Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Andreas M. Matthaiou and Version 2 by Catherine Yang.
Vitamin K is a lipid-soluble vitamin that is normally maintained within appropriate levels by means of dietary intake and bacterial production in the intestinal microflora. It holds a central role in coagulation homeostasis, and thus its depletion leads to hypocoagulation and haemorrhagic diathesis.
- vitamin K
- antibiotics
- vitamin E
1. Introduction
Vitamins are a group of biochemically distinct families of structurally and functionally related organic compounds that are metabolically necessary in trace amounts. Along with essential amino acids, essential fatty acids, and minerals, they constitute the essential nutrients, as they cannot be synthesised in sufficient quantities by the organism per se but rather must be intaken by diet or obtained by symbiosis with the human microbiome [1].
Vitamin K is a family of two major vitamers, i.e., phylloquinone (vitamin K1) that is mainly contained in plants, especially green leafy vegetables, placed on the photosynthetic membranes of chloroplasts in plant cells, and menaquinone (vitamin K2) that is predominantly produced by specific bacterial species of the intestinal microflora, while it is also found in quite lower amounts in animal-derived dietary products. Menaquinone has multiple subtypes characterised as MK-4 through MK-13 based on the length of their isoprenoid side chain. The vast majority of facultative or obligate anaerobes in the gut, such as Escherichia coli, Bacteroides fragilis, Eggerthella lenta, and Lactococcus lactis, produce all different subtypes of menaquinones, whereas their imbalance seen in intestinal microflora dysbiosis can negatively impact the production [2][3][2,3].
Vitamin K deficiency-associated hypocoagulation in a patient with extensive burns receiving meropenem was only reversed upon discontinuation of the broad-spectrum antibiotic therapy [4][11]. Nomoto et al. reported a case of a patient with schizophrenia and catatonia who was hospitalised due to aspiration pneumonia and demonstrated low vitamin K levels and INR prolongation resulting from antibiotic therapy with ampicillin/sulbactam and cefmetazole as well as long-term restriction of food intake due to negativism and stupor [5][12].
2. Vitamin K and Its Function
As a class of lipid-soluble compounds, intact hepatobiliary, pancreatic, and intestinal function is a prerequisite for its unimpeded absorption (Figure 12). The ingested form of vitamin K1 is bound to proteins, which are lysed by pancreatic enzymes in the small intestine. Both free dietary vitamin K1 and bacteria-derived vitamin K2 are solubilised into micelles by bile salts and then are absorbed by enterocytes and incorporated into chylomicrons. It is transferred to the systemic circulation by lymphatic vessels, bypassing the portal circulation, and eventually transported to the liver, where it is incorporated into very low-density lipoprotein (VLDL) and in this form it re-enters the systemic circulation to be distributed in the body [2].
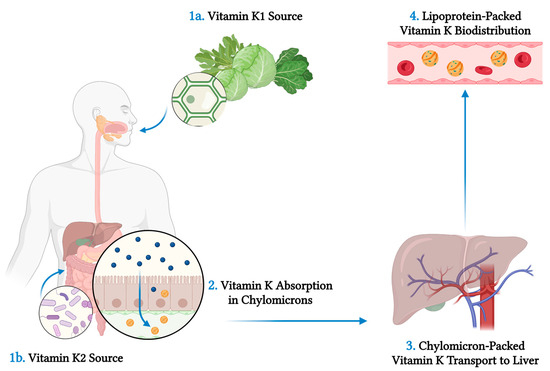
Figure 12. Vitamin K sources and metabolism. Vitamin K1 (phylloquinone) is intaken by consumption of plants, especially green leafy vegetables, as it is found on the photosynthetic membranes of chloroplasts in plant cells (1a). Vitamin K2 (menaquinone) is produced by specific bacterial species in the intestinal microflora (1b). Vitamin K1 is bound to proteins, which are lysed by the action of pancreatic enzymes in the small intestine. Both dietary and bacteria-derived vitamin K is absorbed by enterocytes after it is solubilised into micelles by bile salts (2). Vitamin K is then incorporated into chylomicrons, transferred to the systemic circulation through lymphatic vessels, bypassing the portal circulation, and eventually transported to the liver (3). In the liver, vitamin K is Incorporated into very low-density lipoproteins (VLDL) and in this form it re-enters the systemic circulation and it is distributed to the body (4). Created with: BioRender.com (accessed on 30 August 2023).
Vitamin K holds a central role in coagulation homeostasis. The hydroquinone form of vitamin K acts as a cofactor of the enzyme gamma-glutamyl carboxylase for the γ-carboxylation of glutamic acid residues on several proteins involved in the coagulation cascade, including factors II, VII, IX, and X, as well as proteins C, S, and Z, thus transforming them into their active forms (Figure 23). Molecular oxygen and carbon dioxide are also needed in this reaction, while one molecule of the epoxide form of vitamin K is produced per each glutamic acid residue that becomes carboxylated. The enzyme vitamin K epoxide reductase is responsible for the reduction of vitamin K-2,3-epoxide and the production of vitamin K hydroquinone. Consequently, vitamin K deficiency is mainly associated with hypocoagulation and increased haemorrhagic diathesis, and it also constitutes a therapeutic target for medically-induced anticoagulation, as it is in the case of warfarin and acenocumarol, among other vitamin K antagonists [6][7][4,5].
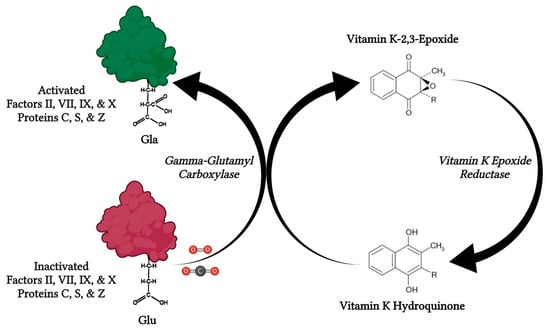
Figure 23. The role of vitamin K in the coagulation pathway. Vitamin K-dependent coagulation factors II, VII, IX, and X as well as proteins C, S, and Z are transformed into their active forms by the carboxylation of the glutamic acid residues in their molecules. In this reaction, which is catalysed by vitamin K-dependent gamma-glutamyl carboxylase, molecular oxygen (O2) and carbon dioxide (CO2) also take part, while vitamin K is oxidised from vitamin K hydroquinone into vitamin K-2,3-epoxide. The levels of the active form of vitamin K are replenished by the action of vitamin K epoxide reductase, which reduces vitamin K-2,3-epoxide into vitamin K hydroquinone. Created with: BioRender.com (accessed on 30 August 2023).
Vitamin K depletion in an otherwise healthy individual is rare, as phylloquinone is widely available in vegetal dietary products, menaquinone is produced by the intestinal microflora, and vitamin K is recycled within cells. However, hypovitaminosis K is common in newborns, so that administration of vitamin K prophylaxis at birth is necessitated to avoid it. Major causes of vitamin K deficiency include decreased dietary intake, decreased absorption by the gastrointestinal tract, hepatic dysfunction, and interactions with medications. Prolonged fasting or starvation, abused alcohol consumption, and prolonged parenteral nutrition without vitamin K supplementation can all contribute to decreased vitamin K intake. Malabsorptive states can lead to impaired vitamin K absorption and can be attributed to impaired bile or pancreatic secretion, such as in cystic fibrosis, primary biliary cholangitis, primary sclerosing cholangitis, and biliary atresia, as well as to intestinal diseases, such as celiac disease, inflammatory bowel disease, and short bowel syndrome, especially in case of terminal ileum involvement. Vitamin K depletion is also seen in chronic liver disease, while decreased hepatic production of coagulation factors can additionally lead to coagulation impairment in this condition. Finally, antibiotics and high vitamin E doses can contribute to hypovitaminosis K.
