Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Silvana Alfei and Version 2 by Camila Xu.
Generally, the term ‘cannabinoids’ refers to a heterogeneous family of compounds that exhibit activity upon particular human cannabinoid receptors, namely CB1 and CB2. They encompass the natural compounds present in the Cannabis plants, lipid mediators called ECs naturally produced by human cells, as well as by all vertebrates on planet Earth, and the synthetic analogs of both groups designed by scientist, called SCs.
- bacterial resistance
- methicillin-resistant S. aureus (MRSA)
- multi drug resistant (MDR) bacteria
- Cannabis sativa
- phytocannabinoids (PCs)
1. Introduction
Given the rapid emergence of multi drug resistant (MDR), extensively drug-resistant (XDR) and pandrug-resistant (PDR) pathogens, against which current antibiotics are no longer functioning, we are rapidly moving into a post-antibiotic era where infections will be practically untreatable [1]. According to the definition of the World Health Organization (WHO), antimicrobial resistance is a natural event that occurs when microbes become tolerant to drugs originally active, thus rendering several infections more difficult or impossible to treat [2][3][2,3]. Particularly, WHO has identified twelve families of bacteria to be considered as the most dangerous to human health. These families have been assigned to three priority groups, comprising critical pathogens (Acinetobacter, Pseudomonas, and Enterobacteriaceae), high priority pathogens (Enterococcus faecium, Staphylococcus aureus, Helicobacter pylori, Campylobacter, Salmonella spp., and Neisseria gonorrhoeae), and medium priority pathogens (Streptococcus pneumoniae, and Shigella spp.) [3][4][3,4]. Resistance in bacteria can be acquired or natural, but several mechanisms exist by which pathogens can become resistant to antibiotics (Figure 1).
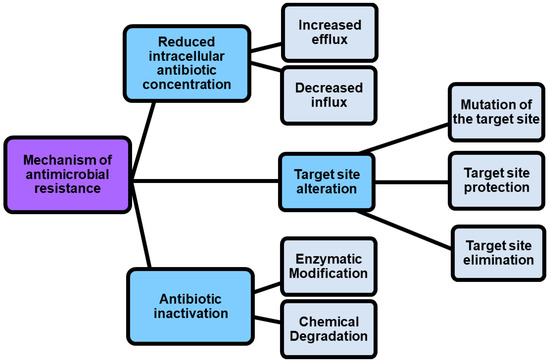
Figure 1.
Mechanisms by which pathogens can become resistant.
As shown in Figure 1, antimicrobial resistance mechanisms include drug inactivation, decreased intracellular drug concentration, and altered drug targets [5].
1.1. Mechanism of Antimicrobial Resistance vs. Strategies to Develop Novel Antibiotics
Drug inactivation can occur either by enzymatic or chemical degradation, while decreased intracellular drug concentration can occur because of increasing drugs efflux and decreasing drugs influx [5]. In this regard, porin mutations in resistant strains alter the permeability of bacterial membranes, thus reducing the uptake of antibiotics into the bacterial cell. On the contrary, the hyperexpression of efflux pumps, which pump antibiotics out of the cell, dramatically reduces their concentration inside the cell [6]. Also, by the action of enzymes that chemically modify components of the bacterial outer membrane essential for antibiotic binding, some Gram-negative bacteria such as P. aeruginosa, Acinetobacter baumannii and others develop resistance to glycopeptide and polymyxin antibiotics. Furthermore, methyltransferases are a class of enzymes capable to modify the target thus promoting the resistance to antibiotics including aminoglycoside, lincosamide, macrolide, streptogramin, and oxazolidinone [7]. Another phenomenon known as “target protection” occurs when antibiotic target’s resistance proteins, such as the tetracycline ribosomal protection proteins (TRPPs), protect bacteria from the antibiotic-induced inhibition [8]. Additionally, the antibiotic resistance could be caused by the use of antibiotics in feed diet for animal production. The overuse, abuse, and misuse of β-lactams, aminoglycosides, tetracyclines, macrolides, and other antibiotics, with the purpose of promoting the development of animals, can cause the presence of residual antibiotics in the products intended for human consumption obtained from those animals, and can determine antibiotics pollution into the environment [9][10][11][9,10,11]. It was reported that some bacterial infections in humans are sustained by animal pathogens, namely zoonotic pathogens, thus proving that antibiotic resistance can be directly or indirectly transmitted from animal to humans [9]. A few practices, including the improvement of animal feed, waste management, and animal natural immunity, as well as the use of antibiotic alternatives such as prebiotics, probiotic vaccines, and bacteriophages can regulate and limit the antibiotic resistance, thus maintaining the potency of the available drugs [12]. However, more strategies to counteract antibiotic resistance are necessary, and currently they include the use of nanotechnology, computational methods, the use of antibiotic alternatives, drug repurposing, the synthesis of novel antibacterial agents, prodrugs, the development of efficient diagnostic agents also named rapid diagnostic tests (RDTs), the use of combination therapy, as well as the awareness, and knowledge of antibiotic prescribing (Table 1).
Table 1.
Strategies for combating antibiotic resistance.
| Strategies for Combating Antibiotic Resistance | Ref. | |||
|---|---|---|---|---|
| Nanotechnology | Quality by design (QbD) approach | [13] | ||
| Computational methods | In silico modelling | [14] | ||
| Fragment-based drug design (FBDD) | CB2 | [15] | ||
| Peripheral immune system tissues | Spleen, tonsils, thymus, lymph nodes | Antibiotic alternatives | Antimicrobial peptides (AMPs) | [12] |
| [ | Essential oils | |||
| 47 | Anti-Quorum Sensing (QS) | |||
| ] | ||||
| Peripheral immune system cells | B cells, natural killer cells, monocytes, macrophages Neutrophils, CD8+ T cells, CD4+ T cells |
|||
| CNS * | Cerebellum, olfactory tubercle, striatum | Darobactins | ||
| Vitamin B6 | ||||
| Thalamic nuclei (hippocampus and amygdala) | Bacteriophages | |||
| Odilorhabdins | ||||
| 18-β-glycyrrhetinic acid | ||||
| Cannabinoids | ||||
| Drug reproposing | Ticagrelor | [16] | ||
* Under certain circumstances, most notably during inflammation.
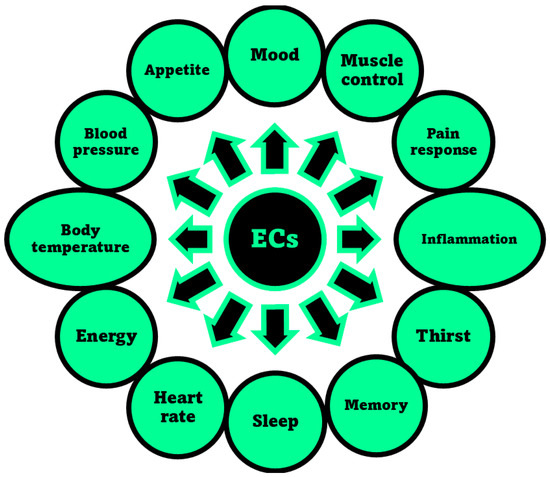
Figure 4. Aspects of humans’ life regulated by the ECS, through the interaction of ECs with receptors CB1 and/or CB2, as reported in the relevant review by Sharma et al. [52].
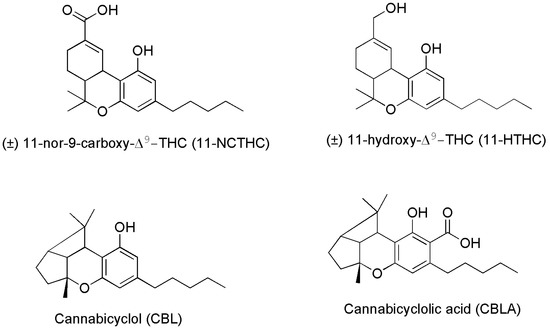
Figure 5.
Chemical structure of two THC metabolites (11-NCTHC and 11-HTHC) and of two products deriving from CBCA degradation.
Structural Differences between Psychotropic and Not-Psychotropic PCs
It has been reported that the n-pentyl chain at the C-(3) position (Figure 2) works and essential role in the activity of psychotropic THC derivatives and that modification in this side chain leads to critical changes in the affinity, selectivity and pharmaco-potency of these ligands relating to the CB1 and CB2 cannabinoid receptors. Generally, while a shorter alkyl chain reduces the affinity of the compound for the cannabinoid receptor, an increase in the number of carbon atoms (hexyl, heptyl, or octyl) leads to an increase affinity for the same cannabinoid receptor [56][57][56,57]. Additionally, a number of other transformations in the tricyclic core of the THC cannabinoid structure have been carried out [58]. Particularly, the pyran ring-opening generally causes in the achieved compound a relative reduction in the affinity to the CB1/CB2 cannabinoid receptors, and in the psycho activity. In this regard, the absence of the tricyclic core in CBC, CBD and CBG for CB2 receptors, could be responsible for the for their higher affinity for CB2 receptors dealing with beneficial pharmacological properties, thus not exerting psychotropic effects [59].2.2. Synthetic Cannabinoids (SCs)
The third group of cannabinoids consists of synthetic analogs of both ECs and PCs groups, appositely designed by scientists in the field, to enhance the benefits and therapeutic properties of ECs and PCs, while reducing the psychotropic and adverse effects. Among others, they include the compounds reported as examples in Figure 6 (chemical structures), and Table 3 (pharmacological properties and selectivity for receptors CB1 and CB2), which have demonstrated to be promising for treating severe humans’ chronic diseases including breast and prostate tumors, the unpleasant side-effects of chemotherapy, and chronic pain [42].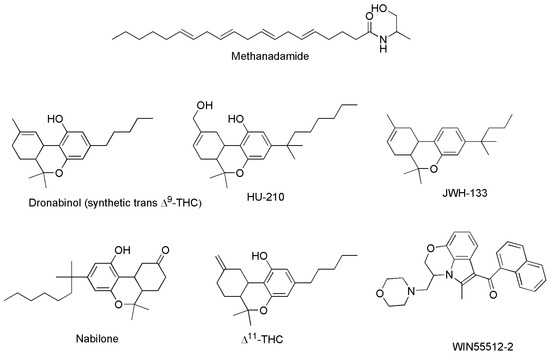
Figure 6.
Structure of some SCs capable to act on CB1 and/or CB2 receptors.
Table 3.
Selectivity of some SCs for CB1 and CB2 receptors, and their effects.
| SCs | Binding Affinity | Effects | Refs. | |
|---|---|---|---|---|
| CB1 (Ki, nM) | CB2 (Ki, nM) | |||
| Dronabinol * | 15 | 51 | Appetite stimulant Psychotropic effects Analgesic ↓ Nausea Antiemetic |
[60] |
| Methanandamide (AM-356) | 20 | 815 | [61] | |
| SR144528 | 280 | 0.1 | Anti-inflammatory Analgesic ↓ Neuropathic pain |
[48] |
| Cannabinor # (PRS-211,375) |
5585 | 17.4 | [62] | |
| CP47,597 | 2.1 (Kd) | 56 | Analgesic | [48] |
| JTE907 | 490 | 2.2 | Anti-inflammatory | [48] |
| JWH133 | 680 | 3.4 | ↓↓ Neurotoxicity Anti-inflammatory ↓ Alzheimer symptoms |
[48] |
| AM1241 | 272 | 3.4 | Analgesic effects ↓ Hyperalgesia ↓ Allodynia Amyotrophic lateral sclerosis |
[48] |
| GW405,833 | 8640 | 7.2 | ↓ Hyperalgesia ↓ Allodynia |
[48] |
| L-759,633 | 1604 | 9.8 | Analgesic Antianxiety Antidepressant Anti-inflammatory ↓ Alzheimer symptoms |
[48] |
| JWH139 | 2290 | 14 | ||
| HU308 | 115,000 | 23 | ||
| AM630 | ||||
| Mitomycin C (MMC) | ||||
| Auranofin | ||||
| Pentamidine | ||||
| Zidovudine (AZT) | ||||
| Synthesis of novel antibacterial agents | Lactones | [17] | ||
| Piperidinol | [18] | |||
| Sugar-based bactericides | [19] | |||
| Isoxazole derivatives | [20] | |||
| Carbazole | [21] | |||
| Prodrugs | Siderophores | [22] | ||
| Carbapenem-oxazolidinones | ||||
| Oral Gyrb/ParE dual binding inhibitor | ||||
| AMPs prodrugs | ||||
| Development of efficient diagnostic agents (RDTs) |
Point-of-care tests (POCTs) Molecular (genotyping) assays |
[23] | ||
| Combination therapy | Penicillin with streptomycin * Rifampin–isoniazid–pyrazinamide ** Trimethoprim-sulfamethoxazole Quinupristin-dalfopristin Bacitracin-polymyxin B Bacitracin-polymyxin B-gramicidin Neomycin,-bacitracin-gramicidin |
[24] | ||
| β-Lactams antibiotics-β-Lactamase inhibitors *** |
[25][26][25,26] | |||
| Awareness and knowledge of antibiotic prescribing | [27] | |||
RDTs = rapid diagnostic tests; * For enterococcal infections; ** in the treatment of tuberculosis; *** ceftazidime/avibactam, meropenem/vaborbactam and imipenem/relebactam.
1.2. Cannabinoids as Strategic Compounds to Develop New Antibiotics
Omitting to comment on each strategy reported in Table 1, and instead focusing on the development of alternative antibiotics, it can be observed that cannabinoids, better known for many other pharmacological and psychotropic effects are included in this category. Particularly, cannabinoids are prenylated polyketides produced in Cannabis plants and particularly in Cannabis sativa, which is an herbaceous plant that has been used for millennia for both medicinal and recreational purposes. C. sativa possesses a plethora of pharmacological properties and mind-altering effects, largely due to its content in cannabinoids, more precisely phytocannabinois (PCs), given their vegetable origin [28]. Collectively, more than 1600 chemical compounds have been isolated from C. sativa, of which over 500 are phytochemicals including cannabinoids, flavonoids terpenoids and sterols [28]. Among phytochemicals, more than 180 are cannabinoids, about 125 have been isolated, that can be classified into 11 structural families [28][29][28,29]. The most abundant representatives of these families are Δ9-tetrahydrocannabinol (Δ9-THC, also the main psychoactive cannabinoid), cannabidiol (CBD), and cannabichromene (CBC). Additionally, other classes whose prototypes are Δ8-E-tetrahydrocannabinol (Δ8-THC), cannabigerol (CBG), cannabinodiol (CBND), cannabielsoin (CBE), cannabicyclol (CBL), cannabinol (CBN), cannabitriol (CBT), and a miscellaneous group have been identified [28][29][28,29]. Currently, despite its psychotropic effects, Δ9- THC is used as therapeutic agent in the treatment of chemotherapy-associated nausea and vomiting, AIDS related loss of appetite, as well as pain and muscle spasms in multiple sclerosis [30]. Also, its carboxylic acid precursor, THCA, not exerting psycho-active effects in humans, is currently examined for its immunomodulatory, anti-inflammatory, neuroprotective and anti-neoplastic effects as well for its effectiveness in reducing adiposity and preventing metabolic disease caused by diet-induced obesity [31]. CBD, non-psychotropic as well, is currently investigated for application in the treatment of Alzheimer’s disease, Parkinson’s disease, epilepsy, cancer and for its neuroprotective efficacy [32]. Although the most studied cannabinoids for medicinal purposes are CBD and Δ9-THC, nowadays the research focus moves increasingly towards other PCs, such as the not psychoactive CBC, currently investigated for its anti-inflammatory, anti-fungal, antibiotic and analgesic effects [30], CBG and cannabigerolic acid (CBGA), which is the precursor of the decarboxylated CBG and could be considered as the “mother of all cannabinoids” (see later). Particularly, CBG has many putative benefits ranging from anti-inflammatory action to pain reliever [33]. Among other more investigated therapeutic properties, PCs including Δ9-THC, Δ8-THC, CBD, CBN, CBG, and CBC and some their correspondent carboxylic acids have shown from moderate to potent antimicrobial properties mainly against Gram-positive bacteria (MICs 0.5–8 µg/mL), and especially against strains of S. aureus, including MRSA, EMRSA, as well as fluoroquinolone and tetracycline-resistant strains, [34]. Particularly, even if the precise mechanisms used by PCs remains unknown so far, recent investigations have revealed that PCs inhibits bacteria by injuring their cytoplasmic membrane [35][36][35,36]. Recently, Luz-Veiga et al. have reported the antibacterial activity of both CBD and CBG, being CBG the most potent compound, and their capability to inhibit Staphylococci adherence to keratinocytes without compromising skin microbiota, thus being very promising as antibacterial agents to treat skin infection by topical administration [37]. Blaskovich et al., in addition to confirm the antibacterial activity of CBD on Gram-positive pathogens, including highly resistant S. aureus, S. pneumoniae, and Clostridioides difficile, demonstrated that CBD has excellent activity against biofilms, little propensity to induce resistance, and topical in vivo efficacy [38]. Moreover, the authors reported that CBD can selectively kill a subset of Gram-negative bacteria that includes the ‘urgent threat’ pathogen Neisseria gonorrhoeae [38]. Additionally, the interaction of CBD with broad-spectrum antibiotics such as ampicillin, kanamycin, and polymyxin B was studied by Gildea et al. [39]. By disrupting membrane integrity at extremely low dosages, CBD-antibiotic co-therapy showed synergistic activity against Salmonella typhimurium, offering an intriguing alternative in the treatment of this clinically relevant bacterium. The impressively strong antibacterial activity against MRSA of CBG has been reported by Farha et al. in the year 2020 [33]. Even in comparison with standard therapy with vancomycin, CBG outcompetes classical approaches against MRSA. Additionally, CBG demonstrated to inhibit the capability of MRSA to generate de novo biofilm, showed to succeed in disaggregating the pre-formed biofilm, to kill rapidly stationary phase cells (persisters), and to effectively inhibit MRSA also in vivo, in a murine model. The authors speculated that C. sativa may produce PCs as a natural defense mechanism against pathogens and suggested PCs as a new compound class serving as novel antibiotic drug [33].
Unfortunately, since in C. sativa, CBGA is promptly and directly converted to CBDA and THCA, leaving no CBGA pool available to form CBG, the CBG levels in plants are exceptionally low. In this context, it has been suggested that a possible strategy to increase the CBG yield from hemp biomass could consist in harvesting much earlier in the ripening phase of the plants before the other cannabinoids are formed and detract the CBGA from the cannabinoid pool [40]. On the other hand, having available reliable synthetic procedures to prepare natural PCs would consent the accessibility to considerable quantities of CBG, as well as of other microbiologically promising minor cannabinoids, unlikely provided naturally by Cannabis plants, thus allowing further studies finalized to the development of novel PCs-based antibiotics.
2. Phytocannabinoids (PCs), Endocannabinoids (ECs) and Synthetic Cannabinoids (SCs)
2.1. Phytocannabinoids (PCs) and Endocannabinoids (ECs)
Generally, the term ‘cannabinoids’ refers to a heterogeneous family of compounds that exhibit activity upon particular human cannabinoid receptors, namely CB1 and CB2 [41][42][41,42]. They encompass the natural compounds present in the Cannabis plants, lipid mediators called ECs naturally produced by human cells, as well as by all vertebrates on planet Earth, and the synthetic analogs of both groups designed by scientist, called SCs [42]. Natural cannabinoids from Cannabis are more specifically called PCs referring to their original plant source, differently from ECs which are produced from human cells [43][44][43,44]. PCs and ECs could include compounds structurally very different both between the two families and inside the same class, as shown in Figure 2 and Figure 3, which report the structure of the most relevant PCs and ECs, respectively.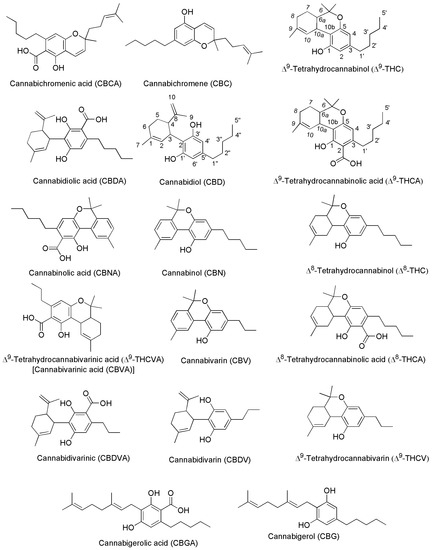
Figure 2.
Chemical structure of the main PCs found in
C. sativa
acting on CB1 and/or CB2 receptors.
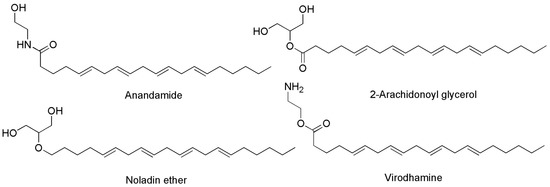
Figure 3.
Chemical structure of the main ECs found in humans acting on CB1 and/or CB2 receptors.
Table 2.
Locations of CB1 and CB2 receptors in the human body.
| Receptor Type | Location | Sublocation | Ref. | |
|---|---|---|---|---|
| CB1 | Central nervous system (CNS) | Hippocampus, cerebellum, basal ganglia, cortical regions Olfactory areas |
[46] | |
| Peripheral nerve terminals Extra-neuronal sites |
Eye, vascular endothelium, adipose tissue, lungs, liver Spleen, kidneys, uterus, prostate, testis, stomach, placenta Skeletal, muscles |
|||
| 3795 | ||||
| 32 | ||||
| HU-210 | ||||
| 0.061 | ||||
| 0.52 | ||||
| [ | 63 | ] | ||
| L-759,656 | 4888 | ↑11.8 | [64] | |
| WIN 55,212-2 | 1.9 | Analgesic Anti-inflammatory ↓ Alzheimer symptoms |
[65] | |
| JWH015 | 383 | 13.8 | Analgesic Anti-inflammatory |
[66] |
| WIN 48,098 (Pravadoline) | 4.9 (IC50) | Analgesic Anti-inflammatory |
[67] |
Ki = Defined kinetically as the ratio of rate constants koff/kon for the binding of a ligand to the receptor. This is the same as Kd; IC50 = the concentration of ligand required to saturate half of the receptor; * Approved by the FDA as safe and effective for HIV/AIDS-induced anorexia and chemotherapy-induced nausea and vomiting only; # failed in Phase IIb human clinical trials due to lack of efficacy; ↓ = reduction of; ↓↓ = strong reduction of.
On the base of their affinity and selectivity for receptors CB1 and CB2, they can exert both therapeutic and psychotropic effects, or mainly one of the two. Table 3 summarizes the selectivity of some SCs for CB1 and CB2, and their therapeutic effects.
The following Figure 7 shows the chemical structures of compounds in Table 3 not previously reported in Figure 6.
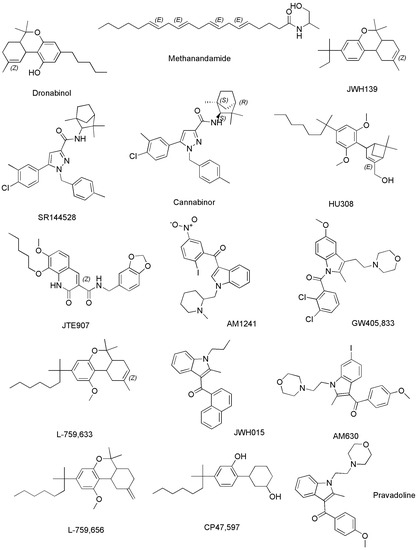 Methanandamide (AM-356) is a synthetically constructed stable chiral analog of anandamide. AM-356 acts on the cannabinoid receptors, and specifically on CB1-type receptors in the CNS found in mammals, fish, and certain invertebrates (e.g., Hydra), thus resulting also a psychoactive compound [68]. HU-210, as well as other SCs including L-759,656, HU-308, L-759,633, L-768,242 etc. are potent analgesic and anti-inflammatory compounds with many of the same effects as natural THC [44]. WIN 55,212-2 is an organic heterotricyclic SC. Particularly, it is the 5-methyl-3-(morpholin-4-ylmethyl)-2,3-dihydro [1,4]oxazine [2,3,4-hi]indole substituted at position 6 by a 1-naphthylcarbonyl group. It has a role as an analgesic, and neuroprotective agent, as well as an apoptosis inhibitor [69].
JWH-133 is a Δ9-tetrahydrocannabinol lacking the hydroxy group and having a 1,1-dimethylbutyl group at position 3 in place of the pentyl group. It acts as potent and highly selective CB2 receptor agonist, thus exerting antineoplastic effects, and working as a vasodilator and an anti-inflammatory agent, as an apoptosis inhibitor, as well as an analgesic molecule [70].
Δ11-THC, also known as exo-tetrahydrocannabinol, is a synthetic isomer of tetrahydrocannabinol, developed in the 1970s. It can be synthesized from Δ8-THC by several different routes, and only the (6aR, 10aR) enantiomer is known. In animal studies in mice, it was found to exert the same effect of Δ9-THC with around 1/4 its potency. It has been identified as a component of “vaping liquids” sold for use in humans [71].
Methanandamide (AM-356) is a synthetically constructed stable chiral analog of anandamide. AM-356 acts on the cannabinoid receptors, and specifically on CB1-type receptors in the CNS found in mammals, fish, and certain invertebrates (e.g., Hydra), thus resulting also a psychoactive compound [68]. HU-210, as well as other SCs including L-759,656, HU-308, L-759,633, L-768,242 etc. are potent analgesic and anti-inflammatory compounds with many of the same effects as natural THC [44]. WIN 55,212-2 is an organic heterotricyclic SC. Particularly, it is the 5-methyl-3-(morpholin-4-ylmethyl)-2,3-dihydro [1,4]oxazine [2,3,4-hi]indole substituted at position 6 by a 1-naphthylcarbonyl group. It has a role as an analgesic, and neuroprotective agent, as well as an apoptosis inhibitor [69].
JWH-133 is a Δ9-tetrahydrocannabinol lacking the hydroxy group and having a 1,1-dimethylbutyl group at position 3 in place of the pentyl group. It acts as potent and highly selective CB2 receptor agonist, thus exerting antineoplastic effects, and working as a vasodilator and an anti-inflammatory agent, as an apoptosis inhibitor, as well as an analgesic molecule [70].
Δ11-THC, also known as exo-tetrahydrocannabinol, is a synthetic isomer of tetrahydrocannabinol, developed in the 1970s. It can be synthesized from Δ8-THC by several different routes, and only the (6aR, 10aR) enantiomer is known. In animal studies in mice, it was found to exert the same effect of Δ9-THC with around 1/4 its potency. It has been identified as a component of “vaping liquids” sold for use in humans [71].
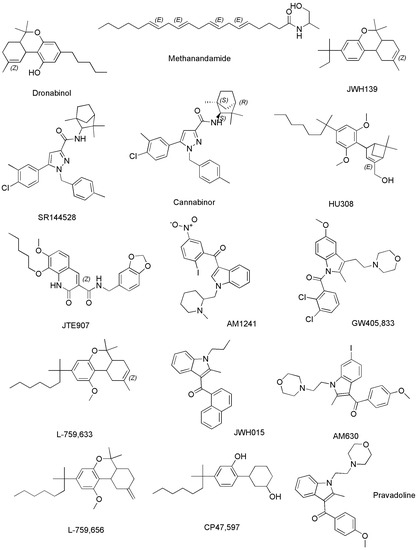
Figure 7.
Structure of SCs capable to act on CB1 and/or CB2 reported in
Table 3
and not previously shown in
Figure 6
.
