Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Jason Zhu and Version 1 by Filippo Maselli.
Direct access in physiotherapy (DAPT) occurs when a patient has the ability to self-refer to physical therapy without physician referral. This model of care in musculoskeletal diseases (MSDs) has shown better outcomes than the traditional-based medical model of care that requires physician referral to access physiotherapist services. This traditional physician referral often results in a delay in care. Unfortunately, DAPT is still not permitted in many countries.
- direct access
- physical therapy
- self-referral
- primary care
1. Introduction
Musculoskeletal disorders (MSDs) are injuries or disorders affecting the body movement or the musculoskeletal system [1]. MSDs are the second most common cause of disability worldwide [2], with a prevalence comparable to the sum of all cardiovascular and chronic respiratory diseases. MSDs resulted in an economic burden of more than USD 800 billion (US) in 2015 [3]. Due to the significant impact of MSDs, it is essential to consider value-based care and work towards examining new approaches to manage MSDs more efficiently. Direct access to physiotherapy (DAPT) occurs when a patient can self-refer to a physiotherapist without having to see another health professional for a medical prescription [4]. Preliminary evidence suggests that DAPT could offer a promising option compared to other traditional models of care, particularly the physician-led model of care [5,6,7,8,9][5][6][7][8][9]. The effectiveness of DAPT has been reported by authors in several areas: reduction in direct and indirect costs for the patient and the national health system [6], reduction in work overload for general practitioners (GPs) [7], and improvement in health indicators for patients (e.g., health-related quality of life, quality-adjusted life years) [9]. World Physiotherapy itself, a global organization that represents the profession of physiotherapists at an international level, advocates for the growing responsibilities of the profession. This phase shift for the profession of physiotherapy is why clarifying the efficacy and safety of DAPT for patients with musculoskeletal disorders is needed [4,10,11,12,13,14][4][10][11][12][13][14].
2. Population
A total of 32,742 patients underwent assessment and management through the DAPT care model, while 9900 patients underwent assessment and management through the physician-led care model, with a total number of 42,642 patients. Characteristics of the population are summarized in Table 31. Age, sex, and gender were not available for four studies [19,27,31,48][15][16][17][18]; seven studies did not provide additional details regarding the type and location of musculoskeletal disorder [19,27[15][16][17][19][20][21][22],28,31,32,36,43], while seventeen studies did not specify pathology onset [9,18,19,26,27,28,29,31,32,36,37,38,39,40,41,45,48][9][15][16][17][18][19][20][21][23][24][25][26][27][28][29][30][31].Table 31.
Population characteristics investigated in the current study.
| Age (mean) | 49 Years |
| Sex (%) | 57% F–43% M |
| Type of MSDs (%) | Upper Limb 15% Spine 50% Lower Limb 25% Widespread/Mixed Pain 7% Rheumatological Disease 3% |
| Onset (%) | Acute (<6 weeks) 40% Sub-acute (6 weeks to 3 months) 25% Chronic (>3 months) 35% |
Table 42.
Type of specialization of the involved physiotherapists in DAPT.
| Type of Specialization | Nr. of Studies |
|---|---|
| Post-graduate specialization/ doctorate or musculoskeletal certification | 2 studies |
| 1 day out for training; direct access to primary care and mentoring | 1 study |
| From 6 to 28 years of experience | 5 studies |
| At least 3 years of experience in primary care + at least 1 orthopedic manipulative physiotherapist specialization | 4 studies |
| Extended or advanced scope practitioner | 11 studies |
| Degree of physiotherapy | 2 studies |
| Specialization not specified | 3 studies |
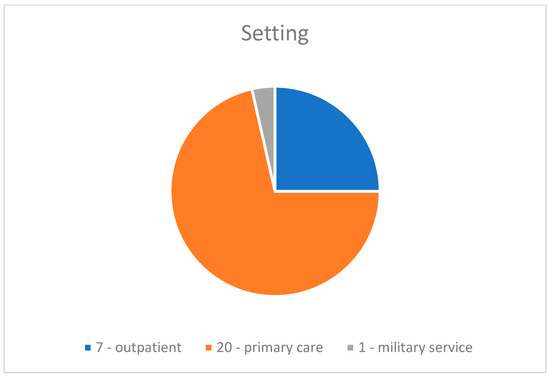
Figure 21.
Setting of care.
3. DAPT Management Accuracy
Fourteen studies evaluated the triage proficiency of physiotherapists [16,18,19,26,29,31,33,36,40,41,42,46,47,49][15][17][21][23][24][25][29][30][33][34][37][40][41][42]. Most commonly, physiotherapists triage patients without additional medical consultation [16,18,19,26,31,36,40,41,42,46,47][15][17][21][23][24][29][30][33][34][37][41]. Three studies compared the surgical conversion rate expressed as a percentage (i.e., surgical conversion rate is considered a useful measure of appropriateness of referrals, as it is a measure of the percentage of patients that were referred to a physician and underwent surgery) [19,40,41][15][29][30]. Referral selection accuracy was used as a measure of management accuracy only in one study [33][40]. The rate of return to visit or rate of re-referral was evaluated in four studies [29,31,33,47][17][25][37][40]. The agreement between physiotherapy and medical evaluation was evaluated in three studies [18,31,49][17][23][42]. Management accuracy is summarized in Table 53, resulting in secondary care referral accuracy (15% average difference) in favor of DAPT.Table 53.
DAPT management accuracy.
| Parameter | Range | Mean |
|---|---|---|
| Patients independently screened by physiotherapist | 69–97 | 80.6% |
| Surgical conversion rate | 40–89.3% | 67.4% |
4. Cost-Effectiveness
Sixteen studies evaluated cost-effectiveness between models using different outcomes [7,9,27,28,31,33,34,35,36,37,42,43,44,45,47,48][7][9][16][17][18][19][21][22][26][31][32][35][36][37][40][41]:- -
-
Use of health system resources, calculating the intervention costs: medication use and number of imaging referrals [9,27,31,33,34,35,37,42,45,46,47,48][9][16][17][18][26][31][32][34][35][37][40][41];
- -
-
Cost sustained by the patient [27,34,46][16][32][34];
- -
-
Patient savings [36,48][18][21];
- -
-
Incremental Cost Effectiveness Ratio (ICER) [9,43,45][9][22][31];
- -
-
Benefits estimated by the Quality-Adjusted Life Years (QALYs) [9,34,43,45][9][22][31][32];
- -
-
Time needed to deliver the triage process [28][19];
- -
-
Waiting time rate per visit [32,34][20][32];
- -
-
Timeframe before discharge [28][19];
- -
-
Number of visits needed for discharge [44][36].Table 64.Type of treatment prescribed.
][9][35]. A summary of compared wage costs and treatment options [42,45][31][41] are reported in Table 75.DAPT Mean
(Min–Max)Medical Model Mean
(Min–Max)Mean Difference Imaging 21% (0–63%) 49% (27–86%) 28% DAPT resulted in EUR 39.370 and EUR 62.867 of savings [9,27,35][9][16][35] in a timeframe ranging from 6 months [27][16] to 1 year [9,35Table 75.Comparison between wage costs and treatment options and QALYs.DAPT Mean (Min–Max) Medical Model Mean (Min–Max) Mean Difference Cost for episode of care EUR 301.5 (255.55–628.24) Medication 22.3% (8–50%) 63.5% (60–73.1%) 41.2% Referral 9.3% (2.9–19.3%) 30% (14–40%) 20.7% ICER, or the incremental cost-effectiveness ratio, is a synthetic measure that represents the economic value of an intervention, compared with an alternative intervention. Three studies have shown the ICER to be smaller for DAPT, meaning that physiotherapist-led management is less expensive and more effective than a physician-led model of care [9,43,45][9][22][31]. Two studies did not find statistically significant differences for direct costs sustained by the patient between care models [34[32][34],46], while another study estimated a favorable cost for the patient who carries out DAPT equal to EUR 29.5 per visit compared to the medical model which had an expense of EUR 63.8, for a total cost saving to the patient equal to EUR 34.3 in favor of DAPT [27][16]. Two studies estimated between USD 36.42 and USD 129 saved per patient per episode of care in favor of DAPT [36[18][21],48], with an average of USD 82.71 saved favoring DAPT. Mallett et al. also calculated an amount of £84,387.80 and £124,472.06 as the projection of the total savings over a year for a physiotherapist-led service, towards a general practitioner (GP)-led pathway, initiated by telephone contact from the patient, followed by a subsequent telephone triage appointment with a physiotherapist [36][21]. Notably, the DAPT pathway ensures an increase of 0.07 and 0.047 (average 0.05) of QALYs [9,34,43,45][9][22][31][32]. Although not statistically significant, Bornhöft et al. agree that DAPT has the potential to be a better cost-effective option (9). Regarding the rate of presence to visit (i.e., the effective presence to visit of a patient after a phone scheduled appointment) results [34,36][21][32] are summarized in Table 86.Table 86.Rate of presence to visit.
Interestingly, the lack of missed appointments due to patient no-show would allow the health system to save between £84,387.80 and £124,472.06 in one year [36][21]. As for the outcome of total time needed to triage and to discharge the patient, results are summarized in Table 97.DAPT Mean
(Min–Max)Medical Model Mean
(Min–Max)Mean Difference Presence to visit 93.5% (90–97.1%) 87.5% (86–89%) 6% The impact of DAPT on patient’s ability to work was evaluated in 10 studies [9,17,32,34,37,39,43,45,46,48][9][18][20][22][26][28][31][32][34][38] which focused on:Table 97. Time to triage/discharge the patient.DAPT Mean Medical Model Mean Mean
DifferenceTime to triage in minutes 108 min 148 min 40 min Percentage of patients discharged within 4 h in primary care 93% 75% 18% Number of sessions/days to discharge
(Ankle MSDs)5.6 sessions/
no difference6.7 sessions/
no difference1.1 sessions Number of sessions/days to discharge
(Knee MSDs)6.3 sessions/
49.7 days9.1 sessions/
60.2 days2.8 sessions/
10.5 days5. Work Related Outcomes
- -
-
Self-administered questionnaire on patients’ work productivity [46][34] or questionnaire intended to measure self-efficacy in the workplace [43][22];
- -
-
Percentage of patients prescribed sick days [37,45][26][31];
- -
-
Number of sick days [9,17,45,48][9][18][31][38];
- -
-
Labor participation measured on a 3-point scale (1 = did not return to work; 2 = returned to work with adaptations; or 3 = returned to work without adaptations) [39][28];
- -
-
Time off work directly reported by the patients [32,34][20][32] or the amount of sick hour leaves [9].Table 108.Percentage of sick leave prescriptions and number of sick leave days.
DAPT Mean (Min–Max) Medical Model Mean (Min–Max) Mean Difference Percentage of sick leave prescriptions 9% (3–15.1%) 12.16% (7.3–23.5%) 5% Number of sick leave days prescribed 13.5 days (0–27 days) 50.5 days (26–75 days) 37 days 6. Patient Satisfaction
Ten studies evaluated the patient, using:- -
-
A 10- and 7-point Likert scale [7,42][7][41];
- -
-
Satisfaction questionnaires [16,18,27,31,33,36,47][16][17][21][23][33][37][40];
- -
-
Qualitative surveys [34][32].
- -
-
A questionnaire related to the satisfaction in care received [47][37];
- -
-
A modified and adapted questionnaire for assessing the quality of direct remote-access care (telephone) [36][21];
- -
-
The Quality from the Patient’s Perspective Questionnaire (QPP) [33][40];
- -
-
A patient satisfaction questionnaire and a physician satisfaction questionnaire related to how the physiotherapist performed the triage [18][23];
- -
-
The Perceived Improvement Evaluation (PIVAS) questionnaire [50][43] and the Deyo and Diehl (DD) [51][44] questionnaire [16][33];
- -
-
A questionnaire on patients’ experience of care [31][17];
- -
-
A questionnaire on patient satisfaction/dissatisfaction with being referred to another professional or additional diagnostic investigations (e.g., X-ray) [27][16].
- -
-
patient dissatisfaction with staff communication;
- -
-
patient dissatisfaction with the quality of treatment received;
- -
-
patient dissatisfaction with the facilities.
7. DAPT Safety
Five studies [27,32,34,38,46][16][20][27][32][34] investigated DAPT safety by the number of adverse events (i.e., unexpected events that occur following an intervention without evidence of causality). As an example, an increase in pain after a physiotherapist intervention occurred. Only one study reported the occurred severity of the adverse events that occurred by categorizing the event as none, mild, moderate, or severe [46][34]. DAPT safety is reported in Table 119.Table 119.DAPT safety.Authors Evaluation of DAPT Safety Results Peterson et al., 2021 [27][16] Number of adverse events none Bishop et al., 2017 [32][20] Number of adverse events none Salisbury et al., 2013 [34][32] Number of adverse events none Bornhöft et al., 2019 [38][27] Number of adverse events none Ojha et al., 2020 [46][34] Number and type of adverse events 4 mild adverse events:
2/77 DAPT group
2/73 medical group
Two patients in the medical group had an accidental fall at home, and unclear diagnosis of ankle pain at one-year and two patients in the DAPT group had side effects from an emergency room medication, and unclear diagnosis of low back pain.8. Health Outcomes
Health outcomes were investigated in 15 studies [16,17,28,32,34,35,36,38,39,42,43,45,46,47,48][18][19][20][21][22][27][28][31][32][33][34][35][37][38][41].- -
-
Six studies [28,32,33,34,36,48][18][19][20][21][32][40] estimated waiting time for assessment/management of DAPT toward a physician-led model of care, of which five were estimated in days [32,33,34,36,48][18][20][21][32][40] and one was estimated in minutes [28][19]. Results of DAPT waiting times are summarized in Table 120;
-
Table 120.DAPT waiting times.
DAPT Mean (Min–Max) Physician-Led Care Model Mean (Min–Max) Mean Difference Waiting times in days 12.31 (3.55–26 days) 35.59 (28–57 days) 23.28 days Primary care waiting time (min) n.a. n.a. 31 min
- -
-
Three studies evaluated health outcomes using district-specific questionnaires [39,42[22][28][41],43], but there was a large heterogeneity of questionnaires used between studies;
- -
-
Quality of life was assessed in 13 studies. The most-often used tool was the EuroQoL (EQ5D) [16[21][22][27][31][32][33][37][38][41],17,34,36,38,42,43,45,47], followed by the Short Form Health Survey 36 (SF-36) [16[33][41],42], SF-12 [43][22], and SF-10 [46][34];
- -
-
Perception of disability was evaluated in four studies through the Pain Disability Index (PDI) [17][38], the Disease Repercussions Profile [42][41], or the Measure Yourself Medical Outcomes Profile and global improvement [34][32]. Koojiman et al. [35] analyzed and compared the percentage of patients who achieved the expected outcomes between patients who underwent DAPT and those who went to the physiotherapist following medical referral;
- -
-
One study [38][27] assessed functional disability in ADLs with the Disability Rating Index (DRI) and the patient’s attitudes towards their musculoskeletal disorder through the Attitude Responsibility for Musculoskeletal disorders scale (ARM);
- -
-
Oostendorp et al. [39][28] evaluated the patient’s coping through the Pain Coping Inventory (PCI) and general health with the Global Perceived Effect (GPE);
- -
-
Two studies [38,42][27][41] assessed psychological health (35,39) through the Hospital Anxiety and Depression Scale;
- -
-
Five studies measured pain, three using the VAS (Visual Analogic Scale) [16[28][33][41],39,42], one the Numeric Pain Rating Scale (NPRS) [38][27], and another the 10-point Likert scale [46][34];
- -
-
Risk of chronicity of musculoskeletal pathology was carried out by two studies [38,43][22][27] through the Örebro Musculoskeletal Pain Screening Questionnaire (ÖMPSQ);
- -
-
Pain-related catastrophization of the patient was assessed by two studies [43,46][22][34] using the Pain Catastrophizing Scale (PCS);
- -
-
Two studies [39,43][22][28] evaluated avoidance behavior using the Fear Avoidance Belief Questionnaire (FABQ);
- -
-
Two studies [42,46][34][41] used the Pain Self Efficacy Questionnaire (PSEQ) to assess patient self-efficacy;
- -
-
One study [46][34] used the Patient-Specific Functional-Scale (PSFS) for physical function and the Patient Acceptability Symptom State (PASS) to measure acceptability of symptoms.
9. Risk of Bias Assessment
Overall, three studies were judged as demonstrating “low risk of bias” [32[20][31][34],45,46], six studies were rated as “some concern” [17[27][32][38][40][41],33,34,38,42], and one as “high risk” [30][39]. The Quality of RCT methodological evidence is summarized in Figure 32.Even if the NOS scale does not allow for the estimation of a final score, each star was considered as a point to generate a score. Table 131 and Table 142 summarizes the NOS evaluation. For observational studies with a control group [18[18][19][21][22][23][26][35][36][37],28,35,36,37,43,44,47,48], the mean score was 6/9 points, with a minimum score of 4 and a maximum score of 9 points, while for observational studies without a control group [19,26,27,29,31,40,41,48][15][16][17][18][24][25][29][30] a mean score of 4.75/9 was reported.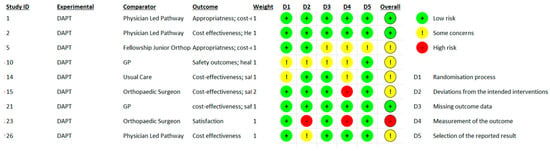 Figure 32.Rob-2 Score evaluation.Table 113.Newcastle Ottawa Scale evaluation for case-control studies.
Figure 32.Rob-2 Score evaluation.Table 113.Newcastle Ottawa Scale evaluation for case-control studies.Reference Selection of Case and Controls Comparability of Cases
and ControlsExposure Total ITEM#1
Is the case definition adequateITEM#2
Representativeness of the casesITEM#3
Selection of ControlsITEM#4
Definition of Controls
Not Present at StartITEM#5
Comparability of cases and controls on the basis of the
design or analysisITEM#6
Ascertainment of exposureITEM#7
Same method of ascertainment for cases and controlsITEM#8
Non-Response RateBird et al., 2016 [28][19] ✸ ✸ ✸ ✸ ✸ ✸ ✸ 8/9 Bornhöft et al., 2015 [37][26] ✸ ✸ ✸ ✸ 5/9 Kooijman et al., 2013 [35] ✸ ✸ ✸ ✸ ✸ ✸ 6/9 Lankhorst et al., 2017 [44][36] ✸ ✸ ✸ ✸ ✸ ✸ ✸ 7/9 Ludvigsson et al., 2012 [47][37] ✸ ✸ ✸ ✸ ✸ ✸ ✸ 7/9 Mallet et al., 2014 [36][21] ✸ ✸ ✸ ✸ ✸ ✸ ✸ 7/9 Oldmeadow et al., 2007 [18][23] ✸ ✸ ✸ ✸ ✸ ✸ ✸ 7/9 Phillips et al., 2012 [43][22] ✸ ✸ ✸ ✸ 4/9 Szymanek et al., 2022 [48][18] ✸ ✸ ✸ ✸ ✸ ✸ ✸ ✸ 8/9 Table 142.Newcastle Ottawa Scale evaluation for cohort studies.Reference Selection of Cohorts Comparability of Cohorts Outcome Total ITEM#1
Representativeness of the Exposed CohortITEM#2
Selection of the Non-ExposedITEM#3
Ascertainment of ExposureITEM#4
Demonstration that outcome of interest was not present at
start of studyITEM#5
Comparability of cohorts on the basis of the design or analysisITEM#6
Assessment of OutcomeITEM#7
Was follow up long enough for outcomes to occurITEM#8
Adequacy of Follow Up of CohortsCaffrey et al., 2019 [26][24] ✸ ✸ ✸ ✸ ✸ 5/9 Chang et al., 2018 [29][25] ✸ ✸ ✸ ✸ 4/9 Downie et al., 2019 [31][17] ✸ ✸ ✸ ✸ ✸ 5/9 Kerridge-Weeks et al., 2016 [41][30] ✸ ✸ ✸ ✸ ✸ ✸ 6/9 Lyons et al., 2022 [19][15] ✸ ✸ ✸ ✸ ✸ 4/9 O’Farrell et al., 2014 [40][29] ✸ ✸ ✸ ✸ ✸ 5/9 Peterson et al., 2021 [27][16] ✸ ✸ ✸ ✸ ✸ 5/9 Szymanek et al., 2022 [48][18] ✸ ✸ ✸ ✸ 4/9
-
References
- National Academies of Sciences, Engineering, and Medicine. Musculoskeletal Disorders. In Selected Health Conditions and Likelihood of Improvement with Treatment; The National Academic Press: Washington, DC, USA, 2020.
- Briggs, A.M.; Woolf, A.D.; Dreinhöfer, K.; Homb, N.; Hoy, D.G.; Kopansky-Giles, D.; Åkesson, K.; March, L. Reducing the Global Burden of Musculoskeletal Conditions. Bull. World Health Organ. 2018, 96, 366–368.
- The Burden of Musculoskeletal Diseases in the United States|Prevalence, Societal and Economic Cost. Available online: https://www.boneandjointburden.org/ (accessed on 12 December 2022).
- APTA APTA Direct Access Advocacy. Available online: https://www.apta.org/advocacy/issues/direct-access-advocacy (accessed on 19 March 2022).
- Hon, S.; Ritter, R.; Allen, D.D. Cost-Effectiveness and Outcomes of Direct Access to Physical Therapy for Musculoskeletal Disorders Compared to Physician-First Access in the United States: Systematic Review and Meta-Analysis. Phys. Ther. 2021, 101, pzaa201.
- Demont, A.; Bourmaud, A.; Kechichian, A.; Desmeules, F. The impact of direct access physiotherapy compared to primary care physician led usual care for patients with musculoskeletal disorders: A systematic review of the literature. Disabil. Rehabil. 2021, 43, 1637–1648.
- Ojha, H.A.; Snyder, R.S.; Davenport, T.E. Direct access compared with referred physical therapy episodes of care: A systematic review. Phys. Ther. 2014, 94, 14–30.
- Samsson, K.S.; Grimmer, K.; Larsson, M.E.H.; Morris, J.; Bernhardsson, S. Effects on health and process outcomes of physiotherapist-led orthopaedic triage for patients with musculoskeletal disorders: A systematic review of comparative studies. BMC Musculoskelet. Disord. 2020, 21, 673.
- Bornhöft, L.; Thorn, J.; Svensson, M.; Nordeman, L.; Eggertsen, R.; Larsson, M.E.H. More cost-effective management of patients with musculoskeletal disorders in primary care after direct triaging to physiotherapists for initial assessment compared to initial general practitioner assessment. BMC Musculoskelet. Disord. 2019, 20, 186.
- Gazzetta Ufficiale Law n 25/2018. Available online: https://www.gazzettaufficiale.it/eli/id/2018/1/31/18G00019/sg (accessed on 26 September 2022).
- Gazzetta Ufficiale Law n 64/2017. Available online: https://www.gazzettaufficiale.it/eli/id/2017/03/17/17G00041/sg (accessed on 18 September 2022).
- Abbafati, C.; Abbas, K.M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abdelalim, A.; Abdollahi, M.; Abdollahpour, I.; Abegaz, K.H.; Abolhassani, H.; Aboyans, V.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222.
- Advocacy|World Physiotherapy. Available online: https://world.physio/what-we-do/advocacy (accessed on 18 September 2022).
- Maselli, F.; Piano, L.; Cecchetto, S.; Storari, L.; Rossettini, G.; Mourad, F. Direct Access to Physical Therapy: Should Italy Move Forward? Int. J. Environ. Res. Public Health 2022, 19, 555.
- Lyons, R.F.; Cassells, M.; Hynes, D.; Mullett, H.; Groarke, P.J. A physiotherapy triage service for orthopaedic upper limb service: An effective way to reduce clinic visits and identify patients for operative intervention. Ir. J. Med. Sci. 2022, 191, 771–775.
- Peterson, G.; Portström, M.; Frick, J. Extended roles in primary care when physiotherapist-initiated referral to X-ray can save time and reduce costs. Int. J. Qual. Heal. Care 2021, 33, mzab122.
- Downie, F.; McRitchie, C.; Monteith, W.; Turner, H. Physiotherapist as an Alternative to a GP for Musculoskeletal Conditions. Br. J. Gen. Pract. 2019, 69, e314–e320.
- Szymanek, E.; Jones, M.; Shutt-Hoblet, C.; Halle, R. Implementation of Direct Access Physical Therapy Within the Military Medical System. Mil. Med. 2022, 187, e649–e654.
- Bird, S.; Thompson, C.; Williams, K.E. Primary contact physiotherapy services reduce waiting and treatment times for patients presenting with musculoskeletal conditions in Australian emergency departments: An observational study. J. Physiother. 2016, 62, 209–214.
- Bishop, A.; Ogollah, R.O.; Jowett, S.; Kigozi, J.; Tooth, S.; Protheroe, J.; Hay, E.M.; Salisbury, C.; Foster, N.E. STEMS pilot trial: A pilot cluster randomised controlled trial to investigate the addition of patient direct access to physiotherapy to usual GP-led primary care for adults with musculoskeletal pain. BMJ Open 2017, 7, e012987.
- Mallett, R.; Bakker, E.; Burton, M. Is Physiotherapy Self-Referral with Telephone Triage Viable, Cost-effective and Beneficial to Musculoskeletal Outpatients in a Primary Care Setting? Musculoskelet. Care 2014, 12, 251–260.
- Phillips, C.J.; Phillips, R.; Main, C.J.; Watson, P.J.; Davies, S.; Farr, A.; Harper, C.; Noble, G.; Aylward, M.; Packman, J.; et al. The cost effectiveness of NHS physiotherapy support for occupational health (OH) services. BMC Musculoskelet. Disord. 2012, 13, 29.
- Oldmeadow, L.B.; Bedi, H.S.; Burch, H.T.; Smith, J.S.; Leahy, E.S.; Goldwasser, M. Experienced physiotherapists as gatekeepers to hospital orthopaedic outpatient care. Med. J. Aust. 2007, 186, 625–628.
- Caffrey, A.; Smart, K.M.; FitzGerald, O. Physiotherapist-Led Triage at a Rheumatology-Based Musculoskeletal Assessment Clinic: An 18-Month Service Evaluation of Activity and Outcomes. ACR Open Rheumatol. 2019, 1, 213–218.
- Chang, A.T.; Gavaghan, B.; O’Leary, S.; McBride, L.-J.; Raymer, M. Do patients discharged from advanced practice physiotherapy-led clinics re-present to specialist medical services? Aust. Health Rev. 2018, 42, 334–339.
- Bornhöft, L.; Larsson, M.E.H.; Thorn, J. Physiotherapy in Primary Care Triage—The effects on utilization of medical services at primary health care clinics by patients and sub-groups of patients with musculoskeletal disorders: A case-control study. Physiother. Theory Pract. 2015, 31, 45–52.
- Bornhöft, L.; Larsson, M.E.; Nordeman, L.; Eggertsen, R.; Thorn, J. Health effects of direct triaging to physiotherapists in primary care for patients with musculoskeletal disorders: A pragmatic randomized controlled trial. Ther. Adv. Musculoskelet. Dis. 2019, 11, 1759720X19827504.
- AB Oostendorp, R.; Elvers, J.H.; van Trijffel, E.; Rutten, G.M.; Scholten-Peeters, G.G.; Heijmans, M.; Hendriks, E.; Mikolajewska, E.; De Kooning, M.; Laekeman, M.; et al. Clinical Characteristics and Patient-Reported Outcomes of Primary Care Physiotherapy in Patients with Whiplash-Associated Disorders: A Longitudinal Observational Study. Patient Prefer. Adherence 2020, 14, 1733–1750.
- O’farrell, S.; Smart, K.M.; Caffrey, A.; Daly, O.; Doody, C. Orthopaedic triage at a physiotherapist-led ‘Musculoskeletal Assessment Clinic’: A seven-month service evaluation of outcomes. Ir. J. Med Sci. 2014, 183, 565–571.
- Kerridge-Weeks, M.; Langridge, N.J. Orthopaedic Spinal Triage: An Evaluation of Decision Making and Outcome in a Physiotherapy Led Service. Int. J. Health Gov. 2016, 21, 5–17.
- Ho-Henriksson, C.-M.; Svensson, M.; Thorstensson, C.A.; Nordeman, L. Physiotherapist or physician as primary assessor for patients with suspected knee osteoarthritis in primary care—A cost-effectiveness analysis of a pragmatic trial. BMC Musculoskelet. Disord. 2022, 23, 260.
- Salisbury, C.; Foster, N.; Hopper, C.; Bishop, A.; Hollinghurst, S.; Coast, J.; Kaur, S.; Pearson, J.; Franchini, A.; Hall, J.; et al. A pragmatic randomised controlled trial of the effectiveness and cost-effectiveness of ‘PhysioDirect’ telephone assessment and advice services for physiotherapy. Health Technol. Assess. 2013, 17, 1–157.
- Sephton, R.; Hough, E.; Roberts, S.A.; Oldham, J. Evaluation of a primary care musculoskeletal clinical assessment service: A preliminary study. Physiotherapy 2010, 96, 296–302.
- Ojha, H.A.; Fritz, J.M.; Malitsky, A.L.; Wu, J.; Weiner, M.G.; Brandi, J.A.; Rhon, D.I.; Mobo, B.H.P.; Fleming, K.M.; Beidleman, R.R.; et al. Comparison of Physical Therapy and Physician Pathways for Employees with Recent Onset Musculoskeletal Pain: A Randomized Controlled Trial. PM&R 2020, 12, 1071–1080.
- Kooijman, M.; Swinkels, I.; van Dijk, C.; de Bakker, D.; Veenhof, C. Patients with shoulder syndromes in general and physiotherapy practice: An observational study. BMC Musculoskelet. Disord. 2013, 14, 128.
- Lankhorst, N.; Barten, J.; Meerhof, R.; Bierma-Zeinstra, S.; van Middelkoop, M. Characteristics of patients with knee and ankle symptoms accessing physiotherapy: Self-referral vs general practitioner’s referral. Physiotherapy 2020, 108, 112–119.
- Ludvigsson, M.L.; Enthoven, P. Evaluation of physiotherapists as primary assessors of patients with musculoskeletal disorders seeking primary health care. Physiotherapy 2012, 98, 131–137.
- Samsson, K.S.; Larsson, M.E. Physiotherapy triage assessment of patients referred for orthopaedic consultation—Long-term follow-up of health-related quality of life, pain-related disability and sick leave. Man. Ther. 2015, 20, 38–45.
- Samsson, K.S.; Bernhardsson, S.; Larsson, M.E.H. Perceived quality of physiotherapist-led orthopaedic triage compared with standard practice in primary care: A randomised controlled trial. BMC Musculoskelet. Disord. 2016, 17, 257.
- Samsson, K.; Larsson, M.E. Physiotherapy screening of patients referred for orthopaedic consultation in primary healthcare—A randomised controlled trial. Man. Ther. 2014, 19, 386–391.
- Daker-White, G.; Carr, A.J.; Harvey, I.; Woolhead, G.; Bannister, G.; Nelson, I.; Kammerling, M. A randomised controlled trial. Shifting boundaries of doctors and physiotherapists in orthopaedic outpatient departments. J. Epidemiol. Community Health 1999, 53, 643–650.
- Peterson, S. Telerehabilitation booster sessions and remote patient monitoring in the management of chronic low back pain: A case series. Physiother. Theory Pract. 2018, 34, 393–402.
- Kremer, E.; Atkinson, H.J.; Ignelzi, R.J. Measurement of pain: Patient preference does not confound pain measurement. Pain 1981, 10, 241–248.
- Deyo, R.A.; Diehl, A.K. Patient Satisfaction with Medical Care for Low-Back Pain. Spine 1986, 11, 28–30.
More
