1. The Effects of Diabetes on Anxiety Risk
Growing evidence has established a synergy between diabetes and anxiety
[1][48]. Individuals living with diabetes are at increased risk of developing anxiety because of concerns about dietary restrictions, taking several medication and insulin injections, constant checking of blood glucose, and lack of support from family and medical practitioners
[2][49]. As such, incorporating psychological care in the management of diabetes could aid in reducing anxiety as emphasized by the International Federation of Diabetes
[3][4][50,51]. In patients with diabetes, comorbid anxiety syndromes are correlated with heightened blood glucose levels, high body-mass index (BMI), and greater disability
[5][6][7][52,53,54]. Cure of anxiety is linked to enhanced glycemic control
[8][22], especially among people affected with acute anxiety
[9][23]. Unfortunately, many people with anxiety are undiagnosed, and hence untreated
[10][55]. Undiagnosed anxiety among people with diabetes is concerning because it delays the onset of therapy for these coexisting illnesses and causes patients to become frustrated, which leads to ineffective therapeutic results
[11][56].
The prevalence of anxiety in diabetes seems to be increasing rapidly. In one study, individuals with diabetes had a 20.6% prevalence of anxiety in 2000, and by 2004 the prevalence had risen to 42.2%
[12][57]. In the same study, it was identified that people aged ≥45 were linked to a higher incidence, while females were associated with a more significant occurrence with age ≥45
[12][57]. In another study, compared to women without diabetes, women with diabetes had a greater lifetime incidence of anxiety disorders, with 50% having had an anxiety disorder at some point in their lives
[13][31]. Moreover, both males and females showed a correlation between
type 2 diabetes (T2DM
), obesity, and anxiety, with more than one in three women and one in five men showing signs of anxiety in research findings
[14][58].
Most people with diabetes who are hospitalized have been observed to experience moderate to severe anxiety, sadness, or both throughout their stay
[15][59]. Research studies have demonstrated that anxiety can influence medication adherence in patients with diabetes through its impact on self-efficacy expectations, which refers to an individual’s belief in their ability to successfully carry out specific tasks or activities
[16][60]. This can lead to worsened glucose regulation and greater difficulties in diabetes management
[17][28]. The coexistence of diabetes and anxiety is associated with an elevated risk of developing comorbidities, increased healthcare costs, and early morbidity and mortality
[18][19][61,62].
2. The Effects of Anxiety on Diabetes Risk
Anxiety is a mental health disorder characterized by behavioral syndrome, fear, and feeling a sense of panic, with distinct subtypes of anxiety traits
[20][63]. Research studies show that generalized anxiety disorder (GAD) and panic disorder are the most common mental health conditions
[21][64]. A study examined the use of depression and anxiety screenings and each of their respective components as concurrent predictors of the onset of diabetes
[22][37]. It was noted that 24.9% of the participants with anxiety at baseline developed diabetes over 10 years
[22][37]. Screening for both diabetes and anxiety is highly recommended for patients, as anxiety not only serves as a risk factor for the development of diabetes but can also coexist as a comorbidity
[22][37].
In a recent study to investigate the occurrence of diabetes among individuals with anxiety, it was discovered that diabetes was more common among patients with anxiety as compared to the general population (11.89% vs. 5.92%, odds ratio, 1.23; 95% confidence interval, 1.17–1.28)
[23][65]. The average annual occurrence of diabetes in patients with an anxiety disorder between 2006–2010 was revealed in another study demonstrating a higher prevalence of diabetes among people with anxiety disorders as contrasted with the general population (2.25% vs. 1.11%, risk ratio 1.34; 95% confidence interval, 1.28–1.41)
[23][65].
Delving deeper into the link between anxiety and diabetes, research studies have identified gender as a contributing factor in diabetes prevalence
[24][66]. Women are observed to be more at risk of developing diabetes than men, as women tend to have higher levels of anxiety disorders than men and men handle anxiety-related conditions differently than women
[25][26][67,68]. Other discoveries have also suggested that the higher ratio of women compared to men in diabetes occurrence is due to a higher percentage of women with mental health issues such as depression and anxiety
[25][67]. In a prospective study investigating the association between mental health and diabetes, individuals with reported symptoms of anxiety and depression at baseline had a higher risk of the occurrence of T2DM at a ten-year follow-up
[27][69]. Dealing with anxiety influences eating habits
[28][70] and eventually results in increased adiposity and risk of developing diabetes
[29][71]. Both anxiety and diabetes-related distress are linked to suboptimal glycemic control, decreased adherence to diabetes self-care routines, and an increased likelihood of developing diabetes complications
[30][72]. A summary of the results of related studies on the interrelationship between diabetes, depression, and anxiety have been reported in
Table 1.
3. Exploring the Role of Nutrition in Preventing and Managing Diabetes, Depression, and Anxiety
Poor nutritional status and unhealthy lifestyle habits have been widely acknowledged as established risk factors contributing to the pathogenesis of diabetes
[40][41][42][78,79,80]. For instance, a study of 200,000 participants found that a healthy diet, characterized by a high intake of whole grains, vegetables, fruits, and nuts, and a low intake of red and processed meats, was correlated with a decreased risk of T2DM
[43][81]. Another study found that a diet high in sugar-sweetened beverages and processed foods was associated with an increased risk of diabetes
[44][82]. Moreover, nutrition plays a crucial role in the management of diabetes and related complications
[45][46][47][48][49][50][47,83,84,85,86,87]. A systematic review found that a Mediterranean diet, which is high in vegetables, whole grains, fruits, lean protein, and healthy fats, improved glycemic control and reduced cardiovascular risk factors in patients with T2DM
[51][88]. An alysis of data from three European cohorts and one Canadian cohort including 78,851 participants showed that higher protein intake was correlated with a lower risk of diabetes
[52][89]. More specifically, plant protein intake was significantly and negatively related to the development of diabetes
[53][90]. Other studies found that a low-carbohydrate diet was effective in improving glycemic control and reducing the need for diabetes medication in patients with T2DM
[54][55][91,92].
Similarly, consuming high-quality diets is associated with improved mental health
[56][93]. In a cross-sectional analysis involving a cohort of 3172 adults between the ages of 18 and 55, it was observed that adhering to the Mediterranean diet exhibited a significant correlation with a decreased likelihood of experiencing psychological disorders such as depression, anxiety, and psychological distress
[57][94]. Another study found that a high glycemic index diet is a risk factor for depression
[58][9]. In contrast, it has been shown that a high-fiber diet improves glucose homeostasis, serum lipid profiles, inflammatory chemokines, and depression and anxiety symptoms in patients with T2DM
[59][95]. Evaluating the effects of different sources of protein on the mental well-being of women showed that women who consumed more animal protein had a higher chance of showing symptoms of depression (OR: 2.63; 95% CI: 1.45, 4.71;
p = 0.001), stress (OR: 3.66; 95% CI: 2.06, 6.50;
p < 0.001), and anxiety (OR: 1.83; 95% CI: 1.04, 3.22;
p = 0.03), while no significant association was found between plant protein and these mental disorders
[60][96]. Polyunsaturated fats have also been found to be effective in reducing symptoms of depression and anxiety. For example, a randomized controlled trial found that omega-3 fatty acid supplementation significantly reduced symptoms of depression in patients with diabetes who showed mild to moderate depressive symptoms, independent of metabolic factors and disease duration
[61][97].
Scientific evidence reveals a significant association between the consumption of ultra-processed foods and the occurrence of depression and other mental disorders
[62][63][98,99]. A meta-analysis of prospective studies supports this link, indicating that higher intake of ultra-processed foods is associated with an increased risk of subsequent depression (hazard ratio: 1.22, 95% CI 1.16 to 1.28)
[64][100]. These findings emphasize the potential detrimental impact of consuming ultra-processed foods on psychological outcomes, underscoring the importance of considering dietary choices in promoting mental well-being.
Overall, there is growing evidence to support the link between nutrition, diabetes, and depression and anxiety. A healthy and balanced diet, characterized by a high intake of whole grains, fruits, vegetables, nuts, lean protein, and healthy fats, reduce the risk of diabetes, improve glycemic control in patients with diabetes, prevent and manage related complications, and improve mental health. Furthermore, certain eating behaviors, such as a high intake of fiber, a low glycemic diet, high intake of unsaturated fats including omega-3 fatty acids and plant-based proteins, may play a crucial role in reducing the risk of developing diabetes and anxiety and depression, and can alleviate symptoms of these diseases if they exist. Aside from the effects of eating patterns, certain nutrients play an important role in preventing or alleviating symptoms of diabetes, anxiety, and depression. Deficiencies in certain essential nutrients, including omega-3 fatty acids, vitamin D, B vitamins, zinc, chromium, magnesium, and selenium, have been associated with the development of both diabetes and mental health disorders
[65][101]. In the realm of mental health treatment in patients with diabetes, there is a noticeable scarcity of randomized trials that assess the effectiveness of dietary interventions in these conditions. The Mediterranean diet has proven effective in mitigating symptoms of depression, anxiety, and diabetes when studied separately. However, its effects have not yet been investigated in individuals who simultaneously suffer from both conditions. A notable example of the effects of the Mediterranean diet on the symptoms of anxiety and depression involves a 12-week Mediterranean diet intervention study, which yielded substantial improvements in mood and reduced anxiety among adults diagnosed with major depression
[66][102]. Another randomized controlled trial has reaffirmed the positive impact of a Mediterranean-style diet on mental health, particularly in the context of depression
[67][103]. The Mediterranean diet has also demonstrated its advantages in mitigating several cardiovascular risk factors, with a particular focus on its positive impact on diabetes
[51][88]. These findings highlight the importance of a healthy diet in promoting overall health and well-being, especially for individuals with diabetes and or anxiety and depression.
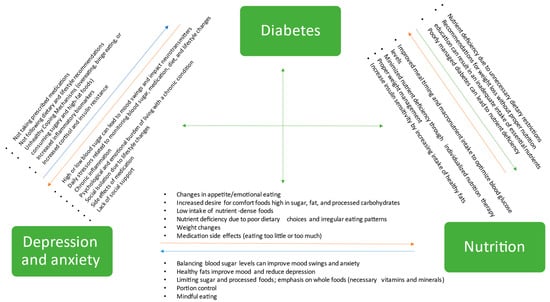
Figure 1 shows the interplay of diabetes, depression, anxiety, and nutrition.
Figure 1.
Interplay of diabetes, depression, anxiety, and nutrition: a comprehensive overview.