2. HER2 as an Oncogenic Molecular Driver
HER2 is an oncogenic membrane-spanning receptor of a signaling pathway located in the intracellular and extracellular domains (ECD). HER2 belongs to the family of epidermal growth factor receptor tyrosine kinases known as EGFR or ErbB, encompassing four structurally analogous receptors including HER1, HER2, HER3, and HER4
[20][21][20,21]. When HER2 is overexpressed, it generates a rearrangement of the HER family of dimers, leading to a significant augmentation of the HER2–containing heterodimers and homodimers and enabling the HER2 receptor activation by dimerization with another HER family member
[22][23][22,23]. Hence, by eliciting a cascade of transduction signals partaking in the PI3K/Akt/mTOR and MAPK molecular alleyways, it leads to the regulation of cellular proliferation and differentiation, thus triggering tumor growth
[23].
3. Classification of HER2+ Tumors
Based on the American Society of Clinical Oncology and the College of American Pathologists (ASCO/CAP) guidelines, HER2+ is defined as IHC 3+ (circumferential membrane staining including >10% of cells) or IHC 2+ combined with HER2 amplification by an ISH assay of the invasive component of a BC specimen using single/dual-probe ISH. There are intricacies for determining HER2 positivity based on the ISH pattern. Nonetheless, to summarize, a single signal probe ISH is based on the average HER2 copy number and is considered negative when the average HER2 copy number is <4.0 signals/cell and positive when the average HER2 copy number is ≥6.0 signals/cell. However, when the estimated HER2 is ≥4.0 and <6.0 signals/cell, the HER2/chromosome enumeration probe 17 (CEP17) ratio should be ≥2.0 in order for HER2 to be considered positive
[24].
4. Treatment Strategies for HER2+ Breast Cancer
4.1. Monoclonal Antibody against HER2
Trastuzumab was the first targeted humanized mAB against HER2 to be approved by the US Food and Drug Administration (FDA)
[25][26][25,26]. By binding to domain-4 on the juxtamembrane region of the HER2 ECD, trastuzumab disrupts ligand-independent downstream signaling pathways to the intracellular environment, triggering antibody-dependent cell-mediated cytotoxicity. Through immune mechanisms, where antibody-coated cells target the surface of tumor-derived antigens, cascade processes are prompted to inhibit cell cycle arrest and tumor angiogenesis via antibody-dependent cellular toxicity (ADCC)
[27][28][27,28].
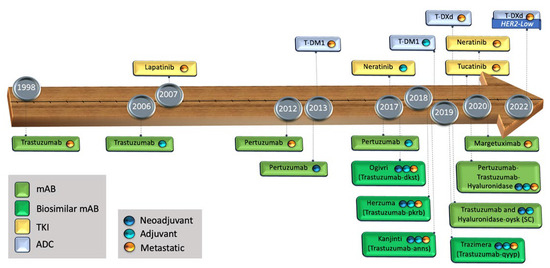
The advent of trastuzumab has been a remarkable breakthrough in the history of BC, due to its ability to prolong survival and improve quality of life (
Figure 1). Trastuzumab has dramatically changed the trajectory of HER2+ populations, not only in BC but in other malignancies such as those involving the gastro-esophageal junction, colorectal, and endometrial carcinomas
[29][30][31][32][29,30,31,32].
Figure 1. Timeline of the FDA-approved targeted treatments against the HER domains. mAB: monoclonal antibody, TKI: tyrosine kinase inhibitor, ADC: antibody drug conjugate, SC: sub-cutaneous.
4.2. Dual HER2 Blockage with mABs
Pertuzumab is a recombinant humanized mAB binding to subdomain II of the ECD of HER2, inhibiting dimerization and subsequent receptor ligand-dependent signaling
[3]. In contrast to trastuzumab, pertuzumab interrupts the HER heterodimerization on the HER1 (or EGFR), HER2, HER3, and HER4 domains, stopping the molecular transduction of downstream tumor signaling
[33][38]. Trastuzumab and pertuzumab have complementary mechanisms of action and potential synergist effects on antitumor activity when administered together
[33][34][38,39].
4.3. Antibody–Drug Conjugate
Ado-trastuzumab emtansine (T-DM1) was the foremost antibody–drug conjugate (ADC) targeting HER2 to be approved by the FDA
[35][36][40,41] (
Figure 1). T-DM1 is composed of the monoclonal antibody trastuzumab linked to a microtubule polymerization inhibitor, mertansine (DM1), via a non-cleavable thioether linker
[37][38][42,43].
4.4. TKIs
The tyrosine kinase inhibitors (TKIs) lapatinib and neratinib, through competitive molecular mechanisms, target the catalytic kinase in the HER2 intracellular domain, promoting a disruption of the ATP phosphorylation-dependent processes, which leads to cancer cell angiogenesis disruption and tumor shrinkage. While lapatinib is a reversible TKI on the EGFR and HER2 domains, neratinib is an irreversible TKI targeting the HER1, HER2, and HER4 pathways
[8][39][8,44].
5. Defining Risk Categories
While achieving pCR is the most valuable predictive factor associated with better recurrence-related results, pathologic residual disease (pRD) indicates a higher risk for the poorest survival and for disease relapse
[40][45]. At baseline, HER2+ BC patients with tumors > 20 mm and with the detection of LN+ prior to surgery, or postoperatively (following NAC with trastuzumab), and with residual tumors > 10 mm or LN+ are highly associated with early relapse events
[40][41][42][45,46,47]. When there is pRD in the breast only, tumors > 10 mm have an estimated increased recurrence risk of 16% when compared to sub-centimeter tumor sizes or pCR. When pRD is seen in LNs, there is an increased relapse risk by at least 50% in those with ≥2 LNs+ when compared to those with 1 LN+
[41][46].
Other contributory factors related to increased risk and linked to worse recurrence rates are an age less than 50 years at the time of diagnosis, low levels of tumor-infiltrating lymphocytes (TILs), as well as a body mass index (BMI) ≥ 25
[40][43][45,48].
The BC recurrence risk attributed to the ER status appears to be linked to the time at which chemotherapy is delivered, whether it is administered before or after surgery, but more supportive data around this are needed. HER2+ BC with ER− is more likely to achieve pCR as compared to the ER+ phenotype, reflecting higher chances of relapse in the latter group
[9][15][9,15]. However, in BC patients with pRD, many studies did not find a correlation between the ER status and OS or DFS
[44][45][46][49,50,51]. Nevertheless, though less prone to attaining a tumor response due to decreased chemotherapy sensitivity, ER+ HER2+ patients who achieve pCR are likely to have a favorable prognosis
[40][45].
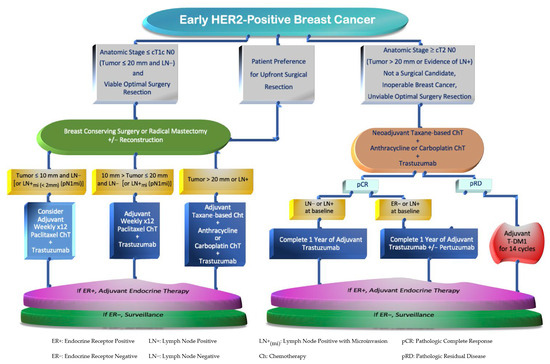
For physician decision making, it is important to identify which patients will benefit from systemic treatment upfront versus after surgery. These decisions are typically determined by the BC risk of recurrence. The evaluation of factors such as breast cancer staging based on radiological and clinical–pathological features characterizing the breast tumor size, nodal involvement, and HER2 levels of expression is required
[47][52]. For example, BC with uninvolved LN and tumors measuring up to 20 mm, which correspond to anatomic stages (by The American Joint Committee on Cancer—AJCC
[48][53]) I to IIA, are preferred for upfront surgery, followed by adjuvant systemic treatment
[49][54]. Conversely, high-risk patients with larger tumors (≥T2 stage or >20 mm) and/or with axillary LN+ involvement, encompassing BC stages IIB and III, are mostly suitable for a multimodal disciplinary approach which consists of the following: neoadjuvant systemic therapy, followed by radical or conservative breast surgical resections, usually along with LN assessment with sentinel LN biopsy or axillary LN dissection
[49][50][54,55]. These approaches should be followed by adjuvant systemic treatment and, if appropriate, the subsequent administration of endocrine and local radiation therapies
[47][52]. The selection between HER2 blockers to be given after surgery would depend on microscopic pathology appraisal, where patients with pRD on the surgical specimen should be considered for adjuvant treatment modalities
[9] (
Figure 2).
Figure 2.
Flowchart of Systemic Therapy Strategies in Early HER2-Positive Breast Cancer.
6. Adjuvant Treatment
6.1. Very Low-Risk HER2+
Most randomized controlled trials (RCTs) for early HER2+ BC excluded patients with tumors ≤ 10 mm with no LN involvement (T1abN0)
[51][56]. The data available for this population are mostly derived from non-randomized studies with a reduced sample size in most cases
[52][53][36,57]. Hence, it is not clear whether small HER2+ tumors should be treated with standard-of-care single-agent chemotherapy and trastuzumab. A recent systematic review and meta-analysis, including 12 studies and almost 7000 patients, investigated whether patients with T1abN0 HER2+ BC would benefit from adjuvant trastuzumab. A significant DFS improvement was seen in patients treated with versus without chemotherapy and trastuzumab. The absolute increased benefit of trastuzumab over no trastuzumab was 7% at a 5-year DFS and less than 1% at the 3-year OS. However, even in those patients who did not receive trastuzumab or chemotherapy, their prognosis was reasonably good, with a 5-year OS of 95.9% and a DFS of 88.3%
[54][58]. Only a few studies evaluated the effect of chemotherapy plus trastuzumab in small HER2+ tumors based on the ER status, suggesting that a larger population sample is needed to ascertain robust conclusions regarding these subgroups
[54][55][58,59]
6.2. Low-Risk HER2+
A meta-analysis that assembled data from five trials and included 4220 patients with breast tumors ≤ 20 mm (pT1c) evaluated participants who were randomized to receive adjuvant trastuzumab versus no trastuzumab. With a median follow up of 8 years, there was a substantial OS and DFS advantage for those treated with trastuzumab. However, the compiled population in this meta-analysis was highly heterogeneous, as it included patients with LN– and LN+ as well as different lengths of trastuzumab administration varying from 9 weeks to 24 months
[56][60].
In summary, very low-risk and low-risk HER2+ BC, defined as anatomic stage T1ab and T1cN0, respectively, with a clinical or radiological breast tumor size estimation of 20 mm or less and with no suspicious LN or biopsy-proven LN at baseline, are candidates for receiving 12 cycles of adjuvant paclitaxel chemotherapy and trastuzumab for 1 year, as long as the surgical findings are consistent with the pre-surgical evaluation.
6.3. High-Risk HER2+
In the higher-risk groups comprising BC stages II or III, the combined analysis of the phase III trials NSABP B-31 and NCCTG N9831 showed that, regardless of the breast tumor size, ER status, LN involvement, or age groups, trastuzumab had a substantial OS and DFS benefit in all subgroups
[15][29][15,29]. In these trials, women with HER2+ BC, with LN+ or LN–, and with high-risk features (defined as ER+ with a tumor size > 20 mm and ER− with tumors > 10 mm) were randomly allocated to receive adjuvant chemotherapy with doxorubicin and cyclophosphamide, followed by weekly paclitaxel (AC→T), plus/minus 1 year of trastuzumab. At 8.4 years, those who received trastuzumab had a significant risk reduction in mortality of 37% (95% CI, 0.54–0.73) and a reduction in relapse events of 40% (95% CI, 0.53–0.68)
[29].
It is a viable option to deliver systemic therapy in the adjuvant setting for HER2+ BC patients with high-risk features, with clinical or radiological staging ≥ T2 or pathological evidence of LN+. However, this high-risk population would potentially benefit more by receiving treatment in a neoadjuvant scenario. This is because up to 65% of them could achieve pCR post-NAC and hence derive additional long-term survival benefits
[11][12][11,12].
6.4. Adjuvant Dual HER2 Blockage
The first phase III RCT to use the dual HER2 blockage trastuzumab and pertuzumab (H+P), in combination with taxane-based chemotherapy, was the CLEOPATRA trial, which included patients with metastatic or unresectable HER2+ BC. This study showed a survival extension of 16.3 months with the dual combination when compared to trastuzumab alone
[57][66]. In an attempt to replicate these results in the adjuvant scenario, the phase III, double-blinded randomized APHINITY trial tested trastuzumab plus/minus pertuzumab in patients with LN+ or high-risk LN– HER2+ BC
[58][67]. There was no significant OS advantage between trastuzumab alone and that in combination with pertuzumab, with HR 0.83 (95% CI, 0.68–1.02). The updated 8-year OS was 92.7% for dual combination therapy H+P and 92.0%, for single therapy. There was a relative IDFS improvement in reducing distant and locoregional recurrence of 23% (95% CI, 0.66–0.91). In the analysis of subgroups, there was an absolute IDFS benefit of 4.5% (95% CI, 0.59–0.87) in patients with LN+ and one of 3% (95% CI, 0.59–0.92) in those with ER−
[59][68].
7. Neoadjuvant Treatment
Candidates who derive the greatest advantage from receiving upfront systemic therapy and trastuzumab are those with high-risk features in HER2+ BC, patients with inoperable diseases, or those with an unfeasible optimal surgical resection at baseline.
In the randomized phase III NOAH trial, women with HER2+ BC with locally advanced or inflammatory disease were assigned to receive NAC alone versus NAC with trastuzumab followed by 1 year of maintenance trastuzumab. At 5 years, the absolute difference in EFS was 15% (HR 0.64 (95% CI, 0.44–0.93)), and in BCSS, it was 13% (HR 0.59 (95% CI, 0.37–0.92)). These outcomes favored those treated with NAC containing trastuzumab. In these trials, there was a high correlation between pCR and enhanced EFS in patients who received trastuzumab
[60][70].
Knowing that pCR is a potential surrogate marker associated with improved survival outcomes, a systematic review and meta-analysis of seventy-eight RCTs, with 25,150 HER2+ BC patients treated with NAC, showed a significant association between pCR and enhanced OS. The OS at 3 and 5 years revealed a significant mortality rate reduction in those who had pCR with a respective HR of 0.25 (95% CI, 0.13–0.47) and 0.26 (95% CI, 0.20–0.33)
[13]. When compared to patients who had pRD, the 5-year absolute OS advantage in those who reached pCR was 13.5%, and the event-free survival was 19.6%. These results highlighted the importance of pCR as a prognostic and surrogate factor for longer survival. Although, over time, as the survival differences amplify in those who had pCR versus pRD, a precise estimate of the survival advantage remains difficult to quantify
[13][14][13,14]. Notably, many trials explored whether adding a second HER2 blocker to trastuzumab in the neoadjuvant setting would maximize the treatment response, further highlighting the importance of optimizing pCR rates in HER2+ BC.
8. Adjuvant HER2 Therapy in Postoperative Pathologic Residual Disease
Knowing that patients who did not achieve pCR have worse BC outcomes, the phase III KATHERINE trial attempted to improve relapse rates in HER2+ BC patients who had pRD on the surgical specimen following taxane-based NAC (with or without anthracycline) plus trastuzumab. Notably, almost 20% of the accrued study population received dual HER2+ monoclonal antibodies in the neoadjuvant setting. The participants were assigned to receive 14 cycles of T-DM1 or trastuzumab, postoperatively. At 3 years, 88.3% of patients treated with T-DM1 and 77.0% of those treated with trastuzumab were free of recurrence, translating to a 50% risk reduction of combined invasive BC recurrence and death events in the T-DM1 arm versus the control arm with trastuzumab (HR 0.50 (95% CI, 0.39–0.64)). The OS analysis was premature (HR 0.70 (95% CI, 0.47–1.05)), as a sufficient number of death events were not statistically seen in both study arms
[61][80]. AEs of grade three and of any grade were 5.5% and 10.3% higher, respectively, in the T-DM1 group
[46][61][51,80].
The ExteNET is a phase III RCT that recruited 2,840 participants with stages I–IIIc HER2+ BC. This study investigated whether extending the adjuvant dual blockage therapy provides a survival advantage. Patients who had received standard-of-care surgery and chemotherapy and had completed adjuvant trastuzumab were enrolled to receive 1 year of neratinib versus placebo
[62][63][81,82]. The most common AE of neratinib was diarrhea, with 40% being classified as a grade 3 event. The iDFS at 5 years was 90.2% and 87.7% in the intervention and control groups, respectively. A subgroup analysis of 1,631 ER+ patients revealed a 40% iDFS risk reduction in those treated with neratinib (95% CI, 0.43–0.83)
[63][82]. Among the ER+ group, which had an early initiation of neratinib/placebo within 1 year after the completion of adjuvant trastuzumab, the absolute iDFS improvement was 5.1% (HR 0.58 (95% CI, 0.41–0.82))
[64][83]. Finally, the 8-year OS analysis showed no benefit with the usage of neratinib as an extended duration of adjuvant HER2 therapy (HR 0.95 (95% CI, 0.75–1.21)). At the 8-year mark, the subgroup analysis of OS revealed no substantial differences between the study arms in the ER+ and ER− groups
[65][84].
9. Chemotherapy Backbone with versus without Anthracycline
In terms of chemotherapy, the optimal strategies comprise taxane-based regimens plus/minus an anthracycline component. The Dutch study TRAIN-2, a controlled phase III trial, randomized patients with stage II–III HER2+ BC to receive NAC with or without anthracycline. The anthracycline arm consisted of three cycles of FEC, followed by six cycles of carboplatin with paclitaxel. In the non-anthracycline groups, the patients received six or nine cycles of carboplatin with paclitaxel. Both parties received H+P
[66][85]. At 3 years, the estimated EFS was 92.7% versus 93.6% (HR 0.90 (95% CI, 0.50–1.63)), and the OS was 97.7% versus 98.2% (HR 0.91 (95% CI, 0.35–2.36)) in those who received NAC with versus without anthracycline, respectively. These results revealed that HER2+ BC patients can safely have anthracycline omitted without compromising BC prognosis
[66][67][85,86]. No statistical difference was seen in the pCR rates between the two groups. In those treated with anthracycline, there was a higher incidence of febrile neutropenia and LVEF impairment (7.7% versus 3.2%;
p = 0.04), when compared to treatment without anthracycline. In this trial, cardiac dysfunction was defined as a drop of ≥10% in LVEF from baseline or a decrease of <50% of the total LVEF. However, symptoms secondary to cardiac dysfunction were rare in both groups, with 1% versus 0, respectively. Regardless of the ER or LN status, these results support that the omission of anthracycline within NAC can be a safe and effective option and does not compromise a patient’s BC outcomes
[66][67][85,86].
In the randomized phase III BCIRG 006 trial, HER2+ BC patients were allocated to receive one of the following three adjuvant treatment regimens: AC→T, AC→TH, or TCH. Approximately 72% of the accrued trial participants had LN+, from which a third of the total population had LN+ ≥ 4 axillary nodes. No significant differences in OS or DFS were identified between the two study arms containing trastuzumab that compared anthracycline versus non-anthracycline chemotherapy
[68][69][35,87].
A recently published systematic review and meta-analysis included 11 RCTs with a total of 1,155 patients comparing NAC with versus without anthracycline in the HER2+ BC population. There was no difference in pCR rates between those comparators (OR 0.95 (95% CI, 0.61–1.48)). Amid these two arms, there was no difference in the rates of breast-conserving surgery (OR 1.18 (95% CI, 0.93–1.49)). However, a critical point to note in this meta-analysis was the heterogeneity of the population, comprising patients with a broad range of risk factors that could have potentially affected the study results
[70][88].
The phase II TRYPHAENA trial, which was primarily focused on assessing cardiac safety, included 225 women with HER2+ BC who were to receive NAC with dual HER2 mAB blockage. Patients who were allocated to the anthracycline group received the FEC→DH+P regimen. The anthracycline sparring group comprised six cycles of TCH+P
[71][89]. NAC promoted similar pCR event rates and recurrence outcomes of DFS and PFS between the study groups. And those who were exposed to anthracyclines were more likely to develop LVEF dysfunction when compared to patients exposed to the anthracycline-free regimen
[71][72][89,90].
Hence, in high-risk HER2+ BC populations, doublet platinum taxane-based chemotherapy regimens, such as carboplatin with docetaxel, have been demonstrated to be a comparable alternative in select patients who should be spared from receiving anthracycline.
10. Optimal HER2 Treatment Duration
With regard to the escalation and de-escalation of treatment, the HERA trial did not show a benefit when adjuvant trastuzumab was extended to 2 years, compared to the 1-year standard duration
[73][91]. Three of the most relevant non-inferiority trials with similar study designs, comparators, and endpoints investigated the optimal duration of mABs against HER2, comparing a 6- versus 12-month administration of adjuvant trastuzumab
[74][92]. While the PERSEPHONE study achieved its prespecified non-inferior boundaries for OS and DFS at 4 years (HR 1.07 (95% CI, 0.93–1.24),
p = 0.011), the PHARE and HORG trials failed to support that the treatment with a shorter schedule is non-inferior to the standard duration at the 7.5-year and 3-year analyses, respectively
[75][76][77][93,94,95]. To tiebreak these contrasting results, a high-level evidence meta-analysis compiled RCTs comparing 6 versus 12 months of adjuvant trastuzumab and emphasized that the shorter treatment length conferred a significantly reduced DFS benefit, with an HR of 1.22 ((95% CI, 1.09–1.38);
p = 0.0008), despite the less frequent cardiotoxicity events
[78][79][96,97]. A 6-month duration of trastuzumab reflected an increased absolute DFS risk by almost 4% at 5 years
[80][98].
Despite the many attempts to achieve comparable outcomes by abbreviating or stretching the course of trastuzumab, the 1-year duration remains the optimal time for which trastuzumab should be delivered in the adjuvant setting.
11. Multigene Profiling Assays
The genomic expression assays (GEAs) help in tailoring optimal treatment whilst also helping to avoid unnecessary chemotherapy in women with BC ER+ HER2−
[81][99]. By means of generating predictive risk scores, GEAs identify patients in whom adjuvant chemotherapy can be advantageous
[81][82][99,100].
Given similar scores among BC tissue samples from biopsy and surgical specimens, the St. Gallen International Consensus Guidelines endorsed the use of GEAs to optimize neoadjuvant treatment strategies from biopsied samples, which has helped contribute to a practice change
[83][84][101,102].
For patients with HER2+ BC disease, the novel HER2DX is a prognostic and predictive GEA encompassing 27 gene expression levels including ErbB2 mRNA, which, in combination with clinical and tumor features, identifies four gene signature profiles (immune, proliferation, luminal differentiation, and HER2 amplicon)
[85][103]. The HER2DX is a validated gene profiling assay that can estimate the BC recurrence risk and NAC tumor response, quantifying the likelihood in achieving pCR
[86][104]. The HER2DX can be helpful by determining in whom the escalation or de-escalation of chemotherapy is the most favorable strategy
[18][85][18,103].
12. Tumor-Infiltrating Lymphocytes
Antitumor immune response can lead to the recruitment and formation of well-organized clusters of T-lymphocytes (mainly, CD4+T and CD8+T), B-lymphocytes, as well as natural-killer (NK) cells. In other words, TILs are such lymphocytic cells that move towards, and surround, the microenvironment of tumor cells
[87][88][105,106]. Quantifying the volume of TILs embodying the breast tumor is essential in determining TIL levels
[89][90][107,108]. The greater the TIL index, the higher the ratio between CD8+ and CD4+ T cells, implying an enhanced cytotoxic T-cell reaction
[91][109]. In these cases, a high number of TILs has been associated with a better NAC response and improved outcomes in HER2+ and TNBC, in addition to being a reliable histologic predictor in determining HER2 positivity when IHC results are equivocal (score 2+)
[89][92][93][107,110,111].
A recent meta-analysis included 29 published trials and 9145 participants with BC treated with NAC. In this pooled-analysis, a high number of TILs were demonstrated to be predictive of pCR (OR 2.54 (95% CI, 1.50–4.29)) and prognostic for OS (HR 0.93 (95% CI, 0.87–0.99)) and DFS (HR 0.96 (95% CI, 0.94–0.98)) in HER2+ patients. However, no association was found in ER+ BC patients
[94][112]. In another study, the secondary analysis of the NeoALTTO trial, which included patients treated with neoadjuvant lapatinib and trastuzumab, demonstrated that for each 1% increase in the level of TILs, there was a 3% decrease in the BC relapse event rate
[95][113].
TIF can also be predictive of a better efficacy of immune checkpoint inhibitors (ICIs) in BC patients
[96][114]. Together with TILs, the programmed death-1 (PD-1) ligand-1 (PD-L1), as immune biomarkers, can identify tumors that are sensitive to immunotherapy, helping clinicians to select potentially successful candidates to be treated with ICIs
[92][110].
13. Immune Checkpoint Inhibitors
By blocking signaling transduction on HER2-enriched cells with targeted HER2 blockers, an immune-mediated response is triggered. Thus, HER2 blockers can be interpreted through the lens of an immunotherapeutic strategy
[97][115]. Emerging data have demonstrated potential synergism in promoting antitumor immunity between HER2 therapies and cytotoxic T lymphocyte-associated antigen 4 (CTLA4) or PD-1/PD-L1 inhibitors in BC patients
[98][99][116,117]. In the metastatic setting, the PANACEA trial showed a durable clinical benefit of pembrolizumab with trastuzumab in heavily treated HER2+ BC patients with PD-L1+ tumors
[100][118]. On the other hand, the KATE2 study did not show an advantage of adding atezolizumab to T-DM1 in previously treated advanced HER2+ BC
[101][119].
The phase III IMpassion050 trial recruited high-risk (T2–4; N1–3) early HER2+ BC patients. Participants were randomized to receive atezolizumab/placebo with standard anthracycline-taxane based NAC with H+P. After surgery, trial candidates continued H+P and atezolizumab/placebo until a 1-year completion of the mABs against the HER2. This study showed that those with PD-L1-positive tumors had higher pCR rates versus those with PD-L1-negative tumors. No substantial difference in pCR rates was noted when atezolizumab was added to standard chemotherapy
[102][120].
To date, TNBC has been the only subtype among all BC phenotypes to show a substantial benefit from being exposed to the combination NAC and ICI, leading to a practice change
[103][104][121,122]. Ongoing trials continue to explore a potential role for checkpoint inhibitors in the management of early HER2+ BC. The ASTEFANIA trial is evaluating adjuvant atezolizumab/placebo in combination with T-DM1 in patients with pRD after surgery
[105][123]. The APTneo is investigating NAC with atezolizumab with H+P in BC patients with high-risk features
[106][124]. The NeoHIP is a neoadjuvant trial accruing candidates with a high risk for BC relapse, comprising weekly paclitaxel, with H+P with versus without pembrolizumab. After surgery, the selection of systemic treatment is in accordance with their treating physician’s discretion
[107][125].
 Encyclopedia
Encyclopedia
