Anxiety and depression have become widespread mental disorders identified by cognition, mood, and attitude variations that significantly impact an individual’s well-being and daily life. Depression disorders have been estimated at approximately 17%, while the prevalence of anxiety disorders is about 29%. Considerable evidence confirms that mental health disorders enhance appetite and cravings and decrease motivation for physical activity. Furthermore, high sugar intake has been associated with depression and anxiety in numerous cross-sectional and observational studies. Along the same lines, research studies have identified a link between the intake of refined carbohydrates and circulating inflammatory markers and their impact on mental health.
- diabetes
- mental health
- anxiety
- depression
- supplementation
- nutrition
1. The Effects of Diabetes on Anxiety Risk
2. The Effects of Anxiety on Diabetes Risk
| Author | Study Design | Population | Results |
|---|---|---|---|
| Rajput et al., 2016 [25][31] |
Cross-sectional, case–control study design. | Diabetes, n = 410 Healthy control, n = 410 |
There were twice as many cases of depression and anxiety in those with T2DM compared with healthy controls (26.3% vs. 11.2%). |
| Tovilla-Zarete et al., 2012 [73][32] |
Cross-sectional, multi-center study | Diabetes, n = 820 | 48.27% were positive for depression while 55.10% showed symptoms of anxiety. Occupation and complications were associated with anxiety while glucose level and complications were correlated with depression. |
| Collins et al., 2009 [74][33] |
Cross-sectional study | Diabetes, n = 1456 | Patients with diabetes had significant levels of anxiety (32.0%) and depressive symptoms (22.4%). Poor glycaemic control and female gender were risk factors for higher anxiety scores. Older age and a higher socioeconomic status demonstrated a protective effect, resulting in lower scores of anxiety and depression. |
| Shaban et al., 2006 [75][34] |
Cohort | Diabetes, n = 273 | Compared to men, women reported considerably greater mean anxiety levels. HbA1c was positively associated with anxiety and depression. |
| Campayo A. et al., 2010 [40][35] |
longitudinal design | Subjects with depression, n = 379 | Severe, moderate, and untreated depression are all linked to an increased risk of developing type 2 diabetes. Although persistent depression had a greater risk than the rest. |
| Golden S.H. et al., 2008 [44][36] |
Longitudinal cohort study | Analysis 1. participants without type 2 diabetes at baseline with and without depressive symptoms, n = 5201 Analysis 2. participants without depression at baseline with and without type 2 diabetes, n = 4847 |
The incidence of diabetes was correlated with baseline depressed symptoms. Impaired fasting glucose and untreated type 2 diabetes were negatively correlated with incident depressive symptoms, while treated type 2 diabetes exhibited a positive association. |
| Iversen et al., 2015 [76][37] |
Cohort | Depression, n = 36,031 | Depression was positively associated with diabetes. |
| Chien I. C & Lin C. H, 2016 [65][23] |
Prospective cohort | subjects had primary and secondary diagnoses of anxiety disorder, n = 766,427 | The prevalence of diabetes among individuals with anxiety disorders was greater than that of the general population. |
| Smith et al., 2018 [77][38] |
Meta-analysis | anxiety, 14 studies (n= 1,760,800) | Substantial positive correlation was shown between baseline anxiety and the incidence of diabetes |
| Khambaty T., 2017 [37][22] |
Cohort | anxiety, n = 2156 | Out of 2156 patients, 558 developed diabetes over a 10-year period. |
| Engum A., 2007 [69][27] |
Prospective population-based study | depression and anxiety, n = 8311 | Individuals with reported baseline symptoms of depression and anxiety were more likely to develop diabetes ten years later. |
| Meurs et al., 2016 [24][39] |
Cohort study | Depression n = 3002 Anxiety n = 9018 Diabetes n = 1781 Undiagnosed diabetes n = 786 |
Diabetes was independently linked to depression in both identified and undiagnosed cases. Diabetes diagnosis was independently linked to anxiety but this association was not observed for undiagnosed cases. |
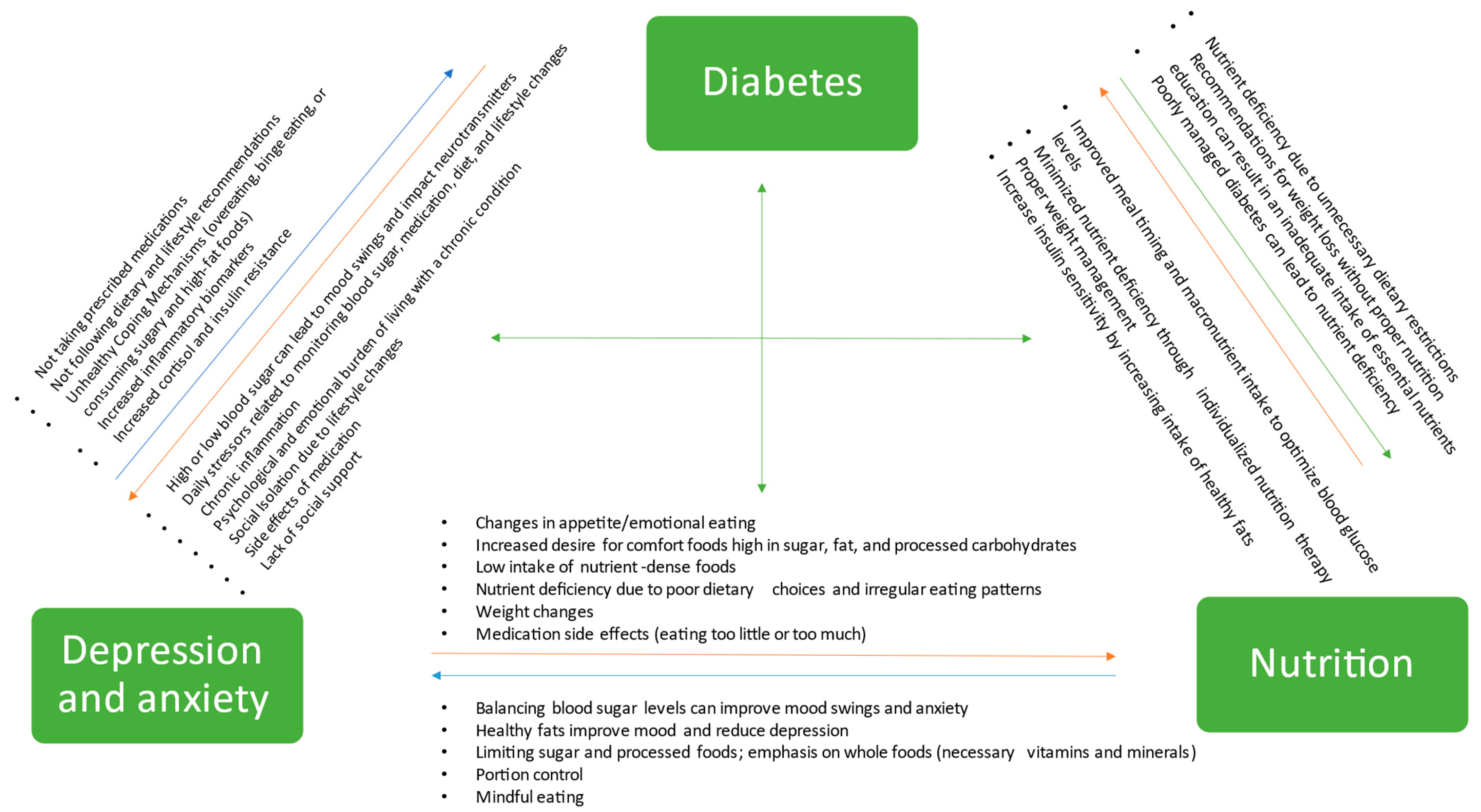
3. Exploring the Role of Nutrition in Preventing and Managing Diabetes, Depression, and Anxiety
References
- Polonsky, W.; Henry, R. Poor Medication Adherence in Type 2 Diabetes: Recognizing the Scope of the Problem and Its Key Contributors. PPA 2016, 10, 1299–1307.
- Rubin, R.R.; Peyrot, M. Psychological Issues and Treatments for People with Diabetes. J. Clin. Psychol. 2001, 57, 457–478.
- Force, I.C.G.T. Global Guideline for Type 2 Diabetes: Recommendations for Standard, Comprehensive, and Minimal Care. Diabet. Med. 2006, 23, 579–593.
- Kaur, G.; Tee, G.H.; Ariaratnam, S.; Krishnapillai, A.S.; China, K. Depression, Anxiety and Stress Symptoms among Diabetics in Malaysia: A Cross Sectional Study in an Urban Primary Care Setting. BMC Fam. Pract. 2013, 14, 69.
- Beckerle, C.M.; Lavin, M.A. Association of Self-Efficacy and Self-Care with Glycemic Control in Diabetes. Diabetes Spectr. 2013, 26, 172–178.
- McSharry, J.; Byrne, M.; Casey, B.; Dinneen, S.F.; Fredrix, M.; Hynes, L.; Lake, A.J.; Morrissey, E. Behaviour Change in Diabetes: Behavioural Science Advancements to Support the Use of Theory. Diabet. Med. 2020, 37, 455–463.
- The ACE/ADA Task Force on Inpatient Diabetes. American College of Endocrinology and American Diabetes Association Consensus Statement on Inpatient Diabetes and Glycemic Control. Diabetes Care 2006, 29, 1955–1962.
- Oğuz, N. Anxiety and Depression in Diabetic Patients. EJMI 2018, 2, 174–177.
- Tuligenga, R.H.; Dugravot, A.; Tabák, A.G.; Elbaz, A.; Brunner, E.J.; Kivimäki, M.; Singh-Manoux, A. Midlife Type 2 Diabetes and Poor Glycaemic Control as Risk Factors for Cognitive Decline in Early Old Age: A Post-Hoc Analysis of the Whitehall II Cohort Study. Lancet Diabetes Endocrinol. 2014, 2, 228–235.
- Pouwer, F. Should We Screen for Emotional Distress in Type 2 Diabetes Mellitus? Nat. Rev. Endocrinol. 2009, 5, 665–671.
- Khuwaja, A.K.; Lalani, S.; Dhanani, R.; Azam, I.S.; Rafique, G.; White, F. Anxiety and Depression among Outpatients with Type 2 Diabetes: A Multi-Centre Study of Prevalence and Associated Factors. Diabetol. Metab. Syndr. 2010, 2, 72.
- Huang, C.-J.; Wang, S.-Y.; Lee, M.-H.; Chiu, H.-C. Prevalence and Incidence of Mental Illness in Diabetes: A National Population-Based Cohort Study. Diabetes Res. Clin. Pract. 2011, 93, 106–114.
- Hasan, S.S.; Clavarino, A.M.; Dingle, K.; Mamun, A.A.; Kairuz, T. Diabetes Mellitus and the Risk of Depressive and Anxiety Disorders in Australian Women: A Longitudinal Study. J. Womens Health 2015, 24, 889–898.
- Svenningsson, I.; Björkelund, C.; Marklund, B.; Gedda, B. Anxiety and Depression in Obese and Normal-Weight Individuals with Diabetes Type 2: A Gender Perspective. Scand. J. Caring Sci. 2012, 26, 349–354.
- AlBekairy, A.; AbuRuz, S.; Alsabani, B.; Alshehri, A.; Aldebasi, T.; Alkatheri, A.; Almodaimegh, H. Exploring Factors Associated with Depression and Anxiety among Hospitalized Patients with Type 2 Diabetes Mellitus. MPP 2017, 26, 547–553.
- Al-Hayek, A.A.; Robert, A.A.; Alzaid, A.A.; Nusair, H.M.; Zbaidi, N.S.; Al-Eithan, M.H.; Sam, A.E. Association between Diabetes Self-Care, Medication Adherence, Anxiety, Depression, and Glycemic Control in Type 2 Diabetes. Saudi Med. J. 2012, 33, 681–683.
- Roy, T.; Lloyd, C.E. Epidemiology of Depression and Diabetes: A Systematic Review. J. Affect. Disord. 2012, 142, S8–S21.
- Khowaja, L.A.; Khuwaja, A.K.; Cosgrove, P. Cost of Diabetes Care in Out-Patient Clinics of Karachi, Pakistan. BMC Health Serv. Res. 2007, 7, 189.
- Lin, E.H.B.; Rutter, C.M.; Katon, W.; Heckbert, S.R.; Ciechanowski, P.; Oliver, M.M.; Ludman, E.J.; Young, B.A.; Williams, L.H.; McCulloch, D.K.; et al. Depression and Advanced Complications of Diabetes. Diabetes Care 2010, 33, 264–269.
- Smith, K.J.; Béland, M.; Clyde, M.; Gariépy, G.; Pagé, V.; Badawi, G.; Rabasa-Lhoret, R.; Schmitz, N. Association of Diabetes with Anxiety: A Systematic Review and Meta-Analysis. J. Psychosom. Res. 2013, 74, 89–99.
- Wiltink, J.; Beutel, M.E.; Till, Y.; Ojeda, F.M.; Wild, P.S.; Münzel, T.; Blankenberg, S.; Michal, M. Prevalence of Distress, Comorbid Conditions and Well Being in the General Population. J. Affect. Disord. 2011, 130, 429–437.
- Khambaty, T.; Callahan, C.M.; Perkins, A.J.; Stewart, J.C. Depression and Anxiety Screens as Simultaneous Predictors of 10-Year Incidence of Diabetes Mellitus in Older Adults in Primary Care. J. Am. Geriatr. Soc. 2017, 65, 294–300.
- Chien, I.-C.; Lin, C.-H. Increased Risk of Diabetes in Patients with Anxiety Disorders: A Population-Based Study. J. Psychosom. Res. 2016, 86, 47–52.
- Kautzky-Willer, A.; Harreiter, J.; Pacini, G. Sex and Gender Differences in Risk, Pathophysiology and Complications of Type 2 Diabetes Mellitus. Endocr. Rev. 2016, 37, 278–316.
- Demmer, R.T.; Gelb, S.; Suglia, S.F.; Keyes, K.M.; Aiello, A.E.; Colombo, P.C.; Galea, S.; Uddin, M.; Koenen, K.C.; Kubzansky, L.D. Sex Differences in the Association between Depression, Anxiety, and Type 2 Diabetes Mellitus. Psychosom. Med. 2015, 77, 467–477.
- Altemus, M.; Sarvaiya, N.; Neill Epperson, C. Sex Differences in Anxiety and Depression Clinical Perspectives. Front. Neuroendocrinol. 2014, 35, 320–330.
- Engum, A. The Role of Depression and Anxiety in Onset of Diabetes in a Large Population-Based Study. J. Psychosom. Res. 2007, 62, 31–38.
- Randler, C.; Desch, I.H.; Otte im Kampe, V.; Wüst-Ackermann, P.; Wilde, M.; Prokop, P. Anxiety, Disgust and Negative Emotions Influence Food Intake in Humans. Int. J. Gastron. Food Sci. 2017, 7, 11–15.
- Verma, S.; Hussain, M.E. Obesity and Diabetes: An Update. Diabetes Metab. Syndr. Clin. Res. Rev. 2017, 11, 73–79.
- Pandit, A.U.; Bailey, S.C.; Curtis, L.M.; Seligman, H.K.; Davis, T.C.; Parker, R.M.; Schillinger, D.; DeWalt, D.; Fleming, D.; Mohr, D.C.; et al. Disease-Related Distress, Self-Care and Clinical Outcomes among Low-Income Patients with Diabetes. J. Epidemiol. Community Health 2014, 68, 557–564.
- Rajput, R.; Gehlawat, P.; Gehlan, D.; Gupta, R.; Rajput, M. Prevalence and Predictors of Depression and Anxiety in Patients of Diabetes Mellitus in a Tertiary Care Center. Indian J. Endocrinol. Metab. 2016, 20, 746.
- Tovilla-Zárate, C.; Juárez-Rojop, I.; Jimenez, Y.P.; Jiménez, M.A.; Vázquez, S.; Bermúdez-Ocaña, D.; Ramón-Frías, T.; Mendoza, A.D.G.; García, S.P.; Narváez, L.L. Prevalence of Anxiety and Depression among Outpatients with Type 2 Diabetes in the Mexican Population. PLoS ONE 2012, 7, e36887.
- Collins, M.M.; Corcoran, P.; Perry, I.J. Anxiety and Depression Symptoms in Patients with Diabetes. Diabet. Med. 2009, 26, 153–161.
- Shaban, M.C.; Fosbury, J.; Kerr, D.; Cavan, D.A. The Prevalence of Depression and Anxiety in Adults with Type 1 Diabetes. Diabet. Med. 2006, 23, 1381–1384.
- Campayo, A.; de Jonge, P.; Roy, J.F.; Saz, P.; de la Cámara, C.; Quintanilla, M.A.; Marcos, G.; Santabárbara, J.; Lobo, A. Depressive Disorder and Incident Diabetes Mellitus: The Effect of Characteristics of Depression. AJP 2010, 167, 580–588.
- Golden, S.H.; Lazo, M.; Carnethon, M.; Bertoni, A.G.; Schreiner, P.J.; Roux, A.V.D.; Lee, H.B.; Lyketsos, C. Examining a Bidirectional Association Between Depressive Symptoms and Diabetes. JAMA 2008, 299, 2751–2759.
- Iversen, M.M.; Tell, G.S.; Espehaug, B.; Midthjell, K.; Graue, M.; Rokne, B.; Berge, L.I.; Østbye, T. Is Depression a Risk Factor for Diabetic Foot Ulcers? 11-Years Follow-up of the Nord-Trøndelag Health Study (HUNT). J. Diabetes Its Complicat. 2015, 29, 20–25.
- Smith, K.J.; Deschênes, S.S.; Schmitz, N. Investigating the Longitudinal Association between Diabetes and Anxiety: A Systematic Review and Meta-Analysis. Diabet. Med. 2018, 35, 677–693.
- Meurs, M.; Roest, A.M.; Wolffenbuttel, B.H.R.; Stolk, R.P.; de Jonge, P.; Rosmalen, J.G.M. Association of Depressive and Anxiety Disorders With Diagnosed Versus Undiagnosed Diabetes: An Epidemiological Study of 90,686 Participants. Psychosom. Med. 2016, 78, 233–241.
- Grajek, M.; Krupa-Kotara, K.; Białek-Dratwa, A.; Sobczyk, K.; Grot, M.; Kowalski, O.; Staśkiewicz, W. Nutrition and Mental Health: A Review of Current Knowledge about the Impact of Diet on Mental Health. Front. Nutr. 2022, 9, 943998.
- Solomou, S.; Logue, J.; Reilly, S.; Perez-Algorta, G. A Systematic Review of the Association of Diet Quality with the Mental Health of University Students: Implications in Health Education Practice. Health Educ. Res. 2023, 38, 28–68.
- O’Neil, A.; Quirk, S.E.; Housden, S.; Brennan, S.L.; Williams, L.J.; Pasco, J.A.; Berk, M.; Jacka, F.N. Relationship Between Diet and Mental Health in Children and Adolescents: A Systematic Review. Am. J. Public Health 2014, 104, e31–e42.
- Hu, F.B.; van Dam, R.M.; Liu, S. Diet and Risk of Type II Diabetes: The Role of Types of Fat and Carbohydrate. Diabetologia 2001, 44, 805–817.
- Tseng, T.-S.; Lin, W.-T.; Gonzalez, G.V.; Kao, Y.-H.; Chen, L.-S.; Lin, H.-Y. Sugar Intake from Sweetened Beverages and Diabetes: A Narrative Review. World J. Diabetes 2021, 12, 1530–1538.
- Basiri, R.; Spicer, M.; Levenson, C.; Ledermann, T.; Akhavan, N.; Arjmandi, B. Improving Dietary Intake of Essential Nutrients Can Ameliorate Inflammation in Patients with Diabetic Foot Ulcers. Nutrients 2022, 14, 2393.
- Basiri, R.; Spicer, M.T.; Levenson, C.W.; Ormsbee, M.J.; Ledermann, T.; Arjmandi, B.H. Nutritional Supplementation Concurrent with Nutrition Education Accelerates the Wound Healing Process in Patients with Diabetic Foot Ulcers. Biomedicines 2020, 8, 263. Available online: https://pubmed.ncbi.nlm.nih.gov/32756299/ (accessed on 1 November 2020).
- Akhavan, N.S.; Pourafshar, S.; Johnson, S.A.; Foley, E.M.; George, K.S.; Munoz, J.; Siebert, S.; Clark, E.A.; Basiri, R.; Hickner, R.C.; et al. The Relationship between Protein Intake and Source on Factors Associated with Glycemic Control in Individuals with Prediabetes and Type 2 Diabetes. Nutrients 2020, 12, 2031. Available online: https://pubmed.ncbi.nlm.nih.gov/32650580/ (accessed on 3 August 2020).
- Basiri, R.; Spicer, M.; Munoz, J.; Arjmandi, B. Nutritional Intervention Improves the Dietary Intake of Essential Micronutrients in Patients with Diabetic Foot Ulcers. Curr. Dev. Nutr. 2020, 4, 8.
- Nutrition Supplementation and Education May Increase the Healing Rate in Diabetic Patients with Foot Ulcers (P19-005-19)|Current Developments in Nutrition|Oxford Academic. Available online: https://academic.oup.com/cdn/article/3/Supplement_1/nzz049.P19-005-19/5518126 (accessed on 26 April 2023).
- Basiri, R.; Spicer, M.T.; Ledermann, T.; Arjmandi, B.H. Effects of Nutrition Intervention on Blood Glucose, Body Composition, and Phase Angle in Obese and Overweight Patients with Diabetic Foot Ulcers. Nutrients 2022, 14, 3564.
- Martín-Peláez, S.; Fito, M.; Castaner, O. Mediterranean Diet Effects on Type 2 Diabetes Prevention, Disease Progression, and Related Mechanisms. A Review. Nutrients 2020, 12, 2236.
- Sluik, D.; Brouwer-Brolsma, E.M.; Berendsen, A.A.M.; Mikkilä, V.; Poppitt, S.D.; Silvestre, M.P.; Tremblay, A.; Pérusse, L.; Bouchard, C.; Raben, A.; et al. Protein Intake and the Incidence of Pre-Diabetes and Diabetes in 4 Population-Based Studies: The PREVIEW Project. Am. J. Clin. Nutr. 2019, 109, 1310–1318.
- Ke, Q.; Chen, C.; He, F.; Ye, Y.; Bai, X.; Cai, L.; Xia, M. Association between Dietary Protein Intake and Type 2 Diabetes Varies by Dietary Pattern. Diabetol. Metab. Syndr. 2018, 10, 48.
- Han, Y.; Cheng, B.; Guo, Y.; Wang, Q.; Yang, N.; Lin, P. A Low-Carbohydrate Diet Realizes Medication Withdrawal: A Possible Opportunity for Effective Glycemic Control. Front. Endocrinol. Lausanne 2021, 12, 779636.
- Goldenberg, J.Z.; Day, A.; Brinkworth, G.D.; Sato, J.; Yamada, S.; Jönsson, T.; Beardsley, J.; Johnson, J.A.; Thabane, L.; Johnston, B.C. Efficacy and Safety of Low and Very Low Carbohydrate Diets for Type 2 Diabetes Remission: Systematic Review and Meta-Analysis of Published and Unpublished Randomized Trial Data. BMJ 2021, 372, m4743.
- Jennings, L.; Basiri, R. Amino Acids, B Vitamins, and Choline May Independently and Collaboratively Influence the Incidence and Core Symptoms of Autism Spectrum Disorder. Nutrients 2022, 14, 2896. Available online: https://www.mdpi.com/2072-6643/14/14/2896 (accessed on 26 April 2023).
- Sadeghi, O.; Keshteli, A.H.; Afshar, H.; Esmaillzadeh, A.; Adibi, P. Adherence to Mediterranean Dietary Pattern Is Inversely Associated with Depression, Anxiety and Psychological Distress. Nutr. Neurosci. 2021, 24, 248–259.
- Gangwisch, J.E.; Hale, L.; Garcia, L.; Malaspina, D.; Opler, M.G.; Payne, M.E.; Rossom, R.C.; Lane, D. High Glycemic Index Diet as a Risk Factor for Depression: Analyses from the Women’s Health Initiative. Am. J. Clin. Nutr. 2015, 102, 454–463.
- Chen, L.; Liu, B.; Ren, L.; Du, H.; Fei, C.; Qian, C.; Li, B.; Zhang, R.; Liu, H.; Li, Z.; et al. High-Fiber Diet Ameliorates Gut Microbiota, Serum Metabolism and Emotional Mood in Type 2 Diabetes Patients. Front. Cell. Infect. Microbiol. 2023, 13, 1069954.
- Sheikhi, A.; Siassi, F.; Djazayery, A.; Guilani, B.; Azadbakht, L. Plant and Animal Protein Intake and Its Association with Depression, Anxiety, and Stress among Iranian Women. BMC Public Health 2023, 23, 161.
- Mazaherioun, M.; Saedisomeolia, A.; Javanbakht, M.H.; Koohdani, F.; Zarei, M.; Ansari, S.; Khoshkhoo Bazargani, F.; Djalali, M. Long Chain N-3 Fatty Acids Improve Depression Syndrome in Type 2 Diabetes Mellitus. Iran J. Public Health 2018, 47, 575–583.
- Zheng, L.; Sun, J.; Yu, X.; Zhang, D. Ultra-Processed Food Is Positively Associated with Depressive Symptoms Among United States Adults. Front. Nutr. 2020, 7, 600449.
- Silva, S.A.; do Carmo, A.S.; Carvalho, K.M.B. Lifestyle Patterns Associated with Common Mental Disorders in Brazilian Adolescents: Results of the Study of Cardiovascular Risks in Adolescents (ERICA). PLoS ONE 2021, 16, e0261261.
- Lane, M.M.; Gamage, E.; Travica, N.; Dissanayaka, T.; Ashtree, D.N.; Gauci, S.; Lotfaliany, M.; O’Neil, A.; Jacka, F.N.; Marx, W. Ultra-Processed Food Consumption and Mental Health: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients 2022, 14, 2568.
- Basiri, R.; Seidu, B.; Cheskin, L.J. Key Nutrients for Optimal Blood Glucose Control and Mental Health in Individuals with Diabetes: A Review of the Evidence. Nutrients 2023, 15, 3929.
- Parletta, N.; Zarnowiecki, D.; Cho, J.; Wilson, A.; Bogomolova, S.; Villani, A.; Itsiopoulos, C.; Niyonsenga, T.; Blunden, S.; Meyer, B.; et al. A Mediterranean-Style Dietary Intervention Supplemented with Fish Oil Improves Diet Quality and Mental Health in People with Depression: A Randomized Controlled Trial (HELFIMED). Nutr. Neurosci. 2019, 22, 474–487.
- Sánchez-Villegas, A.; Cabrera-Suárez, B.; Molero, P.; González-Pinto, A.; Chiclana-Actis, C.; Cabrera, C.; Lahortiga-Ramos, F.; Florido-Rodríguez, M.; Vega-Pérez, P.; Vega-Pérez, R.; et al. Preventing the Recurrence of Depression with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil. The PREDI-DEP Trial: Study Protocol. BMC Psychiatry 2019, 19, 63.
