Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Hamayak Sisakian and Version 2 by Dean Liu.
Heart failure with reduced ejection fraction (HFrEF) is considered a major health care problem with frequent decompensations, high hospitalization and mortality rates. In severe heart failure (HF), the symptoms are refractory to medical treatment and require advanced therapeutic strategies. Early recognition of HF sub- and decompensation is the cornerstone of the timely treatment intensification and, therefore, improvement in the prognosis. Echocardiography is the gold standard for the assessment of systolic and diastolic functions. It allows one to obtain accurate and non-invasive measurements of the ventricular function in HF.
- heart failure with reduced ejection fraction
- echocardiography
- outpatient monitoring
- left ventricular filling pressure
1. Introduction
Heart failure (HF) is considered a major health care problem with more than a million new cases every year [1]. Over the last few decades, guideline-recommended treatment has considerably improved the outcomes of heart failure with reduced ejection fraction (HFrEF) [2][3][2,3]. Despite this, the mortality and rehospitalization rates remain high [1][2][4][5][1,2,4,5]. Moreover, the number of hospitalizations for HF is expected to increase significantly in the future and may double by 2045 due to the aging and growth of the population [6][7][6,7].
HF decompensation may be provoked by trigger factors such as infection, myocardial ischemia, acute renal injury, or anemia. In the case of disease deterioration due to increasing fluid retention, subclinical congestion precedes the clinical manifestation of HF symptoms and hospitalizations for an acute HF decompensation by several days or weeks. Therefore, the identification of a vulnerable period before the symptomatic HF decompensation allows for a prompt increase in diuretic doses and treatment modification, which may prevent the upcoming hospital admission [8]. Physical examination, particularly the identification of crackles on auscultation, is the main strategy routinely used for the prediction and diagnosis of left-sided HF decompensation in outpatients [9]. However, while it allows for the identification of symptomatic patients, the asymptomatic phase of HF decompensation is usually missed.
Hospitalization negatively affects the prognosis and quality of life [10]. Moreover, it is strongly associated with a risk of cardiovascular and all-cause mortality, which increases progressively with every subsequent hospitalization [11]. Thus, the prevention of rehospitalization is one of the main goals of HF management. For an effective reduction in unexpected hospital visits, early prediction of HF decompensation and prompt treatment modification are of paramount importance. Effective ambulatory monitoring and timely treatment modification are the key strategies for the reduction in cardiovascular events and improvement in the prognosis [12]. Numerous data suggest that HF patients who have undergone an echocardiographic examination have better survival rates due to more intensive medical treatment and interventions [13].
2. Left Ventricular Decompensation: Natriuretic Peptides and Basic Echocardiography
It is evident that hemodynamic deterioration precedes the development of clinical signs and symptoms by days or weeks, thus symptomatic clinical congestion may be seen as the “tip of an iceberg” of hemodynamic compromise [14]. Due to the delay between symptom manifestation and the progressive left ventricular (LV) filling pressure increase, physical examination alone may be insufficient for the identification of patients in the vulnerable phase of asymptomatic decompensation and for the prediction of upcoming hospital readmissions in outpatients [15][16][15,16]. It is well-established that an increased venous pressure can be detected by cardiovascular ultrasound, particularly by the assessment of inferior vena cava (IVC) characteristics and the detection of interstitial pulmonary edema through B-line identification. On the other hand, intracardiac hemodynamic changes and LV filling pressure increase precede the manifestation of HF symptoms and can be diagnosed by echocardiography [12][17][12,17]. Comprehensive cardiovascular ultrasound with tissue Doppler imaging (TDI) and lung ultrasound overcome the limitations of physical examination and clinical picture-based strategies for the prediction of HF decompensation. Over the last decade, it has become apparent that natriuretic peptide-guided management of ambulatory chronic HF patients may optimize the treatment. Natriuretic peptides are important components of HF diagnostic work-up due to their high negative predictive value. However, the data on the utility of natriuretic peptides in the prevention of HF decompensations are relatively scarce. In the PARADIGM-HF trial, low levels of natriuretic peptides were associated with lower risks of cardiovascular events [18]. In the GUIDE-IT study involving 894 high risk patients with HFrEF, the most important predictor of cardiovascular death and HF hospitalizations was the baseline natriuretic peptide level [19]. The data suggest that natriuretic peptides also correlate with the risk of hospitalization and the duration of hospital stay [6]. However, with the introduction of a neprilysin inhibitor in the treatment of HFrEF, the accuracy and reliability of natriuretic peptides as prognostic markers have been questioned. By inhibiting neprilysin, sacubitril leads to an increase in B-type natriuretic peptide (BNP) and a reduction in the N-terminal pro-B-type natriuretic peptide (NT-proBNP) concentrations [20]. Thus, the role of natriuretic peptides in the prediction of hospital admissions in outpatients has to be further investigated. Another concern regarding the diagnostic role of natriuretic peptides is related to morbidly obese patients, who have consistently lower natriuretic peptide levels [21][22][23][21,22,23]. Other limitations of natriuretic peptides include their level changes in atrial fibrillation and renal dysfunction. Given the limitations of natriuretic peptides, along with the complex physiology of HF, it is reasonable to consider the implementation of other parameters and markers for the improvement of HF management and the prevention of decompensation. Basic echocardiographic assessment is an important tool for the diagnosis, classification, and treatment of HF. Some authors recommend using LV ejection fraction (EF) for the assessment of prognosis in ambulatory HFrEF patients, based on the role of EF dynamic increase as a predictor marker of an improved survival and hospitalization risk in this patient population [24]. However, EF loses its prognostic role at later stages of the disease and when the values are close to the threshold [25]. As a prognostic marker for HF decompensations, EF has other important limitations. Among them, technical pitfalls, preload dependence, possible measurement errors in the presence of severe mitral regurgitation, atrial fibrillation or heart rate variations, and a weak association with functional class and exercise capacity [26][27][28][26,27,28]. The above-mentioned limitations advocate for the use of additional parameters and methods for the assessment of LV function such as TDI, longitudinal strain quantification by speckle tracking, 3-dimensional echocardiography, and cardiac magnetic resonance imaging (MRI). An increase in left atrial (LA) volume and LV filling pressure contribute to LA remodeling and HF decompensation, leading to frequent hospitalization due to the lung congestion. In clinical practice, the LA volume index is widely used to assess LA overload. A clinically significant increase is considered an LA volume index >34 mL/m2 [29]. The LA volume index is an independent predictor of cardiovascular events including atrial fibrillation as well as cardiovascular mortality [26][30][26,30]. Moreover, the LA volume index is a marker of diastolic dysfunction and, unlike EF, correlates well with the patient’s functional class and overall exercise capacity [27][31][27,31]. The LA volume index correlates with the E/e’ ratio and can serve as a useful predictor of increased LV filling pressure during exercise [32]. Echocardiography with intracardiac hemodynamic assessment provides a semiquantitative analysis of decompensation and identifies filling pressure abnormalities. LV filling pressure measurements are of special interest in patients with HFrEF because the increase in filling pressure underlines the pathophysiological mechanisms of HF deterioration and precedes the manifestation of HF signs and symptoms [12]. Currently, echocardiographic Doppler and TDI are widely used in clinical practice for the evaluation of LV systolic and diastolic functions. As a marker of diastolic dysfunction, LV filling pressure can be assessed by calculating the E/e’ ratio, where the E wave is the peak velocity of the early diastolic flow across the mitral valve, as measured by pulsed-wave Doppler, and e’ is the early diastolic velocity of the septal or lateral mitral annulus obtained by TDI (Figure 1). The accepted threshold for the normal LV end-diastolic pressure is E/e’ <8, while E/e’ >14 and peak tricuspid regurgitation (TR) velocity >2.8 m/s indicate high LV end-diastolic pressure [33]. Recent studies emphasize the importance of the routine measurements of E/e’ for the assessment of LV filling pressure, risk stratification, and prognostication in the HF patient population [33][34][33,34]. Benfari G. et al. suggested an E/e’ ratio >14 as a cut-off for the identification of high-risk patients [35]. The authors reported increased short- and long-term mortality in individuals with E/e’ >14, with a considerable worsening of prognosis in E/e’ >20 [35]. Therefore, in HFrEF, additional parameters should be considered for the assessment of LV filling pressures and atrial hypertension to predict intracardiac volume overload and subclinical deterioration.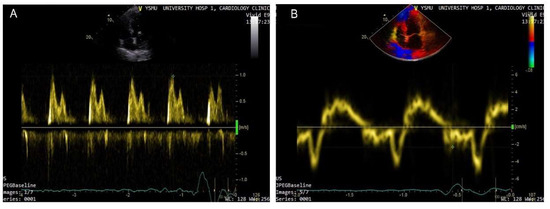
Figure 1. Doppler-based assessment of LV filling pressure. Raised filling pressure based on increased E/e’ ratio derived from the spectral Doppler of transmitral flow early peak velocity (E wave) (arrow) (A) and tissue Doppler of the mitral annular displacement early diastolic peak velocity (e’ wave) (arrow head) (B); E/e’ > 15.
