies. EMBO Rep. 2013, 14, 1039–1042.
- Hasin, Y.; Seldin, M.; Lusis, A. Multi-omics approaches to disease. Genome Biol. 2017, 18, 83.
- Karczewski, K.J.; Snyder, M.P. Integrative omics for health and disease. Nat. Rev. Genet. 2018, 19, 299–310.
- Fiocchi, C. Inflammatory Bowel Disease: Complexity and Variability Need Integration. Front. Med. 2018, 5, 75.
- Fiocchi, C.; Dragoni, G.; Iliopoulos, D.; Katsanos, K.; Ramirez, V.H.; Suzuki, K. Results of the Seventh Scientific Workshop of ECCO: Precision Medicine in IBD-What, Why, and How. J. Crohn’s Colitis 2021, 15, 1410–1430.
- Barrett, J.C.; Hansoul, S.; Nicolae, D.L.; Cho, J.H.; Duerr, R.H.; Rioux, J.D.; Brant, S.R.; Silverberg, M.S.; Taylor, K.D.; Barmada, M.M.; et al. Genome-wide association defines more than 30 distinct susceptibility loci for Crohn’s disease. Nat. Genet. 2008, 40, 955–962.
- Jostins, L.; Ripke, S.; Weersma, R.K.; Duerr, R.H.; McGovern, D.P.; Hui, K.Y.; Lee, J.C.; Schumm, L.P.; Sharma, Y.; Anderson, C.A.; et al. Host-microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature 2012, 491, 119–124.
- Sazonovs, A.; Stevens, C.R.; Venkataraman, G.R.; Yuan, K.; Avila, B.; Abreu, M.T.; Ahmad, T.; Allez, M.; Ananthakrishnan, A.N.; Atzmon, G.; et al. Large-scale sequencing identifies multiple genes and rare variants associated with Crohn’s disease susceptibility. Nat. Genet. 2022, 54, 1275–1283.
- Abreu, M.T.; Taylor, K.D.; Ling, Y.C.; Hang, T.; Gaiennie, J.; Landers, C.J.; Vasiliauskas, E.A.; Kam, L.Y.; Rojany, M.; Papadakis, K.A.; et al. Mutations in NOD2 are associated with fibrostenosing disease in patients with Crohn’s disease. Gastroenterology 2002, 123, 679–688.
- Vermeire, S.; Louis, E.; Rutgeerts, P.; De Vos, M.; Van Gossum, A.; Belaiche, J.; Pescatore, P.; Fiasse, R.; Pelckmans, P.; Vlietinck, R.; et al. NOD2/CARD15 does not influence response to infliximab in Crohn’s disease. Gastroenterology 2002, 123, 106–111.
- McCauley, J.L.; Abreu, M.T. Genetics in diagnosing and managing inflammatory bowel disease. Gastroenterol. Clin. N. Am. 2012, 41, 513–522.
- Agamah, F.E.; Bayjanov, J.R.; Niehues, A.; Njoku, K.F.; Skelton, M.; Mazandu, G.K.; Ederveen, T.H.A.; Mulder, N.; Chimusa, E.R.; t Hoen, P.A.C. Computational approaches for network-based integrative multi-omics analysis. Front. Mol. Biosci. 2022, 9, 967205.
- López-Otín, C.; Kroemer, G. Hallmarks of health. Cell 2021, 184, 1929–1939.
- Chen, R.; Mias, G.I.; Li-Pook-Than, J.; Jiang, L.; Lam, H.Y.; Chen, R.; Miriami, E.; Karczewski, K.J.; Hariharan, M.; Dewey, F.E.; et al. Personal omics profiling reveals dynamic molecular and medical phenotypes. Cell 2012, 148, 1293–1307.
- Schüssler-Fiorenza Rose, S.M.; Contrepois, K.; Moneghetti, K.J.; Zhou, W.; Mishra, T.; Mataraso, S.; Dagan-Rosenfeld, O.; Ganz, A.B.; Dunn, J.; Hornburg, D.; et al. A longitudinal big data approach for precision health. Nat. Med. 2019, 25, 792–804.
- Babu, M.; Snyder, M. Multi-Omics Profiling for Health. Mol. Cell. Proteom. MCP 2023, 22, 100561.
- Marshall, J.L.; Peshkin, B.N.; Yoshino, T.; Vowinckel, J.; Danielsen, H.E.; Melino, G.; Tsamardinos, I.; Haudenschild, C.; Kerr, D.J.; Sampaio, C.; et al. The Essentials of Multiomics. Oncologist 2022, 27, 272–284.
- Muzzey, D.; Evans, E.A.; Lieber, C. Understanding the Basics of NGS: From Mechanism to Variant Calling. Curr. Genet. Med. Rep. 2015, 3, 158–165.
- Lancaster, S.M.; Sanghi, A.; Wu, S.; Snyder, M.P. A Customizable Analysis Flow in Integrative Multi-Omics. Biomolecules 2020, 10, 1606.
- Weinstein, J.N.; Collisson, E.A.; Mills, G.B.; Shaw, K.R.; Ozenberger, B.A.; Ellrott, K.; Shmulevich, I.; Sander, C.; Stuart, J.M. The Cancer Genome Atlas Pan-Cancer analysis project. Nat. Genet. 2013, 45, 1113–1120.
- Srimadh Bhagavatham, S.K.; Pulukool, S.K.; Pradhan, S.S.; Ashok Naik, A.; VM, D.D.; Sivaramakrishnan, V. Systems biology approach delineates critical pathways associated with disease progression in rheumatoid arthritis. J. Biomol. Struct. Dyn. 2022.
- Banchereau, R.; Hong, S.; Cantarel, B.; Baldwin, N.; Baisch, J.; Edens, M.; Cepika, A.M.; Acs, P.; Turner, J.; Anguiano, E.; et al. Personalized Immunomonitoring Uncovers Molecular Networks that Stratify Lupus Patients. Cell 2016, 165, 551–565.
- Logotheti, M.; Agioutantis, P.; Katsaounou, P.; Loutrari, H. Microbiome Research and Multi-Omics Integration for Personalized Medicine in Asthma. J. Pers. Med. 2021, 11, 1299.
- Li, C.X.; Wheelock, C.E.; Sköld, C.M.; Wheelock, Å.M. Integration of multi-omics datasets enables molecular classification of COPD. Eur. Respir. J. 2018, 51, 1701930.
- Mars, R.A.T.; Yang, Y.; Ward, T.; Houtti, M.; Priya, S.; Lekatz, H.R.; Tang, X.; Sun, Z.; Kalari, K.R.; Korem, T.; et al. Longitudinal Multi-omics Reveals Subset-Specific Mechanisms Underlying Irritable Bowel Syndrome. Cell 2020, 183, 1137–1140.
- Higdon, R.; Earl, R.K.; Stanberry, L.; Hudac, C.M.; Montague, E.; Stewart, E.; Janko, I.; Choiniere, J.; Broomall, W.; Kolker, N.; et al. The promise of multi-omics and clinical data integration to identify and target personalized healthcare approaches in autism spectrum disorders. Omics J. Integr. Biol. 2015, 19, 197–208.
- Marbach, D.; Lamparter, D.; Quon, G.; Kellis, M.; Kutalik, Z.; Bergmann, S. Tissue-specific regulatory circuits reveal variable modular perturbations across complex diseases. Nat. Methods 2016, 13, 366–370.
- Kussmann, M.; Blum, S. OMICS-derived targets for inflammatory gut disorders: Opportunities for the development of nutrition related biomarkers. Endocr. Metab. Immune Disord. Drug Targets 2007, 7, 271–287.
- Imhann, F.; Van der Velde, K.J.; Barbieri, R.; Alberts, R.; Voskuil, M.D.; Vich Vila, A.; Collij, V.; Spekhorst, L.M.; Van der Sloot, K.W.J.; Peters, V.; et al. The 1000IBD project: Multi-omics data of 1000 inflammatory bowel disease patients; data release 1. BMC Gastroenterol. 2019, 19, 5.
- Hu, S.; Uniken Venema, W.T.; Westra, H.J.; Vich Vila, A.; Barbieri, R.; Voskuil, M.D.; Blokzijl, T.; Jansen, B.H.; Li, Y.; Daly, M.J.; et al. Inflammation status modulates the effect of host genetic variation on intestinal gene expression in inflammatory bowel disease. Nat. Commun. 2021, 12, 1122.
- Bolte, L.A.; Vich Vila, A.; Imhann, F.; Collij, V.; Gacesa, R.; Peters, V.; Wijmenga, C.; Kurilshikov, A.; Campmans-Kuijpers, M.J.E.; Fu, J.; et al. Long-term dietary patterns are associated with pro-inflammatory and anti-inflammatory features of the gut microbiome. Gut 2021, 70, 1287–1298.
- Vich Vila, A.; Collij, V.; Sanna, S.; Sinha, T.; Imhann, F.; Bourgonje, A.R.; Mujagic, Z.; Jonkers, D.; Masclee, A.A.M.; Fu, J.; et al. Impact of commonly used drugs on the composition and metabolic function of the gut microbiota. Nat. Commun. 2020, 11, 362.
- van der Sloot, K.W.J.; Weersma, R.K.; Alizadeh, B.Z.; Dijkstra, G. Identification of Environmental Risk Factors Associated With the Development of Inflammatory Bowel Disease. J. Crohn’s Colitis 2020, 14, 1662–1671.
- Bourgonje, A.R.; Hu, S.; Spekhorst, L.M.; Zhernakova, D.V.; Vich Vila, A.; Li, Y.; Voskuil, M.D.; van Berkel, L.A.; Bley Folly, B.; Charrout, M.; et al. The Effect of Phenotype and Genotype on the Plasma Proteome in Patients with Inflammatory Bowel Disease. J. Crohn’s Colitis 2022, 16, 414–429.
- Sudhakar, P.; Alsoud, D.; Wellens, J.; Verstockt, S.; Arnauts, K.; Verstockt, B.; Vermeire, S. Tailoring Multi-omics to Inflammatory Bowel Diseases: All for One and One for All. J. Crohn’s Colitis 2022, 16, 1306–1320.
- Vetrano, S.; Bouma, G.; Benschop, R.J.; Birngruber, T.; Costanzo, A.; D’Haens, G.; Frasca, L.; Hillenbrand, R.; Iversen, L.; Johansen, C.; et al. ImmUniverse Consortium: Multi-omics integrative approach in personalized medicine for immune-mediated inflammatory diseases. Front. Immunol. 2022, 13, 1002629.
- Seyed Tabib, N.S.; Madgwick, M.; Sudhakar, P.; Verstockt, B.; Korcsmaros, T.; Vermeire, S. Big data in IBD: Big progress for clinical practice. Gut 2020, 69, 1520–1532.
- Weersma, R.K.; Xavier, R.J.; Vermeire, S.; Barrett, J.C. Multiomics Analyses to Deliver the Most Effective Treatment to Every Patient With Inflammatory Bowel Disease. Gastroenterology 2018, 155, e1–e4.
- Borg-Bartolo, S.P.; Boyapati, R.K.; Satsangi, J.; Kalla, R. Precision medicine in inflammatory bowel disease: Concept, progress and challenges. F1000Research 2020, 9.
- Liu, X.Y.; Tang, H.; Zhou, Q.Y.; Zeng, Y.L.; Chen, D.; Xu, H.; Li, Y.; Tan, B.; Qian, J.M. Advancing the precision management of inflammatory bowel disease in the era of omics approaches and new technology. World J. Gastroenterol. 2023, 29, 272–285.
- Agrawal, M.; Allin, K.H.; Petralia, F.; Colombel, J.F.; Jess, T. Multiomics to elucidate inflammatory bowel disease risk factors and pathways. Nat. Rev. Gastroenterol. Hepatol. 2022, 19, 399–409.
- Huang, H.; Vangay, P.; McKinlay, C.E.; Knights, D. Multi-omics analysis of inflammatory bowel disease. Immunol. Lett. 2014, 162, 62–68.
- Vermeulen, R.; Schymanski, E.L.; Barabasi, A.L.; Miller, G.W. The exposome and health: Where chemistry meets biology. Science 2020, 367, 392–396.
- Suzuki, T.; Hidaka, T.; Kumagai, Y.; Yamamoto, M. Environmental pollutants and the immune response. Nat. Immunol. 2020, 21, 1486–1495.
- Peters, A.; Nawrot, T.S.; Baccarelli, A.A. Hallmarks of environmental insults. Cell 2021, 184, 1455–1468.
- Ananthakrishnan, A.N.; Bernstein, C.N.; Iliopoulos, D.; Macpherson, A.; Neurath, M.F.; Ali, R.A.R.; Vavricka, S.R.; Fiocchi, C. Environmental triggers in IBD: A review of progress and evidence. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 39–49.
- Rothschild, D.; Weissbrod, O.; Barkan, E.; Kurilshikov, A.; Korem, T.; Zeevi, D.; Costea, P.I.; Godneva, A.; Kalka, I.N.; Bar, N.; et al. Environment dominates over host genetics in shaping human gut microbiota. Nature 2018, 555, 210–215.
- Sartor, R.B.; Wu, G.D. Roles for Intestinal Bacteria, Viruses, and Fungi in Pathogenesis of Inflammatory Bowel Diseases and Therapeutic Approaches. Gastroenterology 2017, 152, 327–339.e324.
- Franzosa, E.A.; Huang, K.; Meadow, J.F.; Gevers, D.; Lemon, K.P.; Bohannan, B.J.; Huttenhower, C. Identifying personal microbiomes using metagenomic codes. Proc. Natl. Acad. Sci. USA 2015, 112, E2930–E2938.
- Benech, N.; Sokol, H. Targeting the gut microbiota in inflammatory bowel diseases: Where are we? Curr. Opin. Microbiol. 2023, 74, 102319.
- Schirmer, M.; Smeekens, S.P.; Vlamakis, H.; Jaeger, M.; Oosting, M.; Franzosa, E.A.; Jansen, T.; Jacobs, L.; Bonder, M.J.; Kurilshikov, A.; et al. Linking the Human Gut Microbiome to Inflammatory Cytokine Production Capacity. Cell 2016, 167, 1125–1136.e1128.
- Lloyd-Price, J.; Arze, C.; Ananthakrishnan, A.N.; Schirmer, M.; Avila-Pacheco, J.; Poon, T.W.; Andrews, E.; Ajami, N.J.; Bonham, K.S.; Brislawn, C.J.; et al. Multi-omics of the gut microbial ecosystem in inflammatory bowel diseases. Nature 2019, 569, 655–662.
- Zhang, Y.; Bhosle, A.; Bae, S.; McIver, L.J.; Pishchany, G.; Accorsi, E.K.; Thompson, K.N.; Arze, C.; Wang, Y.; Subramanian, A.; et al. Discovery of bioactive microbial gene products in inflammatory bowel disease. Nature 2022, 606, 754–760.
- Chu, H.; Khosravi, A.; Kusumawardhani, I.P.; Kwon, A.H.; Vasconcelos, A.C.; Cunha, L.D.; Mayer, A.E.; Shen, Y.; Wu, W.L.; Kambal, A.; et al. Gene-microbiota interactions contribute to the pathogenesis of inflammatory bowel disease. Sciecne 2016, 352, 1116–1120.
- Hold, G.L. Western lifestyle: A ‘master’ manipulator of the intestinal microbiota? Gut 2014, 63, 5–6.
- Zmora, N.; Suez, J.; Elinav, E. You are what you eat: Diet, health and the gut microbiota. Nat. Rev. Gastroenterol. Hepatol. 2019, 16, 35–56.
- Hooper, L.V.; Littman, D.R.; Macpherson, A.J. Interactions between the microbiota and the immune system. Science 2012, 336, 1268–1273.
- Maier, L.; Pruteanu, M.; Kuhn, M.; Zeller, G.; Telzerow, A.; Anderson, E.E.; Brochado, A.R.; Fernandez, K.C.; Dose, H.; Mori, H.; et al. Extensive impact of non-antibiotic drugs on human gut bacteria. Nature 2018, 555, 623–628.
- de Souza, H.S.; Fiocchi, C. Immunopathogenesis of IBD: Current state of the art. Nat. Rev. Gastroenterol. Hepatol. 2016, 13, 13–27.
- Schneider, K.M.; Blank, N.; Alvarez, Y.; Thum, K.; Lundgren, P.; Litichevskiy, L.; Sleeman, M.; Bahnsen, K.; Kim, J.; Kardo, S.; et al. The enteric nervous system relays psychological stress to intestinal inflammation. Cell 2023, 186, 2823–2838.e2820.
- Ruiz-Nunez, B.; Pruimboom, L.; Dijck-Brouwer, D.A.; Muskiet, F.A. Lifestyle and nutritional imbalances associated with Western diseases: Causes and consequences of chronic systemic low-grade inflammation in an evolutionary context. J. Nutr. Biochem. 2013, 24, 1183–1201.
- Bekkering, S.; Domínguez-Andrés, J.; Joosten, L.A.B.; Riksen, N.P.; Netea, M.G. Trained Immunity: Reprogramming Innate Immunity in Health and Disease. Annu. Rev. Immunol. 2021, 39, 667–693.
- Lee, J.C.; Lyons, P.A.; McKinney, E.F.; Sowerby, J.M.; Carr, E.J.; Bredin, F.; Rickman, H.M.; Ratlamwala, H.; Hatton, A.; Rayner, T.F.; et al. Gene expression profiling of CD8+ T cells predicts prognosis in patients with Crohn disease and ulcerative colitis. J. Clin. Investig. 2011, 121, 4170–4179.
- Gasparetto, M.; Payne, F.; Nayak, K.; Kraiczy, J.; Glemas, C.; Philip-McKenzie, Y.; Ross, A.; Edgar, R.D.; Zerbino, D.R.; Salvestrini, C.; et al. Transcription and DNA Methylation Patterns of Blood-Derived CD8(+) T Cells Are Associated With Age and Inflammatory Bowel Disease But Do Not Predict Prognosis. Gastroenterology 2021, 160, 232–244.e237.
- Tom, M.R.; Li, J.; Ueno, A.; Fort Gasia, M.; Chan, R.; Hung, D.Y.; Chenoo, S.; Iacucci, M.; Jijon, H.B.; Kaplan, G.G.; et al. Novel CD8+ T-Cell Subsets Demonstrating Plasticity in Patients with Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2016, 22, 1596–1608.
- Christo, S.N.; Evrard, M.; Park, S.L.; Gandolfo, L.C.; Burn, T.N.; Fonseca, R.; Newman, D.M.; Alexandre, Y.O.; Collins, N.; Zamudio, N.M.; et al. Discrete tissue microenvironments instruct diversity in resident memory T cell function and plasticity. Nat. Immunol. 2021, 22, 1140–1151.
- Margraf, A.; Perretti, M. Immune Cell Plasticity in Inflammation: Insights into Description and Regulation of Immune Cell Phenotypes. Cells 2022, 11, 1824.
- de Souza, H.S.P.; Fiocchi, C.; Iliopoulos, D. The IBD interactome: An integrated view of aetiology, pathogenesis and therapy. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 739–749.
- Deans, C.; Maggert, K.A. What do you mean, “epigenetic”? Genetics 2015, 199, 887–896.
- Ventham, N.T.; Kennedy, N.A.; Nimmo, E.R.; Satsangi, J. Beyond gene discovery in inflammatory bowel disease: The emerging role of epigenetics. Gastroenterology 2013, 145, 293–308.
- Cavalli, G.; Heard, E. Advances in epigenetics link genetics to the environment and disease. Nature 2019, 571, 489–499.
- Howell, K.J.; Kraiczy, J.; Nayak, K.M.; Gasparetto, M.; Ross, A.; Lee, C.; Mak, T.N.; Koo, B.K.; Kumar, N.; Lawley, T.; et al. DNA Methylation and Transcription Patterns in Intestinal Epithelial Cells From Pediatric Patients With Inflammatory Bowel Diseases Differentiate Disease Subtypes and Associate With Outcome. Gastroenterology 2018, 154, 585–598.
- Kalla, R.; Adams, A.T.; Nowak, J.K.; Bergemalm, D.; Vatn, S.; Ventham, N.T.; Kennedy, N.A.; Ricanek, P.; Lindstrom, J.; Söderholm, J.; et al. Analysis of Systemic Epigenetic Alterations in Inflammatory Bowel Disease: Defining Geographical, Genetic and Immune-Inflammatory influences on the Circulating Methylome. J. Crohn’s Colitis 2023, 17, 170–184.
- Ventham, N.T.; Kennedy, N.A.; Kalla, R.; Adams, A.T.; Noble, A.; Ennis, H.; Mowat, C.; Dunlop, M.G.; Satsangi, J. Genome-Wide Methylation Profiling in 229 Patients With Crohn’s Disease Requiring Intestinal Resection: Epigenetic Analysis of the Trial of Prevention of Post-operative Crohn’s Disease (TOPPIC). Cell. Mol. Gastroenterol. Hepatol. 2023, 16, 431–450.
- Noble, A.J.; Nowak, J.K.; Adams, A.T.; Uhlig, H.H.; Satsangi, J. Defining Interactions Between the Genome, Epigenome, and the Environment in Inflammatory Bowel Disease: Progress and Prospects. Gastroenterology 2023, 165, 44–60.e42.
- Meuwis, M.A.; Fillet, M.; Geurts, P.; de Seny, D.; Lutteri, L.; Chapelle, J.P.; Bours, V.; Wehenkel, L.; Belaiche, J.; Malaise, M.; et al. Biomarker discovery for inflammatory bowel disease, using proteomic serum profiling. Biochem. Pharmacol. 2007, 73, 1422–1433.
- Titz, B.; Gadaleta, R.M.; Lo Sasso, G.; Elamin, A.; Ekroos, K.; Ivanov, N.V.; Peitsch, M.C.; Hoeng, J. Proteomics and Lipidomics in Inflammatory Bowel Disease Research: From Mechanistic Insights to Biomarker Identification. Int. J. Mol. Sci. 2018, 19, 2775.
- Baldan-Martin, M.; Chaparro, M.; Gisbert, J.P. Tissue Proteomic Approaches to Understand the Pathogenesis of Inflammatory Bowel Disease. Inflamm. Bowel Dis. 2021, 27, 1184–1200.
- Scoville, E.A.; Allaman, M.M.; Brown, C.T.; Motley, A.K.; Horst, S.N.; Williams, C.S.; Koyama, T.; Zhao, Z.; Adams, D.W.; Beaulieu, D.B.; et al. Alterations in Lipid, Amino Acid, and Energy Metabolism Distinguish Crohn’s Disease from Ulcerative Colitis and Control Subjects by Serum Metabolomic Profiling. Metabolomics Off. J. Metabolomic Soc. 2018, 14, 17.
- Fan, F.; Mundra, P.A.; Fang, L.; Galvin, A.; Moore, X.L.; Weir, J.M.; Wong, G.; White, D.A.; Chin-Dusting, J.; Sparrow, M.P.; et al. Lipidomic Profiling in Inflammatory Bowel Disease: Comparison Between Ulcerative Colitis and Crohn’s Disease. Inflamm. Bowel Dis. 2015, 21, 1511–1518.
- Gonzalez, C.G.; Mills, R.H.; Zhu, Q.; Sauceda, C.; Knight, R.; Dulai, P.S.; Gonzalez, D.J. Location-specific signatures of Crohn’s disease at a multi-omics scale. Microbiome 2022, 10, 133.
- Macaulay, I.C.; Ponting, C.P.; Voet, T. Single-Cell Multiomics: Multiple Measurements from Single Cells. Trends Genet. TIG 2017, 33, 155–168.
- Levsky, J.M.; Shenoy, S.M.; Pezo, R.C.; Singer, R.H. Single-cell gene expression profiling. Science 2002, 297, 836–840.
- Tang, F.; Barbacioru, C.; Wang, Y.; Nordman, E.; Lee, C.; Xu, N.; Wang, X.; Bodeau, J.; Tuch, B.B.; Siddiqui, A.; et al. mRNA-Seq whole-transcriptome analysis of a single cell. Nat. Methods 2009, 6, 377–382.
- Björklund, Å.K.; Forkel, M.; Picelli, S.; Konya, V.; Theorell, J.; Friberg, D.; Sandberg, R.; Mjösberg, J. The heterogeneity of human CD127(+) innate lymphoid cells revealed by single-cell RNA sequencing. Nat. Immunol. 2016, 17, 451–460.
- Villani, A.C.; Satija, R.; Reynolds, G.; Sarkizova, S.; Shekhar, K.; Fletcher, J.; Griesbeck, M.; Butler, A.; Zheng, S.; Lazo, S.; et al. Single-cell RNA-seq reveals new types of human blood dendritic cells, monocytes, and progenitors. Science 2017, 356.
- Saviano, A.; Henderson, N.C.; Baumert, T.F. Single-cell genomics and spatial transcriptomics: Discovery of novel cell states and cellular interactions in liver physiology and disease biology. J. Hepatol. 2020, 73, 1219–1230.
- Poulin, J.F.; Tasic, B.; Hjerling-Leffler, J.; Trimarchi, J.M.; Awatramani, R. Disentangling neural cell diversity using single-cell transcriptomics. Nat. Neurosci. 2016, 19, 1131–1141.
- Grün, D.; Lyubimova, A.; Kester, L.; Wiebrands, K.; Basak, O.; Sasaki, N.; Clevers, H.; van Oudenaarden, A. Single-cell messenger RNA sequencing reveals rare intestinal cell types. Nature 2015, 525, 251–255.
- Haber, A.L.; Biton, M.; Rogel, N.; Herbst, R.H.; Shekhar, K.; Smillie, C.; Burgin, G.; Delorey, T.M.; Howitt, M.R.; Katz, Y.; et al. A single-cell survey of the small intestinal epithelium. Nature 2017, 551, 333–339.
- Islam, M.; Chen, B.; Spraggins, J.M.; Kelly, R.T.; Lau, K.S. Use of Single-Cell -Omic Technologies to Study the Gastrointestinal Tract and Diseases, From Single Cell Identities to Patient Features. Gastroenterology 2020, 159, 453–466.e451.
- Vandereyken, K.; Sifrim, A.; Thienpont, B.; Voet, T. Methods and applications for single-cell and spatial multi-omics. Nat. Rev. Genet. 2023, 24, 494–515.
- Carlberg, K.; Korotkova, M.; Larsson, L.; Catrina, A.I.; Ståhl, P.L.; Malmström, V. Exploring inflammatory signatures in arthritic joint biopsies with Spatial Transcriptomics. Sci. Rep. 2019, 9, 18975.
- Vento-Tormo, R.; Vilarrasa-Blasi, R. Cell-level reference maps for the human body take shape. Nature 2023, 619, 467–468.
- Martin, J.C.; Chang, C.; Boschetti, G.; Ungaro, R.; Giri, M.; Grout, J.A.; Gettler, K.; Chuang, L.S.; Nayar, S.; Greenstein, A.J.; et al. Single-Cell Analysis of Crohn’s Disease Lesions Identifies a Pathogenic Cellular Module Associated with Resistance to Anti-TNF Therapy. Cell 2019, 178, 1493–1508.e1420.
- Corridoni, D.; Antanaviciute, A.; Gupta, T.; Fawkner-Corbett, D.; Aulicino, A.; Jagielowicz, M.; Parikh, K.; Repapi, E.; Taylor, S.; Ishikawa, D.; et al. Single-cell atlas of colonic CD8(+) T cells in ulcerative colitis. Nat. Med. 2020, 26, 1480–1490.
- Parikh, K.; Antanaviciute, A.; Fawkner-Corbett, D.; Jagielowicz, M.; Aulicino, A.; Lagerholm, C.; Davis, S.; Kinchen, J.; Chen, H.H.; Alham, N.K.; et al. Colonic epithelial cell diversity in health and inflammatory bowel disease. Nature 2019, 567, 49–55.
- Mukherjee, P.K.; Nguyen, Q.T.; Li, J.; Zhao, S.; Christensen, S.M.; West, G.A.; Chandra, J.; Gordon, I.O.; Lin, S.; Wang, J.; et al. Stricturing Crohn’s disease single-cell RNA sequencing reveals fibroblast heterogeneity and intercellular interactions. Gastroenterology 2023. Online ahead of print.
- Mennillo, E.; Kim, Y.J.; Rusu, I.; Lee, G.; Dorman, L.C.; Bernard-Vazquez, F.; Bain, J.L.; Patel, R.; Andersen, C.; Rao, A.; et al. Single-cell and spatial multi-omics identify innate and stromal modules targeted by anti-integrin therapy in ulcerative colitis. Biorxiv Prepr. Serv. Biol. 2023. Online ahead of print.
- Sands, B.E. Biomarkers of Inflammation in Inflammatory Bowel Disease. Gastroenterology 2015, 149, 1275–1285.e1272.
- Prideaux, L.; De Cruz, P.; Ng, S.C.; Kamm, M.A. Serological antibodies in inflammatory bowel disease: A systematic review. Inflamm. Bowel Dis. 2012, 18, 1340–1355.
- FDA-NIH Biomarker Working Group. BEST (Biomarkers, Endpoints, and Other Tools) Resource ; Food and Drug Administration: Silver Spring, MD, USA, 2016.
- Sheng Ding, N.; De Cruz, P. (Eds.) A Systems Biology Approach to Biomarkers in Inflammatory Bowel Disease. In Biomarkers in Inflammatory Bowel Diseases; Springer: Berlin/Heidelberg, Germany, 2019.
- Quezada, H.; Guzman-Ortiz, A.L.; Diaz-Sanchez, H.; Valle-Rios, R.; Aguirre-Hernandez, J. Omics-based biomarkers: Current status and potential use in the clinic. Bol. Med. Hosp. Infant. Mex. 2017, 74, 219–226.
- Sethi, S.; Brietzke, E. Omics-Based Biomarkers: Application of Metabolomics in Neuropsychiatric Disorders. Int. J. Neuropsychopharmacol. 2015, 19, pyv096.
- Sevimoglu, T.; Arga, K.Y. Computational Systems Biology of Psoriasis: Are We Ready for the Age of Omics and Systems Biomarkers? Omics J. Integr. Biol. 2015, 19, 669–687.
- Robles, A.I.; Harris, C.C. Integration of multiple "OMIC" biomarkers: A precision medicine strategy for lung cancer. Lung Cancer 2017, 107, 50–58.
- Wu, T.; Cooper, S.A.; Shah, V.H. Omics and AI advance biomarker discovery for liver disease. Nat. Med. 2022, 28, 1131–1132.
- Fiocchi, C. A Systems Biology Approach to Biomarkers in Inflammatory Bowel Disease. In Biomarkers in Inflammatory Bowel Diseases; Sheng Ding, N., D’e Cruz, P.A.M., Eds.; Springer: Berlin/Heidelberg, Germany, 2019.
- Borren, N.Z.; Plichta, D.; Joshi, A.D.; Bonilla, G.; Sadreyev, R.; Vlamakis, H.; Xavier, R.J.; Ananthakrishnan, A.N. Multi-“-Omics” Profiling in Patients With Quiescent Inflammatory Bowel Disease Identifies Biomarkers Predicting Relapse. Inflamm. Bowel Dis. 2020, 26, 1524–1532.
- Janker, L.; Schuster, D.; Bortel, P.; Hagn, G.; Meier-Menches, S.M.; Mohr, T.; Mader, J.C.; Slany, A.; Bileck, A.; Brunmair, J.; et al. Multi-omics empowered deep phenotyping of ulcerative colitis identifies biomarker signatures reporting functional remission states. J. Crohn’s Colitis 2023, jjad052.
- Pierre, N.; Huynh-Thu, V.A.; Marichal, T.; Allez, M.; Bouhnik, Y.; Laharie, D.; Bourreille, A.; Colombel, J.F.; Meuwis, M.A.; Louis, E. Distinct blood protein profiles associated with the risk of short-term and mid/long-term clinical relapse in patients with Crohn’s disease stopping infliximab: When the remission state hides different types of residual disease activity. Gut 2023, 72, 443–450.
- Meuwis, M.A.; Fillet, M.; Lutteri, L.; Maree, R.; Geurts, P.; de Seny, D.; Malaise, M.; Chapelle, J.P.; Wehenkel, L.; Belaiche, J.; et al. Proteomics for prediction and characterization of response to infliximab in Crohn’s disease: A pilot study. Clin. Biochem. 2008, 41, 960–967.
- Lee, J.W.J.; Plichta, D.; Hogstrom, L.; Borren, N.Z.; Lau, H.; Gregory, S.M.; Tan, W.; Khalili, H.; Clish, C.; Vlamakis, H.; et al. Multi-omics reveal microbial determinants impacting responses to biologic therapies in inflammatory bowel disease. Cell Host Microbe 2021, 29, 1294–1304.e1294.
- Mishra, N.; Aden, K.; Blase, J.I.; Baran, N.; Bordoni, D.; Tran, F.; Conrad, C.; Avalos, D.; Jaeckel, C.; Scherer, M.; et al. Longitudinal multi-omics analysis identifies early blood-based predictors of anti-TNF therapy response in inflammatory bowel disease. Genome Med. 2022, 14, 110.
- Magro, F.; Rodrigues-Pinto, E.; Santos-Antunes, J.; Vilas-Boas, F.; Lopes, S.; Nunes, A.; Camila-Dias, C.; Macedo, G. High C-reactive protein in Crohn’s disease patients predicts nonresponse to infliximab treatment. J. Crohn’s Colitis 2014, 8, 129–136.
- Johansson, Å.; Andreassen, O.A.; Brunak, S.; Franks, P.W.; Hedman, H.; Loos, R.J.F.; Meder, B.; Melén, E.; Wheelock, C.E.; Jacobsson, B. Precision medicine in complex diseases-Molecular subgrouping for improved prediction and treatment stratification. J. Intern. Med. 2023, 294, 378–396.
- Minervini, A.; Mari, A. Multimodal prognostic models and recent therapeutic advances. Lancet. Digit. Health 2023.
- Denson, L.A.; Curran, M.; McGovern, D.P.B.; Koltun, W.A.; Duerr, R.H.; Kim, S.C.; Sartor, R.B.; Sylvester, F.A.; Abraham, C.; de Zoeten, E.F.; et al. Challenges in IBD Research: Precision Medicine. Inflamm. Bowel Dis. 2019, 25, S31–S39.
- Thomas, J.P.; Modos, D.; Korcsmaros, T.; Brooks-Warburton, J. Network Biology Approaches to Achieve Precision Medicine in Inflammatory Bowel Disease. Front. Genet. 2021, 12, 760501.
- Gardiner, L.J.; Carrieri, A.P.; Bingham, K.; Macluskie, G.; Bunton, D.; McNeil, M.; Pyzer-Knapp, E.O. Combining explainable machine learning, demographic and multi-omic data to inform precision medicine strategies for inflammatory bowel disease. PLoS ONE 2022, 17, e0263248.
- Torres, J.; Halfvarson, J.; Rodríguez-Lago, I.; Hedin, C.R.H.; Jess, T.; Dubinsky, M.; Croitoru, K.; Colombel, J.F. Results of the Seventh Scientific Workshop of ECCO: Precision Medicine in IBD-Prediction and Prevention of Inflammatory Bowel Disease. J. Crohn’s Colitis 2021, 15, 1443–1454.
- Verstockt, B.; Noor, N.M.; Marigorta, U.M.; Pavlidis, P.; Deepak, P.; Ungaro, R.C. Results of the Seventh Scientific Workshop of ECCO: Precision Medicine in IBD-Disease Outcome and Response to Therapy. J. Crohn’s Colitis 2021, 15, 1431–1442.
- Dart, R.J.; Ellul, P.; Scharl, M.; Lamb, C.A. Results of the Seventh Scientific Workshop of ECCO: Precision Medicine in IBD—Challenges and Future Directions. J. Crohn’s Colitis 2021, 15, 1407–1409.
