You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is a comparison between Version 1 by Haiko Sprott and Version 2 by Camila Xu.
Hyaluronic acid (HA) is as naturally occurring glycosaminoglycan composed of repeating disaccharide units consisting of glucuronic acids and N-acetylglucosamine, resulting in different molecular weights. HA plays a crucial pathophysiological role in rheumatic diseases, especially concerning joint health and function.
- hyaluronic acid
- rheumatology
- osteoarthritis
- rheumatoid arthritis
- joint lubrication
1. Introduction
Hyaluronic acid (HA) plays an important role in a wide range of medical physiological and pathological conditions: Notably, it finds application in dermatology, ophthalmology, cosmetic medicine, and rheumatology [1][2][3][1,2,3]. Its significance extends to wound healing, granulation, and cell migration [4]. However, the efficacy of HA in rheumatology remains a subject of controversy at times [5][6][5,6].
HA is as naturally occurring glycosaminoglycan composed of repeating disaccharide units consisting of glucuronic acids and N-acetylglucosamine (Figure 1), resulting in different molecular weights [7][8][9][7,8,9]. This structural variability imparts diverse functional implications in both physiological and pathological contexts [10]. HA is commercially produced through extraction from animal tissues, such as chicken combs, and from Streptococci bacteria [11].
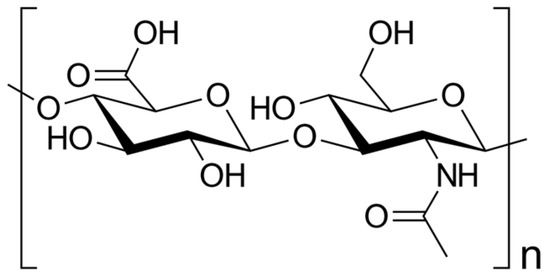
Figure 1. Skeletal formula of hyaluronan—a polymer consisting of D-glucuronic acid and N-acetyl-D-glucosamine linked via alternating β-(1→4) and β-(1→3) glycosidic bonds [7].
Functionally, HA demonstrates remarkable water-binding capacity, rendering it an essential constituent of the extracellular matrix (ECM) [12]. Its elongated, unbranched chains create a gel-like network, imparting hydration and lubrication to crucial tissues like the skin, cartilage, and synovial fluid [13][14][15][13,14,15].
In the field of rheumatology, HA has garnered substantial attention, owing to its pivotal involvement in joint health and its relevance to diseases like osteoarthritis (OA) and rheumatoid arthritis (RA) [16][17][16,17].
OA is a degenerative joint disorder characterized by the gradual deterioration of articular cartilage, resulting in pain, stiffness, and diminished joint function [18]. There is no cure for OA, so doctors usually treat OA symptoms with a combination of therapies [18]. HA serves as a lubricant and shock absorber within the synovial fluid, facilitating smooth joint movements [19]. However, in OA, the concentration and quality of HA decrease, compromising its protective and viscoelastic properties due to heightened degradation and decreased synthesis. Consequently, this leads to impaired cartilage function and joint degeneration [20]. As a therapeutic approach, supplementation with exogenous HA has emerged to alleviate symptoms and enhance joint function in OA patients [21]. By restoring synovial fluid viscosity and promoting cartilage repair, HA aids in improving joint mobility and reducing pain [16].
On the other hand, RA is an autoimmune and inflammatory disease characterized by the immune system mistakenly attacking healthy cells, resulting in inflammation, particularly in the joints, leading to painful swelling [22]. RA can be effectively treated and managed with medication(s) and self-management strategies [22]. In RA, the level of HA in the synovial fluid is significantly diminished, causing reduced lubrication and increased inflammation and pain [23].
Numerous studies have explored the potential therapeutic benefits of exogenous HA supplementation in rheumatic diseases. Through intra-articular injections, HA has shown promise in improving joint mobility, reducing pain, and promoting cartilage repair by restoring synovial fluid viscosity [24].
Furthermore, HA has demonstrated immunomodulatory effects, including the suppression of pro-inflammatory cytokines and the promotion of anti-inflammatory cytokine production [25]. This suggests that HA may also hold promise in the treatment of immune-mediated rheumatic diseases [26].
Moreover, researchers have explored HA’s potential applications in drug delivery systems and tissue engineering due to its biocompatibility and biodegradability [27].
However, the use of HA therapy in rheumatology remains a topic of controversy, with conflicting evidence regarding its efficacy and safety [5][28][5,28].
In summary, HA represents a promising therapeutic option in the field of rheumatology due to its potential to enhance joint function and alleviate inflammation and pain [29]. Nevertheless, further investigation is required to fully elucidate its therapeutic potential in rheumatic diseases.
2. Hyaluronic Acid: Structure, Function, and Biochemistry
HA plays a crucial role in diverse cellular and tissue processes, encompassing hydration, lubrication, tissue repair, regulation of inflammation, and cell signaling [14]. It is naturally synthesized by various cell types, predominantly fibroblasts, chondrocytes, and synoviocytes [30]. The biosynthesis of HA takes place in the plasma membrane through the coordinated activity of specific enzymes, including hyaluronan synthases [30].2.1. Molecular Structure of Hyaluronic Acid
Hyaluronan synthases catalyze the addition of glucuronic acid and N-acetylglucosamine, leading to the formation of the repeating disaccharide units that constitute HA [31]. The molecular weight of HA displays highly variability, ranging from several hundred kilo Da to millions of kilo Da, exerting a direct impact on its functional properties [32]: Notably, higher-molecular-weight HA exhibits increased viscosity [33], thereby affecting its flow and lubrication capability, i.e., in joints [34]. As a result, high-molecular-weight HA provides superior lubrication and cushioning effects [35].2.2. Biosynthesis and Degradation of Hyaluronic Acid
HA turnover in tissues is intricately regulated by a delicate balance between biosynthesis and degradation processes [36]. The degradation of HA primarily involves the action of enzymes known as hyaluronidases, which cleave HA into smaller fragments [37]. Hyaluronidase enzymes are categorized into several families, including HYAL1, HYAL2, and PH-20 [38], and they play a pivotal role in maintaining the appropriate concentration and size distribution of HA within tissues [39]. Furthermore, the degradation of HA can be modulated by reactive oxygen species, matrix metalloproteinases (MMPs), and other factors present in the extracellular environment [40].2.3. Physiological Functions and Distribution in Tissues of Hyaluronic Acid
HA plays a critical role in tissue repair and remodeling processes within the human body [41]. It participates in various stages of wound healing, encompassing inflammation, cell migration, proliferation, and ECM remodeling [42]. As a scaffolding molecule, HA provides essential structural support and aids in cell migration during tissue repair [43] (Table 1).Table 1.
Physiological functions of hyaluronic acid (HA) in rheumatology.
| Function | Mechanisms | References |
|---|---|---|
| Lubrication of joints | HA provides lubrication and viscoelastic properties to synovial fluid, reducing friction between joint surfaces and enhancing joint mobility. | [44] |
| Chondroprotection | HA exhibits chondroprotective effects by promoting cartilage matrix synthesis, reducing matrix degradation, and inhibiting the activity of proteolytic enzymes | [45][46][45,46] |
| Anti-inflammatory activity | HA can modulate inflammation by reducing the expression of pro-inflammatory cytokines and enzymes, inhibiting leukocyte migration, and suppressing immune responses. | [47][47[48],48] |
| Tissue repair and remodeling | HA plays a role in tissue repair and remodeling processes by promoting cell migration, angiogenesis, and extracellular matrix remodeling | [44][49][44,49] |
| Viscoelasticity | HA contributes to the viscoelastic properties of connective tissues, maintaining tissue integrity, elasticity, and shock-absorbing capabilities. | [48][50][48,50] |
Selected studies on the physiological role of HA in rheumatology. This is not an exhaustive list, and further research and clinical trials have been conducted in this field. For more detailed information, it is recommended to refer to the referenced papers.
During the inflammatory phase of wound healing, HA is involved in the recruitment and activation of immune cells, such as macrophages and neutrophils [51]. HA fragments generated during tissue injury can function as damage-associated molecular patterns and trigger immune responses [51]. Moreover, HA promotes the infiltration of immune cells into the wound site, facilitating the removal of debris and pathogens [52]. In the subsequent proliferative phase, HA contributes to cell migration and proliferation [53]. It forms a provisional matrix that guides cell movement and stimulates cell proliferation [53]. HA receptors, such as CD44 and RHAMM, mediate cell adhesion, migration, and signal transduction, enabling cells to migrate into the wound area and contribute to tissue repair [54]. Furthermore, HA plays a regulatory role in ECM remodeling during tissue repair [55]. It interacts with other components, such as fibronectin and collagen, promoting their assembly and organization [56]. HA also influences the activity of enzymes involved in ECM remodeling, such as MMPs and tissue inhibitors of MMPs, which are essential for matrix turnover and remodeling [57].
Beyond its involvement in tissue repair, HA also plays a role in tissue remodeling processes, such as embryonic development, organ morphogenesis, and angiogenesis [58]. HA provides a structural framework for cell migration and tissue organization during these processes [59]. It regulates cell behavior, including cell differentiation, proliferation, and survival, through interactions with specific receptors and signaling pathways [60].
Overall, HA exhibits a multifaceted role in tissue repair and remodeling, contributing to inflammation resolution, cell migration, proliferation, and ECM (re)organization [61]. Its involvement in these processes highlights its significance in wound healing, tissue regeneration, and developmental biology [62].
Regarding tissue distribution, HA is widely distributed throughout the body, with particularly high concentrations found in connective tissues, such as the skin, synovial fluid, and cartilage [63]. In the skin, HA resides in the ECM and contributes to tissue hydration, elasticity, and wound healing [64]. In the synovial fluid of joints, HA forms a viscous, gel-like substance that provides lubrication, shock absorption, and nutrient supply to the articular cartilage [65]. Additionally, HA is present in the vitreous humor of the eye, where it helps maintain the transparency and shape of the eyeball [66]. Moreover, HA is found in other tissues, including the umbilical cord, umbilical vessels, and embryonic tissues, where it plays crucial roles in development and tissue morphogenesis [67].
