Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Alfred Zheng and Version 1 by Tadej Durič.
Gastrointestinal (GI) endoscopy forms an important part of the daily practice of a gastroenterologist. Its use and applicability nowadays shift from diagnostic to therapeutic fields, and it forms a significant part of the workload of the GI practitioner. Ergonomics in GI endoscopy plays an important role in occupational injury prevention. Due to a higher volume of procedures, the problem with musculoskeletal injuries is becoming bigger and everyday more present among fellow gastroenterologists.
- GI endoscopy
- endoscopy
- occupational injury
1. Introduction
Gastrointestinal (GI) endoscopy forms an important part of the daily practice of a gastroenterologist. Its use and applicability nowadays shift from diagnostic to therapeutic fields, and it forms a significant part of the workload of the GI practitioner. Having in mind that the basic design of a flexible endoscope remained practically the same for the last couple of decades [1] and considering the complexity of modern endoscopic procedures, musculoskeletal injuries amongst endoscopists are on the rise. According to Young et al., a systematic review of 13 studies showed that 39–89% of surveyed endoscopists reported pain and/or injuries related to endoscopy. Common areas of pain were the back (15–57%), neck (9–46%), shoulders (9–19%), elbows (8–15%) and hands/fingers (14–82%). Risk factors included procedure volume, time spent performing endoscopy, cumulative time in practice and endoscopist age. Experimental studies showed that the forces and loads placed on endoscopists’ bodies during procedures place them at risk of occupational injury. Areas of pain differed between novice and experienced endoscopists, implying separate mechanisms of injury [2]. Villa et al. depicted the importance of proper endoscopy training in young fellows. Among the two researched groups, the one without formal ergonomic training reported a significantly higher percentage of musculoskeletal injuries related to endoscopy [3,4][3][4]. With this emerging and growing problem, a set of basic recommendations was published by Amandeep K. Shergill [5].
2. Endoscopy with Regard to Reducing and Preventing Musculoskeletal Injuries
2.1. Robotics
When talking about ergonomic challenges in GI endoscopy, robotics offers many solutions and possibilities [22,23][6][7]. Robotics is a unique and special technology in the field of gastrointestinal endoscopy that offers new diagnostic and therapeutic possibilities. However, it is also a method that can improve ergonomics and thus reduce the burden on the musculoskeletal systems of physicians during endoscopic procedures. Visconti et al. [24][8] divides the area of robotics in GI endoscopy into two basic approaches: that which aims to improve forceps handling and stability and that which aims to provide active movement. Furthermore, a more detailed stratification can be made in the three following directions:
-
Platforms capable of high degrees of freedom in forceps manipulation for ESD (endoscopic submucosal dissection) and NOTES (natural orifice transluminal endoscopic surgery).
-
Active introduction of the endoscopes to reduce the influence of the operator’s ability and to reduce the discomfort and pain referred by the patients.
Looking from the perspective of ergonomic change, platforms capable of high degrees of freedom in forceps manipulation for ESD and NOTES demand two-people manipulation. In each platform with high degrees of freedom in forceps manipulation for ESD and NOTES, there are slight variations; however, this layout totally changes the approach in therapeutic endoscopy, ergonomically and organizationally. It unburdens the endoscopist from the classical stance and has practically no resemblance to the GI endoscopy performed with standard endoscopes. The approach demands two-people manipulation. The first physician manipulates the robot, usually in seating position, and the second physician manipulates the endoscope (Figure 1).
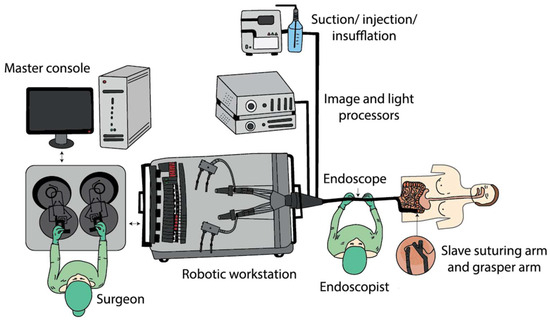
Figure 1.
Layout of an endoscopic robotic platform.
Pioneer platforms with high degrees of freedom in forceps manipulation are the MASTER platform (developed by the Nanyang Technological University and the National University of Singapore), STRAS/Anubiscope (developed by the Research Institute against Digestive Cancer (IRCAD) with Karl-Storz) and Endo-Samurai (developed by Olympus Medical Systems) [24][8]. However, its applicability in everyday practice is limited due to the high cost, complexity and long learning curve. Nevertheless, the concept offers an idea worth pursuing in tackling the ergonomic issue.
Systems which are designed for active introduction of the endoscope incorporate devices which propel or introduce the endoscope mechanically. This can be achieved with mechanisms that are attached to the classical endoscope, or the endoscope design can be altered or redesigned. In his review article, Lim divides flexible robotic systems into four categories: robot-assisted flexible endoscopy for manoeuvring, robotic flexible endoscopy with therapeutic functions, active flexible colonoscopy and active capsule endoscopy [25][9]. A summary of available robotic endoscopic systems is provided, including the need for further development and clinical applicability.
Li and Chiu provide a stratification of the field in a similar fashion: the first category is robot-assisted rigid endoscopy for minimally invasive surgery, i.e., the rigid endoscope is held and manipulated by a robot arm. The second category is robot-assisted flexible endoscopy for GI tract inspection, i.e., the flexible endoscope is held and manipulated by a robotic device. The third category is active GI endoscopy, which includes active flexible colonoscopy and active capsule endoscopy [26][10]. A clear trend of introducing robotics in everyday practice is outlined, offering solutions in the technical and ergonomic area.
In the most recent publication on robotics in gastrointestinal endoscopy by Kim et al., a similar approach was used. However, certain robotic projects from the previous articles were discontinued; the latest robotic systems were divided into the three following categories: The first category includes robot-assisted therapeutic devices that assist advanced endoscopic procedures. This category includes robotic endoscopic multitasking platforms and robotic add-on devices. The second category is the robot-assisted colonoscopy system—a robotic-driven colonoscope that automatically navigates in the colon and an auxiliary device that assists the conventional colonoscope. The last category is robotic capsule endoscopy.
The idea of capsule endoscopy changes the approach to endoscopy in comparison to conventional or robotic endoscopy. The process of capsule endoscopy eliminates the previously outlined musculoskeletal injuries connected to repetitive strain injuries. However, currently available endoscopic capsules lack the possibility of therapeutic interventions and serve mainly as diagnostic tools [28][11].
An almost unanimous division of the robotics area is provided by all of the abovementioned authors. Their work mainly focuses on technical issues with subtle insinuations to change the endoscope design and layout and therefore also addresses the ergonomic challenge. All of the abovementioned robotic systems are a novelty in GI endoscopy. One might argue that solutions are sought only in colonoscopy [29,30][12][13]. However most occupational injuries in GI endoscopy arise from repetitive actions with high-force manoeuvres [1,12][1][14]. From an ergonomic standpoint, the systems presented practically eliminate repetitive strain injuries due to their robotic-joystick properties. The downside is the high cost of the equipment, its uniqueness and its applicability in everyday practice. If one is to imagine the number of endoscopy units in the world and the number of procedures performed daily, implementing a system with disposable colonoscopes with robotic guidance systems poses an incomprehensible challenge.
The redesign of the endoscope is a crucial step in achieving better ergonomic conditions for endoscopists. However, an easier way is to implement robotic assistance with the existing traditional endoscope. In their review, Kim et al. present solutions using add-on platforms and the master–slave concept in conventional endoscopes. It is a lot easier and conventional to combine robotic assistance; however, the limitations in comparison with robotic platforms are greater. The add-ons used usually are less capable of triangulation of instruments and tissue manipulation compared to the robotic endoscopic multitasking platform. Their exchangeability, possibility of sterilization and low cost offer an interesting approach in preventing musculoskeletal injuries [27][15].
2.2. “Hands-Free” Endoscopy
As conceptualized by Dr. Binmoeller in 2004, the ScopeDoc (Figure 2) was the first device of its kind designed for “hands-free” endoscopy to reduce stress and fatigue from flexible endoscopy. The fatigue and stress result from having to carry the sheer weight of the endoscope and having to steer the endoscope with the hands. The ScopeDoc transfers the weight of the endoscope from the hand to the body. Subtle changes in body position are transferred to the endoscope shaft and the endoscope tip, enabling the endoscopist to steer the endoscope with the body rather than the hands. The concept of the device was developed further, and clinical trials with EMG of specific muscles of the left and right arms, torso and back are in progress [31,32,33][16][17][18]. The first results are confirming tension relief in left trapezoid and biceps muscles and a significant increase in microbreaks in the muscles when using the holder. This combination offers an alternative solution to robotics. Its simplistic design and idea allow widespread use. On the downside, it offers a solution only for the left arm and body posture, while the right arm still operates with conventional movements [31][16].

Figure 2.
The ScopeDoc (COOK Medical).
2.3. Personal Care Strategies—Floor Mats and Cushioned Insoles
Prolonged standing on a hard surface is a known trigger for discomfort, resulting in suboptimal performance, leg pain, etc. In their research, Wiggerman and Keyserling demonstrated the positive effect of cushioned floor mats and their effect on discomfort relief and better work performance [34][19]. Their use in endoscopy can be beneficial to all endoscopists, despite not being a “true” endoscopic accessory connected to endoscope redesign or function [35][20]. Standing in cushioned insoles has been suggested to create subtle muscular movement, reducing musculoskeletal pain, improving blood flow and decreasing discomfort and fatigue [36][21]. The fundamental principle behind using anti-fatigue mats and insoles is to provide a supportive interface between the floor and the feet and to optimize bodyweight distribution [37][22]. When performing endoscopy, the body posture is predominantly in the upright standing position; hence, the use of cushioned insoles proves itself useful in the prevention of musculoskeletal injuries during endoscopy.
References
- Shergill, A.K.; Harris Adamson, C. Failure of an engineered system: The gastrointestinal endoscope. Tech. Gastrointest. Endosc. 2019, 21, 116–123.
- Yung, D.E.; Banfi, T.; Ciuti, G.; Arezzo, A.; Dario, P.; Koulaouzidis, A. Musculoskeletal injuries in gastrointestinal endoscopists: A systematic review. Expert Rev. Gastroenterol. Hepatol. 2017, 11, 939–947.
- Villa, E.; Attar, B.; Trick, W.; Kotwal, V. Endoscopy-related musculoskeletal injuries in gastroenterology fellows. Endosc. Int. Open 2019, 7, E808–E812.
- Austin, K.; Schoenberger, H.; Sesto, M.; Gaumnitz, E.; Teo Broman, A.; Saha, S. Musculoskeletal Injuries Are Commonly Reported Among Gastroenterology Trainees: Results of a National Survey. Dig. Dis. Sci. 2019, 64, 1439–1447.
- Shergill, A.K.; McQuaid, K.R.; Rempel, D. Ergonomics and GI endoscopy. Gastrointest. Endosc. 2009, 70, 145–153.
- Yeung, B.P.M.; Chiu, P.W.Y. Application of robotics in gastrointestinal endoscopy: A review. World J. Gastroenterol. 2016, 22, 1811–1825.
- Kume, K.; Sakai, N.; Goto, T. Development of a novel endoscopic manipulation system: The Endoscopic Operation Robot ver.3. Endoscopy 2015, 47, 815–819.
- de Carvalho Visconti, T.A.; Otoch, J.P.; de Almeida Artifon, E.L. Robotic Endoscopy. A Review of the Literature. Acta Cir. Bras. 2020, 35, e202000206.
- Lim, S.G. The development of robotic flexible endoscopic platforms. Int. J. Gastrointest. Interv. 2020, 9, 9–12.
- Li, Z.; Chiu, P.W.Y. Robotic Endoscopy. Visc. Med. 2018, 34, 45–51.
- Bianchi, F.; Masaracchia, A.; Shojaei Barjuei, E.; Menciassi, A.; Arezzo, A.; Koulaouzidis, A.; Stoyanov, D.; Dario, P.; Ciuti, G. Localization strategies for robotic endoscopic capsules: A review. Expert Rev. Med. Devices 2019, 16, 381–403.
- Pullens, H.J.; van der Stap, N.; Rozeboom, E.D.; Schwartz, M.P.; van der Heijden, F.; van Oijen, M.G.; Siersema, P.D.; Broeders, I.A. Colonoscopy with robotic steering and automated lumen centralization: A feasibility study in a colon model. Endoscopy 2016, 48, 286–290.
- Kang, M.; Joe, S.; An, T.; Jang, H.; Kim, B. A novel robotic colonoscopy system integrating feeding and steering mechanisms with self-propelled paddling locomotion: A pilot study. Mechatronics 2021, 73, 102478.
- Ridtitid, W.; Coté, G.A.; Leung, W.; Buschbacher, R.; Lynch, S.; Fogel, E.L.; Watkins, J.L.; Lehman, G.A.; Sherman, S.; McHenry, L. Prevalence and risk factors for musculoskeletal injuries related to endoscopy. Gastrointest. Endosc. 2015, 81, 294–302.e4.
- Kim, S.H.; Choi, H.S.; Keum, B.; Chun, H.J. Robotics in Gastrointestinal Endoscopy. Appl. Sci. 2021, 11, 11351.
- Duric, T. Ergonometry in Endoscopic Procedures: Prevention of Musculoskeletal Injuries During Endoscopic Procedures by Using Belt-Like Manouvring Device with Joystick Capabilities. Endoscopy 2021, 52, S160.
- Luttmann, A.; Jäger, M.; Laurig, W. Electromyographical indication of muscular fatigue in occupational field studies. Int. J. Ind. Ergon. 2000, 25, 645–660.
- Albayrak, A.; van Veelen, M.A.; Prins, J.F.; Snijders, C.J.; de Ridder, H.; Kazemier, G. A newly designed ergonomic body support for surgeons. Surg. Endosc. 2007, 21, 1835–1840.
- Wiggermann, N.; Keyserling, W. Effects of Anti-Fatigue Mats on Perceived Discomfort and Weight-Shifting During Prolonged Standing. Hum. Factors 2013, 55, 764–775.
- Noor, S.N.A.M.; Ahmad, I.N.; Wahab, N.A.; Ma’arof, M.I.N. A Review of Studies Concerning Prolonged Standing Working Posture. Adv. Eng. Forum 2013, 10, 131–136.
- King, P.M. A comparison of the effects of floor mats and shoe in-soles on standing fatigue. Appl. Ergon. 2002, 33, 477–484.
- Speed, G.; Harris, K.; Keegel, T. The effect of cushioning materials on musculoskeletal discomfort and fatigue during prolonged standing at work: A systematic review. Appl. Ergon. 2018, 70, 300–314.
More
