Obesity is a long-term condition resulting from a continuous imbalance between the amount of energy consumed and expended. It is associated with premature mortality and contributes to a large portion of the global chronic disease burden, including diabesity, cardiovascular disease, hypertension, and some cancers. While lifestyle changes and dietary adjustments are the primary ways to manage obesity, they may not always be sufficient for long-term weight loss. In these cases, medication may be necessary. However, the options for drugs are limited due to their potential side effects. As a result, there is a need to identify safe and effective alternative treatments. Recently, dDietary compounds, plants, and bioactive phytochemicals have been considered as promising sources for discovering new pharmacological agents to treat obesity and its related complications. These natural products can function independently or synergistically with other plants to augment their effects at various levels of the body. They can modulate appetite, lipase activity, thermogenesis and fat synthesis and degradation, satiation, adipogenesis, and adipocyte apoptosis. Additionally, targeting adipocyte growth and differentiation with diverse medicinal plants/diet is a significant strategy for devising new anti-obesity drugs that can intervene in preadipocytes, maturing preadipocytes, and mature adipocytes.
- obesity
- diabetes
- hypertension
- cardiovascular disease
- inflammation
1. Introduction
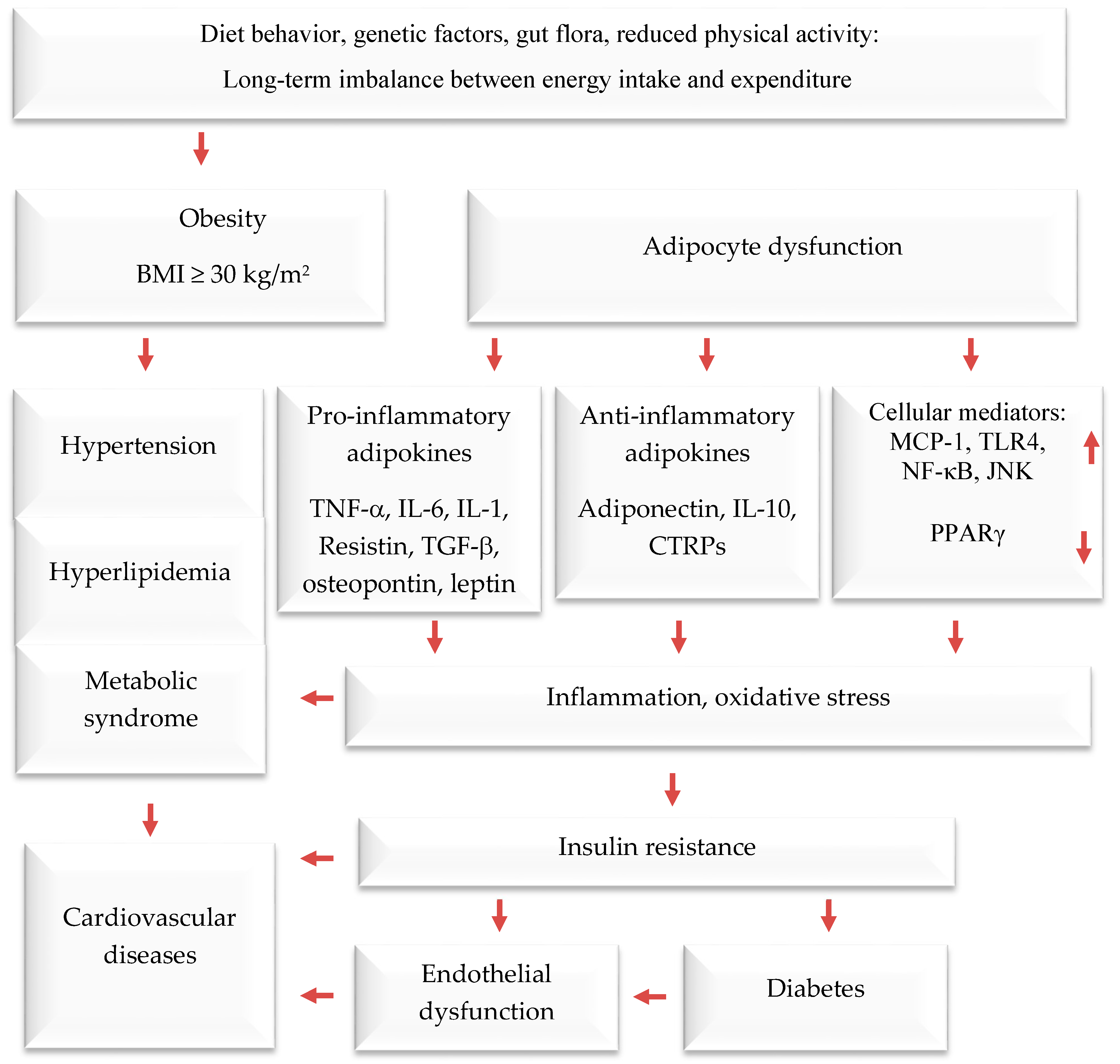
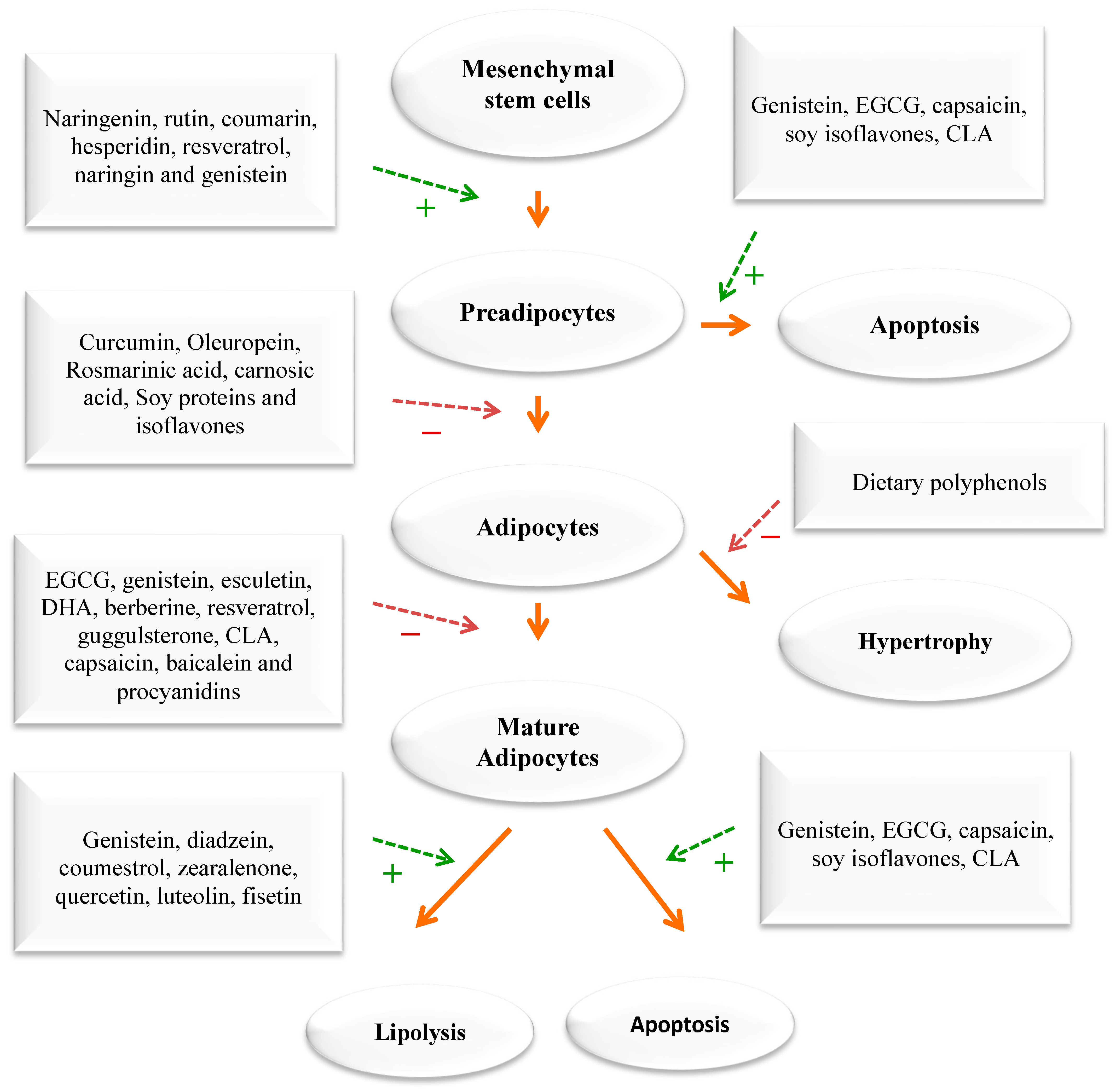
2. Prevention and Treatment of Obesity by Mediterranean Dietary Compounds and Wild Plants
In addition to using the whole herb or its extracts, numerous scientific in vitro and clinical trials have confirmed the anti-obesity activities of phytochemicals [33,35,36,37][31][32][33][34]. The pharmacological mechanisms of the anti-obesity effects of active compounds from pomegranate, citrus fruits, rosemary, black seeds, cumin, ginger, olive leave/oil, turmeric, cinnamon, fenugreek, and garlic have been evaluated through tests on cells, animals, and humans [33,34,35,36,37][31][32][33][34][35]. Dietary compounds, medicinal plants, and phytochemicals generated from them were reported to fight obesity by affecting different processes in the body. These include the blocking of pancreatic lipase and glucosidase, the suppression of hunger, the stimulation of thermogenesis and lipid metabolism, and the inhibition of fat breakdown and adipogenesis (Figure 2). Phytochemicals have been found to target fat cells in several ways, including inhibiting fat cell formation, promoting fat breakdown, and reducing energy intake while increasing energy expenditure (Figure 3). These findings come mainly from laboratory and animal studies. However, more high-quality research is needed to confirm the effectiveness of these phytochemicals in humans. Some examples of polyphenols include quercetin, myricetin, diadzein, genistein, cyanidin, luteolin, apigenin, kaempferol, proanthocyanidin, xanthohumol, and epigallocatechin gallate (EGCG). Numerous scientific studies demonstrated that these compounds exhibit weight-reducing and anti-obesity effects [33,35,36,37,38,39][31][32][33][34][36][37] (Figure 2).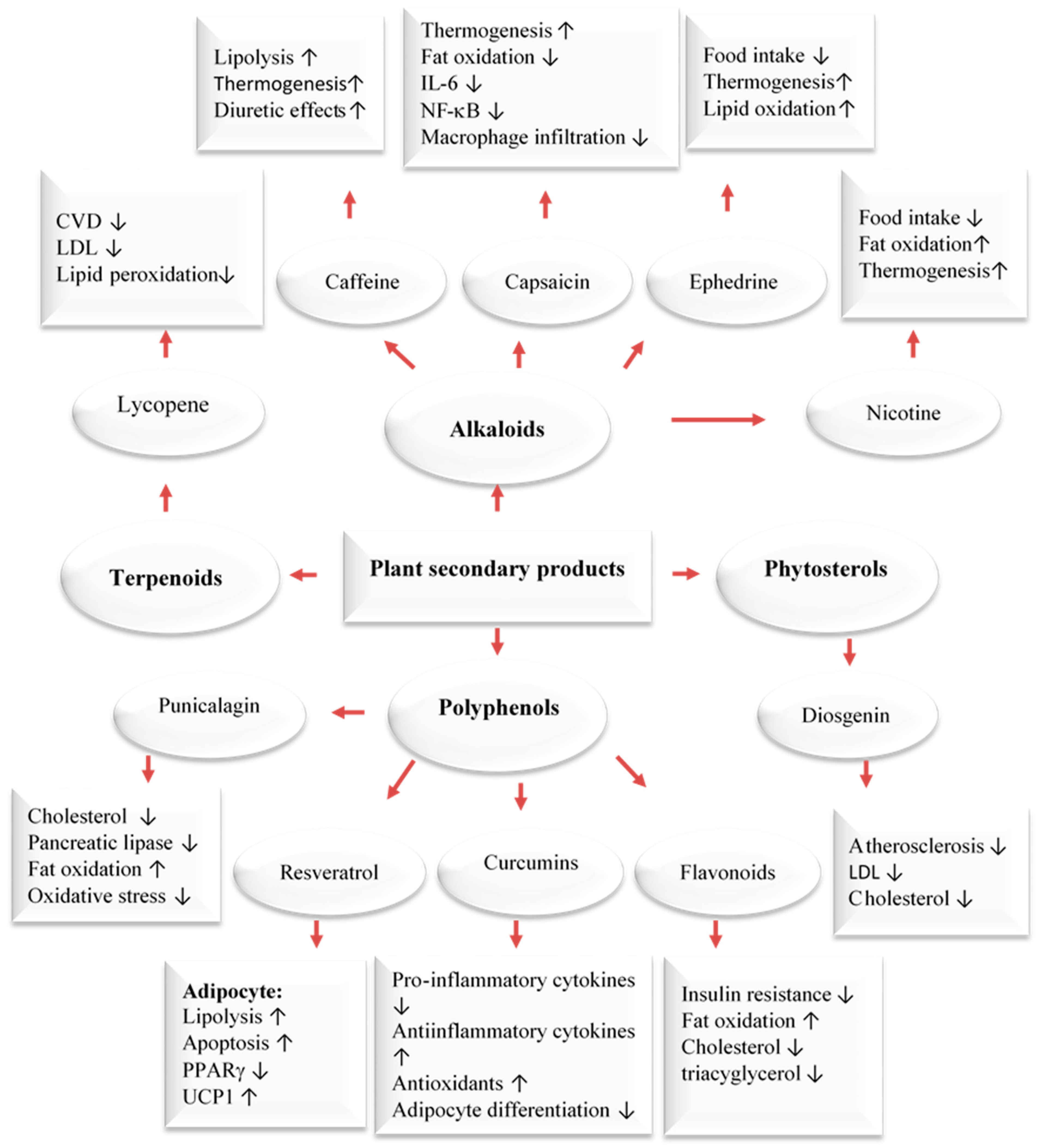
3. Wild Edible Plants and Their Active Compounds
Due to their rich content in plant secondary metabolites, including polyphenols and terpenoids, WEPs are prime candidates for use in nutraceuticals or functional foods. The Mediterranean area is renowned for its abundant variety of WEPs that are edible and form a vital component of this diet. Local communities have long acknowledged the nutritional, protective, and medicinal benefits of these plants, even before their advantages were scientifically validated. In the eastern Mediterranean, WEPs continue to be valued as healthy food sources and are often collected by women as a means of subsistence and income generation in rural areas with limited economic opportunities [40,41,42][38][39][40]. The scientific community has recently shown an increased interest in traditional Arab-Islamic herbal medicine, particularly in its potential for treating metabolic and chronic diseases [38,39][36][37]. This practice, known as Greco-Arab medicine, remains dominant in the Mediterranean region as well as in many Arab and Islamic countries. According to surveys, the Middle East is home to over 2600 species of plants, of which more than 700 are utilized in treating various ailments. Currently, Arab traditional medicine uses fewer than 200–250 plant species to treat various diseases. Many of these species are WEPs that have been assessed in cell culture, in vivo, and in clinical trials and were found to contain pharmacology active compounds [43][41]. WEPs have similar effects as medicinal plants. They can modulate appetite, lipase activity, thermogenesis and fat synthesis and degradation, satiation, adipogenesis, and adipocyte apoptosis. Additionally, targeting adipocyte growth and differentiation with diverse medicinal plants/diet is a significant strategy for devising new anti-obesity drugs that can intervene in preadipocytes, maturing preadipocytes, and mature adipocytes. Many plant extracts from the Mediterranean region and their natural compounds have been tested for their anti-obesity effects in the past ten years [33,34,41][31][35][39]. Specifically, 31 plant species showed the ability to block the pancreatic lipase enzyme. The flavonoid rutin (found in citrus and in a wide range of herbs) and the phenolic acids p-coumaric (found in a wide variety of herbs) and ferulic acids (an antioxidant found in a wide range of plants), which are three bioactive compounds, were found to be successful in blocking this enzyme. It was also shown that trans-anethole and resveratrol, two natural compounds, work by stimulating the brown fat tissue [41][39]. In addition, wild cranberries can influence fat cell formation, and blueberries have shown a remarkable ability to lower blood lipids. In addition, 28 plants from the Mediterranean region and 21 active substances from them have shown promising effects on sugar metabolism. Many studies have examined how plant extracts and pure substances can block digestive enzymes related to obesity and T2D (α-amylase, α-glucosidase, and pancreatic lipase). For example, the effects of 18 WEPs that people eat in southern Italy’s Calabria region on pancreatic lipase, an enzyme that breaks down fats, were tested in a recent study [44,45][42][43]. Nine of the plant extracts could inhibit the enzyme at a concentration of less than 10 mg/mL. The leaves of purslane (Portulaca oleracea) and bladder campion (Silene vulgaris), extracted with water and ethanol, had the strongest inhibition, with 5.48 mg/mL and 6.02 mg/mL needed to block half of the enzyme activity, respectively. Among the plants from the mint family (Lamiaceae), spearmint (Mentha spicata) and rosemary (Rosmarinus officinalis) showed inhibition, with 7.85 mg/mL and 7.00 mg/mL required, respectively. The most effective plants from the sunflower family (Asteraceae) and the cabbage family (Brassicaceae) were common sowthistle (Sonchus oleraceus) (9.75 mg/mL) and perennial wall-rocket (Diplotaxis tenuifolia) (7.76 mg/mL), respectively. Many phytochemicals can help reduce weight by decreasing the absorption of lipids and inhibiting pancreatic lipase. For example, green tea contains catechins and saponins, such as EGCG, which have this effect. Pomegranate (Punica granatum) contains punicalagin, ellagic acid, and anthocyanins; rosemary has rosmarinic acid and carnosic acid; black seed contain thymoquinone; and soybean contains proteins and isoflavones that can also help with weight reduction [33,35][31][32]. However, most of the studies on how plant extracts affect the body were conducted in vitro or on animals. In addition, many new substances and natural products from plants were found to block pancreatic lipase, an enzyme that breaks down fat, better than orlistat, a common drug for weight loss. Some of these extracts have strong effects on fat digestion because of their compounds like polyphenols, saponins, and terpenes. Many natural products that stop pancreatic lipase are being tested on animals or cells, but none of them have been tested on humans yet. Sometimes, it is hard to apply the findings from these tests to clinical use, because they may not work as well in practice. Therefore, the main problem with these studies is that even though many plant chemicals are stronger than orlistat, we do not know how safe they are compared to orlistat. When energy intake consistently exceeds energy expenditure, the excess energy is mostly stored as triglycerides in fat tissue. An increase in adipose tissue mass can result from an increase in cell size, cell number, or both. The cellular pathways that control the growth of pre-adipose cells, adipose differentiation, and lipogenesis in adipocytes were thoroughly investigated [1,3,4][1][3][4] (Figure 4). Recently, the differentiation of pre-adipocytes has garnered research attention and has been investigated through in vitro adipogenesis models, including the 3T3-L1 cell line [46,47,48,49][44][45][46][47]. Many published reports focused on the effects of medicinal plants and their active compounds on adipocyte life cycle. Curcumin (from turmeric), oleuropein (from olive oil), thymoquinone (from black seeds), rosmarinic acid (from rosemary), resveratrol (from grapes), punicalagin (from pomegranate), coumestrol (from soybeans), quercetin (found in many fruits, flowers, and vegetables), Luteolin (found in many fruits, vegetables, and medicinal herbs), and fisetin (found in many fruits and vegetables such as strawberry, apple, and onion) were reported to affect the adipogenesis (Figure 3).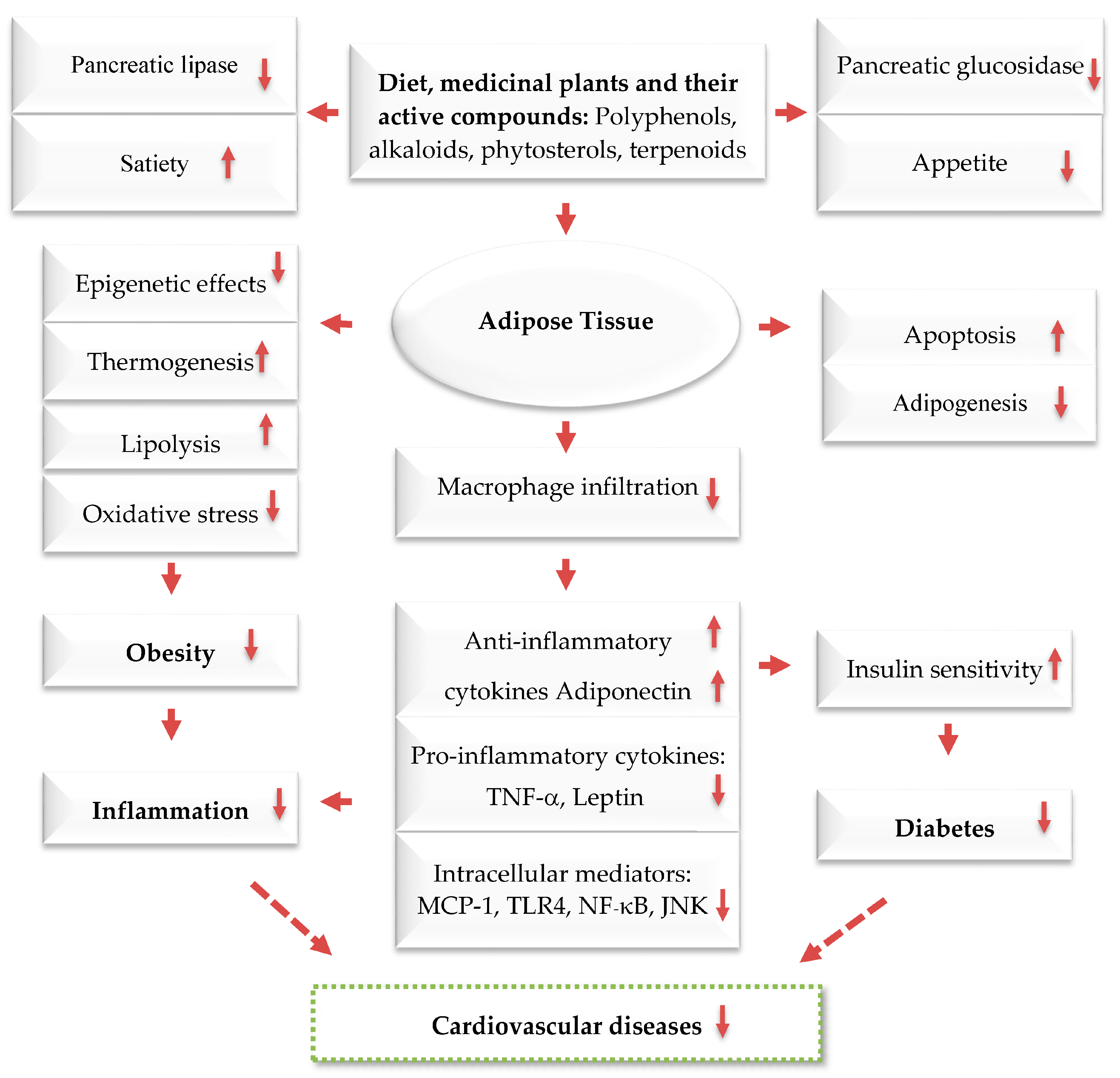
4. The Mediterranean Diet and Its Active Compounds
The main ingredients of the Mediterranean diet (MedDiet) are among the most researched dietary components for treating and preventing various metabolic disorders and CVD. They are recognized for decreasing the risk of CVD, hypertension, T2D, being overweight/obesity, breast and colon cancers, asthma, and mental decline [33,34,50][31][35][48]. The MedDiet, which is rich in antioxidants and has anti-inflammatory, hypotensive, and hypolipidemic properties, is a great alternative to a diet high in red meat for reducing the risk of CVD. Its positive effects are similar to those of standard drugs such as beta-blockers, aspirin, and angiotensin-converting enzyme inhibitors [50,51,52,53,54,55,56][48][49][50][51][52][53][54]. However, it is not yet clear whether these benefits come from individual components of the diet or their combined and synergistic effects [50,51,52,53][48][49][50][51]. There is a lot of evidence that shows a lower risk of mortality from CVD, T2D, specific types of cancer, and cognitive problems when following a MedDiet [53,54][51][52]. A comprehensive review of 27 meta-analyses based on 70 cohort studies found 34 different ways to measure the MedDiet [57][55]. There are various ways to evaluate the MedDiet [58[56][57],59], and all of them involve the common food groups that define this dietary pattern. These include a high intake of fruits, vegetables, nuts, legumes, fish, whole grain cereals, and extra virgin olive oil; a moderate consumption of alcohol, preferably red wine; and a low consumption of dairy products, red meat, and processed meat. Recent meta-analyses of observational studies have consistently shown that following a MedDiet is associated with positive health outcomes [60,61,62][58][59][60]. Critical reviews of both observational studies and RCTs have also confirmed the health benefits of this diet [63,64,65,66][61][62][63][64]. A recent Cochrane review concluded that the evidence supporting the effectiveness of the MedDiet in preventing CVD is only of low to moderate certainty. A recent Cochrane review concluded that the evidence supporting the effectiveness of the MedDiet in preventing CVD is only of low to moderate certainty [63][61]. Nutrition research RCTs are often limited by factors such as small sample sizes, high dropout rates, and short follow-up periods, whereas larger samples, lower dropout rates, and longer follow-up periods are needed to observe patient-relevant outcomes [64][62]. Some discrepancies may arise from the use of varying definitions of the dietary pattern being studied. Inconsistencies may also result from differences in the diets being compared. The health benefits of the MedDiet may be attributed to its impact on the composition and metabolism of the gut microbiota. A systematic review was recently conducted to investigate the effects of this diet on the gut microbiota, as observed in both observational studies and randomized controlled trials. While some research has indicated that a MedDiet may have a positive effect on certain microbiota, a systematic review found that this diet did not consistently alter the composition or metabolism of the microbiota. This inconsistency may be attributed to variations in methodology among studies, particularly in the composition of the MedDiet [65][63].5. The MedDiet and Cardiovascular Disease
A recent long-term RCT (CORDIOPREV study) from Córdoba, Spain, with a 7-year follow-up, compared the effects of the Mediterranean and low-fat diets on the secondary prevention of CVD based on cardiovascular outcomes in patients with coronary heart disease [66][64]. The study involved 1002 patients, with 500 assigned to a low-fat diet group and 502 to a MedDiet group. The primary outcome was a composite of major cardiovascular events, including myocardial infarction, revascularization, ischaemic stroke, peripheral artery disease, and cardiovascular death. The primary endpoint occurred in 198 participants: 87 in the MedDiet group and 111 in the low-fat group. Multivariable-adjusted hazard ratios of the different models ranged from 0.719 to 0.753 in favor of the MedDiet. These effects were more evident in men, with primary endpoints occurring in 16.2% of the men in the MedDiet group versus 22.8% of the men in the low-fat diet group. These data suggest that, in terms of preventing major cardiovascular events in secondary prevention, the MedDiet was more effective than a low-fat diet [66][64].6. Anti-Obesity Effects of MedDiet Polyphenols and Their Possible Mechanisms of Action
The polyphenol rich components of the MedDiet are responsible for the health benefits of this diet. In general, polyphenols are classified into two groups: flavonoids and non-flavonoid polyphenols. Members of both groups can exist in their free form or combined with sugars or acylated sugars (glycosides) or amides, esters, and methyl ethers. Flavonoids include around 6000 different chemicals and are classified into several subgroups [116,117][65][66]. Hydrolysable tannins, lignans, stilbenes, and phenolic acids belong to non-flavonoid polyphenols that have a more complex structure [118,119,120][67][68][69]. Regular consumption of polyphenols is associated with a lower blood pressure and adiposity, an improved lipid profile, as well as antioxidant and anti-inflammatory effects, all of which help protect against CVD [81,121,122][70][71][72]. Polyphenols may contribute to weight loss through several mechanisms. These include promoting satiety, stimulating thermogenesis by activating brown fat, regulating fat tissue by inhibiting fat cell growth and encouraging fat cell apoptosis, and controlling the β-oxidation [123,124,125][73][74][75] (Figure 2). Evidence regarding the impact of polyphenols on obesity and related complications in humans is inconsistent. This is due to variations in study designs, populations, intervention periods, and polyphenol supplements. A systematic review of five RCTs compared the MedDiet with low-fat diets, a low-carbohydrate diet, and the American Diabetes Association (ADA) diet [126][76]. The results show that the MedDiet was more effective for weight loss than low-fat diets but had similar results to the other two interventions. It is unclear if following a traditional MedDiet leads to a reduction in body weight and waist circumference. A meta-analysis of 16 RCTs, however, found that greater adherence to the MedDiet resulted in more weight reduction when compared to a control diet [126,127][76][77]. The MedDiet may promote weight loss due to its high fiber content, low energy density, and low glycemic load. The impact on body weight was more significant when the MedDiet was combined with a calorie-restricted plan or increased physical activity. In T2D patients, the Mediterranean-style diet was found to decrease BMI compared to the control diets [127,128][77][78]. While some clinical trials have found that polyphenol-enriched foods can decrease body fat mass, they have not shown reductions in body weight, BMI, or waist circumference [129][79]. In contrast, a recent study using a polyphenol supplement found significant reductions in these measures. Few studies have investigated the link between total dietary polyphenol intake and weight control. One long-term study found that a higher total polyphenol excretion was associated with a lower BMI, body weight, and waist circumference [130,131,132][80][81][82]. In a 14-year longitudinal study of 4280 participants aged 55–69 in the Netherlands, it was found that women who had a higher intake of flavonoids experienced a lower increase in BMI [133][83].7. Anti-Obesity Effects of Carotenoids and Their Possible Mechanisms of Action
Many studies have found a link between obesity and low levels of carotenoids in the blood [155,156][84][85]. Carotenoids are a type of hydrophobic pigment present in vegetables and fruits, which cannot be synthesized by the human body. Consuming them has been linked to numerous health benefits for humans, including a reduction in overall mortality [157][86]. One of their key characteristics is their ability to affect oxidative stress and inflammation by interacting with transcription factors [158][87]. For instance, they can serve as precursors for bioactive derivatives that activate signaling through nuclear hormone receptors. These derivatives, such as retinoids or vitamin A derived from β-carotene, can activate retinoic acid receptors (RARs), which are a type of nuclear hormone receptor [159][88]. Recent research has led to the discovery of various new metabolic pathways. These pathways are mediated through specific nuclear hormone receptor activation pathways, which were predicted and subsequently confirmed. There is a strong negative correlation between body mass index (BMI) and the levels of all measured carotenoids in the blood. Additionally, many disorders associated with obesity, such as chronic low-grade inflammation and insulin resistance, also show a strong negative correlation with the levels of carotenoids in the blood [160,161,162][89][90][91]. Consuming a diet high in fat can alter the functions of white adipose tissue, which can affect the way AMPK regulates the breakdown of fats and lipid metabolism in fat cells. By activating AMPK, it may be possible to reduce oxidative stress and inflammation. Consuming carotenoids, either through diet or supplements, has been shown to help reduce complications caused by a high-fat diet [163][92]. Different types of carotenoids can stimulate the AMPK signaling pathway, activating enzymes, increasing the activity of transcription factors, promoting the conversion of white adipose tissue to brown, and inhibiting the formation of new fat cells. Carotenoids may also improve the levels of certain “homeostatic” factors, such as adiponectin, which may play a role in activating AMPK. Based on these findings, it is recommended that clinical trials be conducted to confirm the effects of carotenoids on the AMPK pathway in long-term treatments, particularly in cases of obesity [163][92]. Several studies have been conducted to investigate the potential use of carotenoids in managing obesity. However, many of these studies used a combination of carotenoids and vitamins in natural sources, such as fruit juices or plant extracts, making it difficult to determine the specific effects of carotenoids alone [164,165,166][93][94][95]. According to outhe researchers' knowledge, only two clinical trials have been conducted that were randomized, double-blind, placebo-controlled, and investigated the effect of pure carotenoid or xanthophyll supplementation. Canas et al. [167][96] found that children who were given a mixture of carotenoids (including β-carotene, α-carotene, lutein, zeaxanthin, lycopene, astaxanthin, and γ-tocopherol) for 6 months experienced a decrease in their BMI z-score, waist-to-height ratio, and subcutaneous adipose tissue. These positive effects were closely linked to an increase in the concentration of β-carotene in the plasma of children [166][95]. Another study used a combination of paprika xanthophylls and carotenoids, given to healthy overweight volunteers for 12 weeks. This supplementation resulted in a reduction in the visceral fat area, subcutaneous fat area, and total fat area, as well as the BMI in the group that received the treatment compared to a placebo group [166,167,168][95][96][97].References
- Loos, R.J.; Yeo, G.S. The genetics of obesity: From discovery to biology. Nat. Rev. Genet. 2022, 23, 120–133.
- Mohajan, D.; Mohajan, H.K. Obesity and Its Related Diseases: A New Escalating Alarming in Global Health. J. Innov. Med. Res. 2023, 2, 12–23.
- Yang, M.; Liu, S.; Zhang, C. The related metabolic diseases and treatments of obesity. Healthcare 2022, 10, 1616.
- Kajikawa, M.; Higashi, Y. Obesity and Endothelial Function. Biomedicines 2022, 10, 1745.
- Koenen, M.; Hill, M.A.; Cohen, P.; Sowers, J.R. Obesity, Adipose Tissue and Vascular Dysfunction. Circ. Res. 2021, 128, 951–968.
- Higashi, Y.; Noma, K.; Yoshizumi, M.; Kihara, Y. Endothelial function and oxidative stress in cardiovascular diseases. Circ. J. 2009, 73, 411–418.
- Cummings, M.J.; Baldwin, M.R.; Abrams, D.; Jacobson, S.D.; Meyer, B.J.; Balough, E.M.; Aaron, J.G.; Claassen, J.; Rabbani, L.E.; Hastie, J.; et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: A prospective cohort study. Lancet 2020, 395, 1763–1770.
- Zhao, X.; Gang, X.; He, G.; Li, Z.; Lv, Y.; Han, Q.; Wang, G. Obesity increases the severity and mortality of influenza and COVID-19: A systematic review and meta-analysis. Front. Endocrinol. 2020, 11, 595109.
- Lim, H.J.; Xue, H.; Wang, Y. Global trends in obesity. In Handbook of Eating and Drinking: Interdisciplinary Perspectives; Springer: Berlin/Heidelberg, Germany, 2020; pp. 1217–1235.
- ALNohair, S. Obesity in gulf countries. Int. J. Health Sci. 2014, 8, 79.
- Al-Jawaldeh, A.; Taktouk, M.; Nasreddine, L. Food consumption patterns and nutrient intakes of children and adolescents in the Eastern Mediterranean Region: A call for policy action. Nutrients 2020, 12, 3345.
- Colagiuri, S. Diabesity: Therapeutic options. Diabetes Obes. Metab. 2010, 12, 463–473.
- Haslam, D.W.; James, W.P. Obesity. Lancet 2005, 366, 1197–1209.
- Abusalah, M.A.; Albaker, W.; Al-Bsheish, M.; Alsyouf, A.; Al-Mugheed, K.; Issa, M.R.; Alumran, A. Prevalence of type 2 diabetes mellitus in the general population of Saudi Arabia, 2000–2020: A systematic review and meta-analysis of observational studies. Saudi J. Med. Med. Sci. 2023, 11, 1.
- Apovian, C.M.; Okemah, J.; O’Neil, P.M. Body weight considerations in the management of type 2 diabetes. Adv. Ther. 2019, 36, 44–58.
- Narayan, K.M.; Boyle, J.P.; Thompson, T.J.; Gregg, E.W.; Williamson, D.F. Effect of BMI on lifetime risk for diabetes in the U.S. Diabetes Care 2007, 30, 1562–1566.
- Wannamethee, S.G.; Shaper, A.G.; Walker, M. Overweight and obesity and weight change in middle aged men: Impact on cardiovascular disease and diabetes. J. Epidemiol. Community Health 2005, 59, 134–139.
- Hart, C.L.; Hole, D.J.; Lawlor, D.A.; Vey Smith, G. How many cases of type 2 diabetes mellitus are due to being overweight in middle age? Evidence from the Midspan prospective cohort studies using mention of diabetes mellitus on hospital discharge or death records. Diabet Med. 2007, 24, 73–80.
- Klein, S.; Gastaldelli, A.; Yki-Järvinen, H.; Scherer, P.E. Why does obesity cause diabetes? Cell Metab. 2022, 34, 11–20.
- Montague, C.T.; O’Rahilly, S. The perils of portliness: Causes and consequences of visceral adiposity. Diabetes 2000, 49, 883–888.
- Al-Mansoori, L.; Al-Jaber, H.; Prince, M.S.; Elrayess, M.A. Role of inflammatory cytokines, growth factors and adipokines in adipogenesis and insulin resistance. Inflammation 2022, 45, 31–44.
- Chait, A.; Den Hartigh, L.J. Adipose tissue distribution, inflammation and its metabolic consequences, including diabetes and cardiovascular disease. Front. Cardiovasc. Med. 2020, 7, 22.
- Kawai, T.; Autieri, M.V.; Scalia, R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am. J. Physiol.-Cell Physiol. 2021, 320, C375–C391.
- Liu, X.; Zhang, Z.; Song, Y.; Xie, H.; Dong, M. An update on brown adipose tissue and obesity intervention: Function, regulation and therapeutic implications. Front. Endocrinol. 2023, 13, 1065263.
- Maria, V.; Cosetta, R.; Elisabetta, G.; Michela, C.; Andreas, D.F.; Stefania, M. The impact of adipokines on vascular networks in adipose tissue. Cytokine Growth Factor Rev. 2022, 69, 61–72.
- Cypess, A.M. Reassessing Human Adipose Tissue. N. Engl. J. Med. 2022, 386, 768–779.
- Zeyda, M.; Stulnig, T.M. Adipose tissue macrophages. Immunol. Lett. 2007, 112, 61–67.
- Heilbronn, L.K.; Campbell, L.V. Adipose tissue macrophages, low grade inflammation and insulin resistance in human obesity. Curr. Pharm. Des. 2008, 14, 1225–1230.
- Koh-Banerjee, P.; Wang, Y.; Hu, F.B.; Spiegelman, D.; Willett, W.C.; Rimm, E.B. Changes in body weight and body fat distribution as risk factors for clinical diabetes in US men. Am. J. Epidemiol. 2004, 159, 1150–1159.
- Guh, D.P.; Zhang, W.; Bansback, N.; Amarsi, Z.; Birmingham, C.L.; Anis, A.H. The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health 2009, 9, 1–20.
- Saad, B.; Ghareeb, B.; Kmail, A. Metabolic and epigenetics action mechanisms of antiobesity medicinal plants and phytochemicals. Evid.-Based Complement. Altern. Med. 2021, 2021, 1–9.
- Saad, B.; Zaid, H.; Shanak, S.; Kadan, S. Anti-Diabetes and Anti-Obesity Medicinal Plants and Phytochemicals; Springer: Cham, Switzerland, 2017; pp. 59–93.
- Zaid, H.; Saad, B. State of the Art of Diabetes Treatment in Greco-Arab and Islamic Medicine. In Bioactive Food as Dietary Interventions for Diabetes; Watson, R.R., Preedy, V.R., Eds.; Academic Press: San Diego, CA, USA, 2013; pp. 327–337.
- Saad, B.; Said, O. Herbal Medicine. In Greco-Arab and Islamic Herbal Medicine: Traditional System, Ethics, Safety, Efficacy and Regulatory Issues; Wiley-Blackwell John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2011; pp. 47–71.
- Shanak, S.; Saad, B.; Zaid, H. Metabolic and epigenetic action mechanisms of antidiabetic medicinal plants. Evid.-Based Complement. Altern. Med. 2019, 2019, 3583067.
- Saad, B. Greco-Arab and Islamic Herbal Medicine, A Review. Eur. J. Med. Plants 2014, 4, 249–258.
- Saad, B.; Zaid, H.; Shanak, S.; Kadan, S.; Saad, B.; Zaid, H.; Shanak, S.; Kadan, S. Herbal-derived anti-obesity compounds and their action mechanisms. In Anti-Diabetes and Anti-Obesity Medicinal Plants and Phytochemicals: Safety, Efficacy, and Action Mechanisms; Springer: Berlin/Heidelberg, Germany, 2017; pp. 129–144.
- Baydoun, S.; Hani, N.; Nasser, H.; Ulian, T.; Arnold-Apostolides, N. Wild leafy vegetables: A potential source for a traditional Mediterranean food from Lebanon. Front. Sustain. Food Syst. 2023, 6, 991979.
- Marrelli, M.; Statti, G.; Conforti, F. A review of biologically active natural products from Mediterranean wild edible plants: Benefits in the treatment of obesity and its related disorders. Molecules 2020, 25, 649.
- Marouf, M.; Batal, M.; Moledor, S.N.; Talhouk, S. Exploring the practice of traditional wild plant collection in Lebanon. Food Cult. Soc. 2015, 18, 355–378.
- Ceccanti, C.; Landi, M.; Benvenuti, S.; Pardossi, A.; Guidi, L. Mediterranean wild edible plants: Weeds or “new functional crops”? Molecules 2018, 23, 2299.
- Kristanc, L.; Kreft, S. European medicinal and edible plants associated with subacute and chronic toxicity part II: Plants with hepato-, neuro-, nephro-and immunotoxic effects. Food Chem. Toxicol. 2016, 92, 38–49.
- Conforti, F.; Perri, V.; Menichini, F.; Marrelli, M.; Uzunov, D.; Statti, G.A.; Menichini, F. Wild Mediterranean dietary plants as inhibitors of pancreatic lipase. Phytother. Res. 2012, 26, 600–604.
- Ntambi, J.M.; Young-Cheul, K. Adipocyte differentiation and gene expression. J. Nutr. 2000, 130, 3122S–3126S.
- Ruiz-Ojeda, F.J.; Rupérez, A.I.; Gomez-Llorente, C.; Gil, A.; Aguilera, C.M. Cell models and their application for studying adipogenic differentiation in relation to obesity: A review. Int. J. Mol. Sci. 2016, 17, 1040.
- Mansour, B.; Shaheen, N.; Kmail, A.; Haggag, N.; Saad, B. Rosmarinus officinalis L, Eriobotrya japonica and Olea europaea L attenuate adipogenesis in 3T3-L1-derived adipocytes and inflammatory response in LPS-induced THP-1-derived macro-phages. Biointerface Res. Appl. Chem. 2022, 13, 343–360.
- Kmail, A.; Jaradat, N.; Mansour, B.; Abu-Labdeh, R.; Zakarneh, S.; Abu-Farha, S.; Hussein, F.; Issa, L.; Saad, B. Phytochemical analysis, cytostatic, cytotoxic, and anti-inflammatory effects of Arum palaestinum, Ocimum basilicum, and Trigonella foe-num-graecum in human monocytic cell line (THP-1)-derived macrophages. Eur. J. Integr. Med. 2022, 54, 102159.
- Saad, B. Prevention and treatment of obesity-related cardiovascular diseases by diet and medicinal plants. Herb. Med. Back Future 2019, 2, 125–165.
- Vázquez-Ruiz, Z.; Toledo, E.; Vitelli-Storelli, F.; Goni, L.; de la O, V.; Bes-Rastrollo, M.; Martínez-González, M.Á. Effect of dietary phenolic compounds on incidence of cardiovascular disease in the sun project; 10 years of follow-up. Antioxidants 2022, 11, 783.
- Przybylska, S.; Tokarczyk, G. Lycopene in the prevention of cardiovascular diseases. Int. J. Mol. Sci. 2022, 23, 1957.
- Schwingshackl, L.; Morze, J.; Hoffmann, G. Mediterranean diet and health status: Active ingredients and pharmacological mechanisms. Br. J. Pharmacol. 2020, 177, 1241–1257.
- Dinu, M.; Pagliai, G.; Casini, A.; Sofi, F. Mediterranean diet and multiple health outcomes: An umbrella review of meta-analyses of observational studies and randomised trials. Eur. J. Clin. Nutr. 2018, 72, 30–43.
- Martinez-Gonzalez, M.A.; Salas-Salvado, J.; Estruch, R.; Corella, D.; Fito, M.; Ros, E. Benefits of the Mediterranean diet: Insights from the PREDIMED study. Prog. Cardiovasc. Dis. 2015, 58, 50–60.
- Martinez-Gonzalez, M.A.; Gea, A.; Ruiz-Canela, M. The Mediterranean diet and cardiovascular health. Circ. Res. 2019, 124, 779–798.
- Galbete, C.; Schwingshackl, L.; Schwedhelm, C.; Boeing, H.; Schulze, M.B. Evaluating Mediterranean diet and risk of chronic disease in cohort studies: An umbrella review of meta-analyses. Eur. J. Epidemiol. 2018, 33, 909–931.
- Trichopoulou, A.; Costacou, T.; Bamia, C.; Trichopoulos, D. Adherence to a Mediterranean diet and survival in a Greek population. N. Engl. J. Med. 2003, 348, 2599–2608.
- Trichopoulou, A.; Kouris-Blazos, A.; Wahlqvist, M.L.; Gnardellis, C.; Lagiou, P.; Polychronopoulos, E.; Trichopoulos, D. Diet and overall survival in elderly people. BMJ 1995, 311, 1457–1460.
- Chen, G.C.; Neelakantan, N.; Martín-Calvo, N.; Koh, W.P.; Yuan, J.M.; Bonaccio, M.; Iacoviello, L.; Martínez-González, M.A.; Qin, L.Q.; van Dam, R.M. Adherence to the Mediterranean diet and risk of stroke and stroke subtypes. Eur. J. Epidemiol. 2019, 34, 337–349.
- Kojima, G.; Avgerinou, C.; Iliffe, S.; Walters, K. Adherence to Mediterranean diet reduces incident frailty risk: Systematic review and meta-analysis. J. Am. Geriatr. Soc. 2018, 66, 783–788.
- Shafiei, F.; Salari-Moghaddam, A.; Larijani, B.; Esmaillzadeh, A. Adherence to the Mediterranean diet and risk of depression: A systematic review and updated meta-analysis of observational studies. Nutr. Rev. 2019, 77, 230–239.
- Rees, K.; Takeda, A.; Martin, N.; Ellis, L.; Wijesekara, D.; Vepa, A.; Stranges, S. Mediterranean-style diet for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst. Rev. 2019, 3, Cd009825.
- Satija, A.; Yu, E.; Willett, W.C.; Hu, F.B. Understanding nutritional epidemiology and its role in policy. Adv. Nutr. 2015, 6, 5–18.
- Kimble, R.; Gouinguenet, P.; Ashor, A.; Stewart, C.; Deighton, K.; Matu, J.; Griffiths, A.; Malcomson, F.C.; Joel, A.; Houghton, D.; et al. Effects of a mediterranean diet on the gut microbiota and microbial metabolites: A systematic review of randomized controlled trials and observational studies. Crit. Rev. Food Sci. Nutr. 2022, 1–22.
- Delgado-Lista, J.; Alcala-Diaz, J.F.; Torres-Peña, J.D.; Quintana-Navarro, G.M.; Fuentes, F.; Garcia-Rios, A.; Ortiz-Morales, A.M.; Gonzalez-Requero, A.I.; Perez-Caballero, A.I.; Yubero-Serrano, E.M.; et al. Long-term secondary prevention of cardiovascular disease with a Mediterranean diet and a low-fat diet (CORDIOPREV): A randomised controlled trial. Lancet 2022, 399, 1876–1885.
- Chu, A.J. Quarter-century explorations of bioactive polyphenols: Diverse health benefits. Front. Biosci.-Landmark 2022, 27, 134.
- Rana, A.; Samtiya, M.; Dhewa, T.; Mishra, V.; Aluko, R.E. Health benefits of polyphenols: A concise review. J. Food Biochem. 2022, 46, e14264.
- Scalbert, A.; Manach, C.; Morand, C.; Remesy, C.; Jimenez, L. Dietary polyphenols and the prevention of diseases. Crit. Rev. Food Sci. Nutr. 2005, 45, 287–306.
- Pereira, D.M.; Valentão, P.; Pereira, J.A.; Andrade, P.B. Phenolics: From chemistry to biology. Molecules 2009, 14, 2202–2211.
- Pandey, K.B.; Rizvi, S.I. Plant polyphenols as dietary antioxidants in human health and disease. Oxid. Med. Cell. Longev. 2009, 2, 270–278.
- Castro-Barquero, S.; Lamuela-Raventós, R.M.; Doménech, M.; Estruch, R. Relationship between Mediterranean dietary polyphenol intake and obesity. Nutrients 2018, 10, 1523.
- Phenol-Explorer, An Online Comprehensive Database on Polyphenol Contents in Foods. 2010. Available online: http://www.phenol-explorer.eu (accessed on 21 September 2018).
- Tresserra-Rimbau, A.; Rimm, E.B.; Medina-Remon, A.; Martinez-Gonzalez, M.A.; dela Torre, R.; Corella, D.; Salas-Salvador, J.; Gómez-Garcia, E.; Lapetra, J.; Arós, F.; et al. Inverse association between habitual polyphenol intake and incidence of cardiovascular events in the PREDIMED study. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 639–647.
- Rupasinghe, H.P.V.; Sekhon-Loodu, S.; Mantso, T.; Panayiotidis, M.I. Phytochemicals in regulating fatty acids β-oxidation: Potential underlying mechanisms and their involvement in obesity and weight loss. Pharmacol. Ther. 2016, 165, 153–163.
- Cox, L.M.; Blaser, M.J. Pathways in microbe-induced obesity. Cell Met. 2013, 17, 883–894.
- Wang, Z.; Wang, Q.A.; Liu, Y.; Jiang, L. Energy metabolism in brown adipose tissue. FEBS J. 2021, 288, 3647–3662.
- Mancini, J.G.; Filion, K.B.; Atallah, R.; Eisenberg, M.J. Systematic Review of the Mediterranean Diet for Long-Term Weight Loss. Am. J. Med. 2016, 129, 407–415.
- Huo, R.; Du, T.; Xu, Y.; Xu, W.; Chen, X.; Sun, K.; Yu, X. Effects of Mediterranean-style diet on glycemic control, weight loss and cardiovascular risk factors among type 2 diabetes individuals: A meta-analysis. Eur. J. Clin. Nutr. 2015, 69, 1200–1208.
- Tricò, D.; Moriconi, D.; Berta, R.; Baldi, S.; Quinones-Galvan, A.; Guiducci, L.; Taddei, S.; Mari, A.; Nannipieri, M. Effects of low-carbohydrate versus mediterranean diets on weight loss, glucose metabolism, insulin kinetics and β-cell function in morbidly obese individuals. Nutrients 2021, 13, 1345.
- Barth, S.W.; Koch, T.C.L.; Watzl, B.; Dietrich, H.; Will, F.; Bub, A. Moderate effects of apple juice consumption on obesity-related markers in obese men: Impact of diet-gene interaction on body fat content. Eur. J. Nutr. 2012, 51, 841–850.
- Cases, J.; Romain, C.; Dallas, C.; Gerbi, A.; Cloarec, M. Regular consumption of Fiit-ns, a polyphenol extract from fruit and vegetables frequently consumed within the Mediterranean diet, improves metabolic ageing of obese volunteers: A. randomized, double-blind, parallel trial. Int. J. Food. Sci. Nutr. 2015, 66, 120–125.
- Guo, X.; Tresserra-Rimbau, A.; Estruch, R.; Martinez-Gonzalez, M.A.; Medina-Remon, A.; Fitó, M.; Corella, D.; Salas-Salvadó, J.; Portillo, M.P.; Moreno, J.J.; et al. Polyphenol levels are inversely correlated with body weight and obesity in an elderly population after 5 years of follow up (The Randomised PREDIMED Study). Nutrients 2017, 9, 452.
- Marranzano, M.; Ray, S.; Godos, J.; Galvano, F. Association between dietary flavonoids intake and obesity in a cohort of adults living in the Mediterranean area. Int. J. Food Sci. Nutr. 2018, 26, 1–10.
- Wang, S.; Moustaid-Moussa, N.; Chen, L.; Mo, H.; Shastri, A.; Su, R.; Bapat, P.; Kwun, I.; Shen, C.L. Novel insights of dietary polyphenols and obesity. J. Nutr. Biochem. 2014, 25, 1–18.
- Kennedy, D.O. Polyphenols and the Human Brain: Plant “Secondary Metabolite” Ecologic Roles and Endogenous Signaling Functions Drive Benefits. Adv. Nutr. 2014, 5, 515–533.
- Kapolou, A.; Karantonis, H.C.; Rigopoulos, N.; Koutelidakis, A.E. Association of mean daily polyphenols intake with Mediterranean diet adherence and anthropometric indices in healthy Greek adults: A retrospective study. Appl. Sci. 2021, 11, 4664.
- Kimmons, J.E.; Blanck, H.M.; Tohill, B.C.; Zhang, J.; Khan, L.K. Associations between body mass index and the prevalence of low micronutrient levels among US adults. MedGenMed 2006, 8, 59.
- Garcia, O.P.; Long, K.Z.; Rosado, J.L. Impact of micronutrient deficiencies on obesity. Nutr. Rev. 2009, 67, 559–572.
- Von Lintig, J. Colors with functions: Elucidating the biochemical and molecular basis of carotenoid metabolism. Annu. Rev. Nutr. 2010, 30, 35–56.
- Bohn, T.; de Lera, A.R.; Landrier, J.F.; Carlsen, H.; Merk, D.; Todt, T.; Renaut, J.; Rühl, R. State-of-the-art methodological investigation of carotenoid activity and metabolism–from organic synthesis via metabolism to biological activity–exemplified by a novel retinoid signalling pathway. Food Funct. 2023, 14, 621–638.
- Andersen, L.F.; Jacobs, D.R., Jr.; Gross, M.D.; Schreiner, P.J.; Dale Williams, O.; Lee, D.H. Longitudinal associations between body mass index and serum carotenoids: The CARDIA study. Br. J. Nutr. 2006, 95, 358–365.
- Calder, P.C.; Ahluwalia, N.; Brouns, F.; Buetler, T.; Clement, K.; Cunningham, K.; Esposito, K.; Jonsson, L.S.; Kolb, H.; Lansink, M.; et al. Dietary factors and low-grade inflammation in relation to overweight and obesity. Br. J. Nutr. 2011, 106, S5–S78.
- Beydoun, M.A.; Shroff, M.R.; Chen, X.; Beydoun, H.A.; Wang, Y.; Zonderman, A.B. Serum antioxidant status is associated with metabolic syndrome among U.S. adults in recent national surveys. J. Nutr. 2011, 141, 903–913.
- Beydoun, M.A.; Chen, X.; Jha, K.; Beydoun, H.A.; Zonderman, A.B.; Canas, J.A. Carotenoids, vitamin A, and their association with the metabolic syndrome: A systematic review and meta-analysis. Nutr. Rev. 2019, 77, 32–45.
- Ferreira, Y.Y.; Jamar, G.; Estadella, D.; Pisani, L.P. Role of Carotenoids in Adipose Tissue trough AMPK-mediated Pathway. Food Funct. 2023, 14, 3454–3462.
- Bonet, M.L.; Canas, J.A.; Ribot, J.; Palou, A. Carotenoids and their conversion products in the control of adipocyte function, adiposity and obesity. Arch. Biochem. Biophys. 2015, 572, 112–125.
- Canas, J.A.; Lochrie, A.; McGowan, A.G.; Hossain, J.; Schettino, C.; Balagopal, P.B. Effects of Mixed Carotenoids on Adipokines and Abdominal Adiposity in Children: A Pilot Study. J. Clin. Endocrinol. Metab. 2017, 102, 1983–1990.
- Kakutani, R.; Hokari, S.; Nishino, A.; Ichihara, T.; Sugimoto, K.; Takaha, T.; Kuriki, T.; Maoka, T. Effect of Oral Paprika Xanthophyll Intake on Abdominal Fat in Healthy Overweight Humans: A Randomized, Double-blind, Placebo-controlled Study. J. Oleo Sci. 2018, 67, 1149–1162.
