Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Francesco Prata and Version 2 by Jessie Wu.
The advent of robotic surgical systems had a significant impact on every surgical area, especially urology, gynecology, and general and cardiac surgery.
- robotic surgery
- robotic platform
- technology
1. Introduction
Even though the term “robot” may seem like a modern idea, the concept of machines operating independently has been around for centuries. Already, by 3000 years BC, the ancient Egyptians had developed water clocks that featured miniature human figures to strike bells at regular intervals. Around 400 BC, Archytus of Taremtum, the brilliant mind behind the creation of pulleys and screws, designed a wooden pigeon with the astonishing ability to fly. Moving forward to the twelfth century AD, Ismail al-Jazari, hailed as the “father of robotics” and modern-day engineering, authored The Book of Knowledge of Ingenious Mechanical Devices where he detailed 50 machines, along with instructions on how to construct them. Subsequent centuries witnessed an exponential growth in ingenious automated machines, ushering in a relatively prosperous era of robotic inventions that reached its apex in the fifteenth century with Leonardo Da Vinci, who fascinated the world with a plethora of robotic marvels, ranging from humanlike to animal-like designs. Although many of Da Vinci’s designs were left unfinished, they were undeniably ahead of their time and have since served as a wellspring of inspiration for modern-day robots utilized in various fields such as medicine and astronomy. In fact, the word “robot” was initially coined by Joseph Capek in 1921, in his play Rossom’s Universal Robots, derived from the Czech “robota” meaning “forced labor.” Over time, the term has come to reflect a repetitive task performed by machines.
2. Robotic Surgical Device
The incorporation of robotics in surgical procedures emerged as a response to the urgency to attain telepresence and execute repetitive and precise tasks. The first need was fulfilled in 1951, through the work of Raymond Goertz at the Atomic Energy Commission (USA), who designed a remotely operated mechanical arm to handle hazardous radioactive components [1][2][3][2,3,4]. The second goal was attained a decade later, when Joseph Engelberger and George Devol produced for General Motors the very first Unimate® industrial robot [1][2] These significant accomplishments were instrumental in paving the way for the integration of robotics in various other areas of industry across the globe.
The concept of utilizing robotics in surgical procedures originated more than 50 years ago, but it was not until the late 1980s that actual use began. Kwoh et al. are often credited with the honor of the first modern robotic procedure, as they utilized the PUMA 560 robotic system for neurosurgical biopsies, effectively performing stereo-tactic brain surgery [4][5]. Davies et al. later used the same system for the transurethral resection of the prostate, which led to the development of the PROBOT®. The latter was specifically conceived by Surgical Supplies Ltd. (Dairy Flat, New Zealand) to guide the motion of a rotating blade within a predefined virtual reconstruction of the prostate, obtained through ultrasound scans [5][6]. Though, due to the need for manual coagulation of the prostatic fossa at the end of the procedure and because of the poor accuracy of three-dimensional reconstructions of the enlarged gland, the diffusion of PROBOT® was limited [4][6][7][5,7,8]. However, this did not prevent the application of the same technology to orthopedic prosthetic surgery, leading to the creation of ROBODOC®, the first robot approved by the Food and Drugs Administration (FDA) [8][9].
Although there was an initial interest in active robotic systems that can autonomously perform predefined tasks, the predominant type that has gained widespread use is the master–slave one, which solely relies on the surgeon’s actions, without any pre-programmed or self-governing elements [9][10][11][10,11,12]. This evolution can be easily understood considering the nature of surgery, which seems to be an unsuitable profession for the utilization of fully automated robotic systems. In fact, sensitivity, empathy, adaptability, and decision-making abilities displayed by doctors are indispensable qualities when operating on the delicate boundary between health and disease, between life and death. The first surgical robot of this type was conceived in the late 1980s by Dr Phil Green, of the Stanford Research Institute (SRI, later SRI International), combining technologies for three-dimensional vision (developed by the National Aeronautics and Space Administration, NASA, in the 1960s) and telepresence [12][13]. The first prototype (SRI Green Telepresence) consisted of two distinct segments, the telepresence surgeon’s workstation (TSW) and the remote surgical unit (RSU). The former was equipped with a stereoscopic video monitor and a pair of instrument manipulators that relayed hand movements to the RSU. The monitor itself offered a field of view of 120 degrees and required the surgeon to wear passive polarized glasses for a clear 3D image. The RSU, on the other hand, was comprised of manipulator end-effectors with interchangeable instrument tips that could be swapped out via a twist-lock system, facilitating the use of forceps, needle drivers, bowel graspers, scalpels, and cautery tips. The unit additionally featured a pair of stereographic video cameras designed to follow the surgeon’s natural line of sight. In the early 1990s, these prototypes came under the control of the Advanced Biomedical Technologies program. In those years, in fact, the Defense Advanced Research Projects Agency (DARPA) pursued the ambitious project of halving casualties on the battlefield by cutting first aid response times, without endangering the health of military doctors [13][14][14,15]. This could be achieved through the use of an armored vehicle, deployed on the front line, equipped with a RSU (MEDFAST) through which the surgeon, using a TSW installed in the second lines, could carry out “damage control surgery” interventions from the distance [15][16]. In June of 1993, the telepresence surgical system was presented for the first-time during field exercises at Fort Gordon in Augusta (USA). One year later, in October of 1994, the complete system was showcased at the Association of the U.S. Army Annual Convention, where attendees were encouraged to try their hand at operating on a bleeding mannequin using the SRI: remarkably, even those lacking any surgical experience were able to successfully complete a suture and knot on the tissue, highlighting the system’s inherent user-friendliness and marking the conclusion of its initial development stages [16][17].
The SRI system was never intended for commercialization, but rather as a research prototype. However, the extraordinary results achieved up until then did not take long to attract private investors. Thus, in the early 90s, the two companies that would dominate the scene of robotic surgery for a decade came to life.
In 1994, the Automated Endoscopic System for Optimal Positioning® (AESOP), manufactured by the Computer Motion Inc. (Goleta, CA, USA), was cleared by the FDA to assist surgeons performing minimally invasive surgery. This robotic arm was specifically designed to provide direct control over the laparoscopic camera, using either a foot pedal or voice commands. It ensured a steady view of the operative field and eliminated the need for a surgical assistant, reducing the risk of fatigue during lengthy procedures [17][18]. Numerous reports describe its utilization in laparoscopic cholecystectomies, hernioplasties, fundoplications, and colectomies [18][19].
In 1995, Intuitive Surgical was founded in California (USA) by Frederick H. Moll and Robert Younge. They reworked the SRI Green Telepresence and created their first prototype, named Lenny, which featured three separate robotic arms attached to the operating table: two were equipped with surgical instruments, while the third arm held the camera. In 1997, Mona, Intuitive’s second-generation robot, became the first surgical platform employed in human trials as J. Himpens and G. Cardiere, bariatric surgeons from Saint-Blasium General Hospital in Belgium, used it to perform a cholecystectomy [19][20]. In 1998, a third generation of robots was introduced: the articulated wrists of the daVinci® robotic arms, characterized by 6 degrees of freedom, enabled cardiac surgeons from the Leipzig Heart Center (Leipzig, Germany) to perform minimally invasive cardiac valve repairs and coronary artery bypass graft surgeries [20][21]. The introduction of EndoWrist® technology has indeed marked a significant turning point in the adoption of surgical robots. In fact, conventional laparoscopy, which had already demonstrated the benefits of a minimally invasive approach since the 1980s, had one inherent major flaw: the lack of articulating instruments. This limitation made tasks like intracorporeal suturing extremely challenging. As a result, laparoscopic training required long learning curves and led to the concentration of the widest range of surgical cases in the hands of a few experienced surgeons. The advent of robotic platforms has democratized minimally invasive surgery, enabling a larger number of doctors to approach this type of procedure.
Computer Motion replied, launching the ZEUS® Robotic Surgical System (ZRSS) on the market, which was obtained coupling the AESOP with two other robotic arms with four degrees of freedom. Such a “patient-side” system, affixed to the operating table, was operated through a “surgeon-side” console, capable of minimizing the resting tremor and downscaling the hand movements to a range of 2:1 to 10:1 [21][22]. Although the system was initially employed in a fallopian tube anastomosis, in 1998 [22][23], its primary focus was on cardiac surgery, including mammary artery harvest and coronary artery bypass [19][23][24][25][20,24,25,26]. On 3 September 2001, ZEUS® made history by allowing the first transatlantic telesurgery: in this groundbreaking event, Jacques Marescaux, from New York (USA), successfully performed a laparoscopic cholecystectomy in Strasbourg (France) [21][26][22,27].
In 2000, the daVinci® received FDA approval for general laparoscopic procedures, becoming the first surgical robot used in operations in the United States. The Vattikuti Institute of Detroit documented the Vattikuti Institute prostatectomy, which would later become known as the robotic-assisted prostatectomy, with positive outcomes [27][28][29][30][31][28,29,30,31,32]. In comparison to the ZEUS® device, the daVinci® offered a stand-alone cart housing patient-side components, stereoscopic viewer improvements, and a more ergonomic design.
Intuitive and Computer Motion engaged in a legal battle for 3 years until their merger in 2003, ultimately resulting in the phasing out of ZEUS® and the integration of some of its elements into later iterations of the daVinci®. A timeline of surgical robotics development is represented in Figure 1.
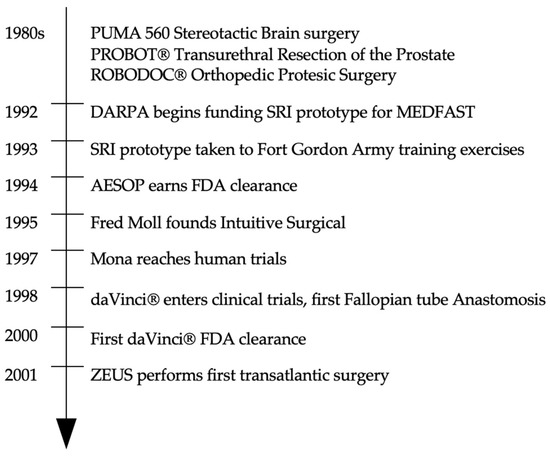
Figure 1.
Timeline of surgical robotics development.
