Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Kuo-Hu Chen and Version 2 by Camila Xu.
Preeclampsia is a systemic disorder that may present with various symptoms and signs. The manifestation of preeclampsia is widely perceived to be centered around hypertension and proteinuria, but clinical presentations could be variable in essence.
- preeclampsia
- gestational hypertension
- pregnancy induced hypertension
- proteinuria
1. Introduction
Preeclampsia is a systemic disorder that may present with various symptoms and signs. The manifestation of preeclampsia is widely perceived to be centered around hypertension and proteinuria, but clinical presentations could be variable in essence. Different organs and systems could all be influenced by preeclampsia. Systemic manifestations of preeclampsia are shown in Figure 1.
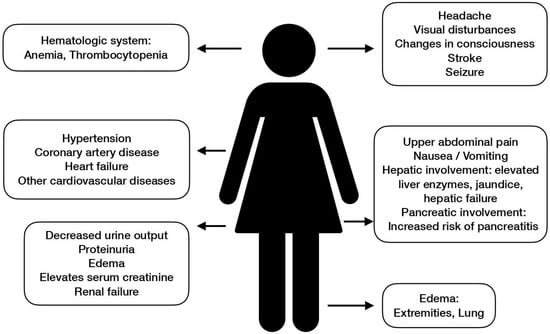
Figure 1.
Systemic manifestations of preeclampsia.
According to the two-stage theory, preeclampsia proceeds into the clinical stage once the systemic vascular response and inflammation have taken place as a result of endothelial dysfunction. This aptly explains why preeclampsia is a global syndrome as the endothelium is distributed all over the body. The most famous affected organs and systems include the central nervous system, cardiovascular system, liver, and kidney.
2. Central Nervous System (CNS)
The brain is a vital organ that requires approximately 20% of available oxygen to maintain normal function. In most physiological conditions, cerebral blood flow (CBF) has sufficient capability to autoregulate and remains rather stable to cope with its high metabolic demand. However, once brain injury to a certain extent occurs, sequelae including acute severe hypertension, the loss of myogenic tone of the vascular smooth muscle, and uncontrolled vasoconstriction may lead to the failure of autoregulation. As they key to the delicate homeostasis of the brain environment, both hypoperfusion and hyperperfusion may break the balance and bring great harm. Insufficient CBF could lead to ischemic brain injury and ischemic stroke. Hyperperfusion, on the other hand, may disrupt the blood–brain barrier (BBB) and cause edema formation, which is one of the classic findings in preeclamptic and eclamptic patients [1][2][49,50].
CBF could be assessed in patients with preeclampsia via transcranial Doppler imaging. The middle cerebral artery is often chosen to be the target of examinations. Perhaps somewhat surprisingly, the cerebral flow index (CFI) appears to be normal in most women with preeclampsia. However, cerebral perfusion pressure (CPP) exhibits greater elevation in preeclamptic women and may serve as the key to brain injury among these women [3][51]. Brain damage has been demonstrated in autopsies and image studies [4][52]. It has been proven in some studies that elevated CPP corresponds to hypertension, and antihypertensive treatment that decreases CPP lowers the rate of cerebral complications in these patients [5][53].
CNS manifestations that are suggestive of severe disease status are headaches, visual disturbances, changes in consciousness, and seizures. The spectrum is coined “preeclamptic encephalopathy” [5][53]. Once a seizure takes place, the impression of eclampsia is almost certain after the exclusion of other previously known neurological conditions that may also lead to convulsion events. Eclampsia is one of the most serious forms of preeclampsia and is highly related to obstetric morbidities and mortalities. Management for eclampsia is similar to those for any form of severe preeclampsia, and most patients recover well without neurological sequelae [6][54].
Another frequent neurological finding is posterior reversible encephalopathy syndrome (PRES). PRES is a result of hypoxia and vasogenic edema of the brain that is often related to acute uncontrolled hypertension or systemic endothelial dysfunction. The syndrome progresses in a rather rapid manner but also resolves rapidly with a good prognosis once the trigger is withdrawn [7][55]. PRES is high among pregnant women with severe preeclampsia or eclampsia, and usually indicates a better prognosis than PRES in non-pregnant women or is associated with other causes [8][56].
Stroke—or a cerebrovascular accident—refers to a brain attack when impairment of part of the CBF or a burst in a brain blood vessel occurs. Strongly related to hypertensive disorders, cerebrovascular events are yet another complication that is significantly linked to preeclampsia. Although uncommon in pregnancy, it shares similar disease pathways and risk factors with strokes that take place in non-pregnant patients, and thus is indicative of an increased long-term risk for stroke events [9][57].
3. Cardiovascular Systems
Preeclampsia has been classified as one independent gender-specific risk factor for cardiovascular events by the American Heart Association (AHA). Studies have proven that women with gestational hypertensive disorders carry a 2- to 4-fold risk for cardiovascular diseases [10][58]. In fact, preeclampsia and cardiovascular diseases share many predisposing factors such as elevated blood pressure and increased BMI. The disease spectrum includes coronary heart disease, heart failure, and cardiovascular disease death, and the influences may be life-long [11][59].
The long-term cardiovascular sequelae not only affect the mother but have also proven to bring hazards to her children at the same time. Although the establishment of a dependency relationship is difficult, many studies have shown an increased rate of congenital heart disease and future cardiovascular morbidities for offspring. Some scholars believe, however, that the influences of cardiovascular risks on offspring are limited to term infants or cases with early preeclampsia [12][60].
The complex multifactorial nature of preeclampsia and cardiovascular diseases makes it hard to make a straightforward ascription of the latter to the former. There is also a lack of a standardized protocol for cardiovascular prevention. Nevertheless, medical staff and preeclamptic patients should keep in mind the importance of continuous screening and early intervention of cardiovascular diseases. Monitoring of the body weight, blood pressure, lipid level, and lifestyle should be performed every five years until the age of 50 when women would qualify for most other international regular cardiovascular risk assessment guidelines [13][61].
4. Liver
Preeclampsia-related liver disease is frequently seen in the third trimester. Liver involvement is rare but indicative of severe disease extent. The most notorious example is H(Hemolysis)EL(Elevated Liver Enzymes)LP(Low Platelet Count) syndrome, which is a variant of severe preeclampsia. According to the diagnostic criteria of Tennessee Classification and Mississippi Classification, an elevated liver enzyme is usually defined by an elevated AST or ALT ≥ 70 U/L, although blood tests often reveal a level ≥ 500 U/L. Thrombotic microangiopathy serves as one of the possible explanations, while periportal hemorrhage and necrosis have been observed in histopathology studies. As rare as it may be, the condition could lead to hepatic rupture [14][62]. Women treated with corticosteroids exhibit overall improved laboratory results including liver function tests. Administration after delivery helps to avoid a rebound and further complications. Nevertheless, the natural course of HELLP could not be altered by corticosteroids [15][63].
Other liver diseases associated with preeclampsia include acute fatty liver of pregnancy (AFLP), hepatic infarction, and rupture. In cases of AFLP, laboratory abnormalities include elevated liver enzymes, prolonged prothrombin time and partial thromboplastin time, and increased bilirubin levels. Other typical clinical symptoms comprise central nervous system involvements such as headache and consciousness disturbances, jaundice, and gastrointestinal symptoms including anorexia, abdominal discomfort, nausea, and vomiting. If the expression of long-chain 3-hydroxyacyl-CoA dehydrogenase is not evident, the prognosis is usually good [16][64].
Hepatic complications in pregnancy are rare but could be fatal. They are more likely to be found in preeclamptic or eclamptic cases and indicate severe disease status. Hence, prompt termination of pregnancy or delivery is often indicated. Liver transplantation may be considered in patients with a grave prognosis [15][63].
5. Kidney
The imbalance of the renin-angiotensin aldosterone system (RAAS) along with the imbalance between proangiogenic and anti-angiogenic factors may explain the relationship between preeclampsia and renal impairment. Similar to cardiovascular risks, preeclampsia shares common predisposing factors with renal risks and confers a higher risk of chronic kidney diseases later in life [17][65].
The activation of RAAS is normal during pregnancy, which results in a volume increase. However, excessive activation possibly related to sFlt-1 and AT1-AAs—as may be seen in preeclamptic subjects—could lead to preeclampsia or preeclampsia-like syndrome. Once the delicate balance is disrupted, hypertension and renal involvements may be seen [18][66]. Thrombotic microangiopathies in renal cells have been observed in histopathology studies, suggesting glomerular injury in preeclamptic patients [19][67].
When acute kidney injury occurs, an abrupt increase in serum creatinine and a decrease in urine output could be detected. However, both the glomerular filtration rate and serum creatinine level are not perfectly reliable markers during pregnancy, as physiological changes allow an increase in the former and a reduction in the latter. The diagnosis may rely on other clinical manifestations such as oliguria, proteinuria, and edema, and is thereby delayed in some cases [20][68].
The condition may be life threatening, but also tends to regress rapidly in the postpartum period. Nonetheless, it still warrants concern for screening for later renal diseases. There is a significant association between preeclampsia—the early-onset subgroup in particular—and future chronic kidney diseases, hypertensive diseases, and glomerular or proteinuric diseases. For preeclamptic women, a 10- to 12-fold increase in end-stage renal disease has been proposed in existing statistical analyses. Hence, further screening for kidney diseases years after pregnancy should be implemented [21][69].
6. Other Targets
Preeclampsia is a global disorder that may present with symptoms and pathologic findings all over the body. Aside from the vital organs, for example, the hematologic system is another commonly affected target. In a study conducted by Neelam Jhajharia et al., lower hemoglobin and platelets were found in these patients, while higher WBC and hematocrit were observed [22][70]. Similar findings could also be found in other studies [23][24][71,72]. Some parameters may vary from study to study, but a trend of decreased hemoglobin and platelet levels is almost always observed in data analyses. Marked thrombocytopenia signifies a severe disease form, as manifested in HELLP syndrome.
Gastrointestinal involvements are common in preeclamptic patients. Symptoms of nausea and vomiting are frequently experienced by them, and some women complain of indigestion. The more devastating complications include hepatic involvement as described earlier, and pancreatic involvement, namely referring to the increased risk of pancreatitis and necrosis of the pancreas [25][73].
Another classic clinical manifestation of preeclampsia is edema. It is worth noting that edema is not essential to the diagnosis of preeclampsia and is often observed in normal pregnancies as a result of the increase in body fluids. General swelling due to water and salt retention is especially prominent in preeclampsia due to elevated blood pressure and endothelial injury causing extravasation from the vessels. As rare as it may be, one of the most severe presentations of fluid overload is pulmonary edema, which has been reported in cases of severe preeclampsia [26][74].
