Advancements in modern medicine have bolstered the usage of home-based rehabilitation services for patients, particularly those recovering from diseases or conditions that necessitate a structured rehabilitation process. Understanding the technological factors that can influence the efficacy of home-based rehabilitation is crucial for optimizing patient outcomes. As technologies continue to evolve rapidly, it is imperative to document the current state-of-the-art and elucidate the key features of the hardware and software employed in these rehabilitation systems. This narrative review aims to provide a summary of the modern technological trends and advancements in home-based shoulder rehabilitation scenarios. It specifically focuses on wearable devices, robots, exoskeletons, Machine Learning, virtual and augmented reality, and serious games. Through an in-depth analysis of existing literature and research, this review presents the state-of-the-art in home-based rehabilitation systems, highlighting their strengths and limitations. Furthermore, this review proposes hypotheses and potential directions for future upgrades and enhancements in these technologies. By exploring the integration of these technologies into home-based rehabilitation, this review aims to shed light on the current landscape and offer insights into the future possibilities for improving patient outcomes and optimizing the effectiveness of home-based rehabilitation programs.
- home-based rehabilitation
- wearables
- robots
- exoskeletons
1. Introduction
2. Technology Solutions for Home-Based Shoulder Rehabilitation
In the realm of medical advancements, numerous devices are currently under development, with many designed for use in clinical or hospital settings due to their inherent complexity. However, certain devices and technologies offer relative simplicity in their operation, making them well suited for home use and enabling patients to regain autonomy and independence in their rehabilitation journey [16][20]. Figure 1 presents an overview of these key technologies, categorized into the domains of physical and virtual applications, each playing a significant role in home-based rehabilitation. By exploring these technologies, rwesearchers c can better understand their potential impact and effectiveness in supporting patients’ rehabilitation progress.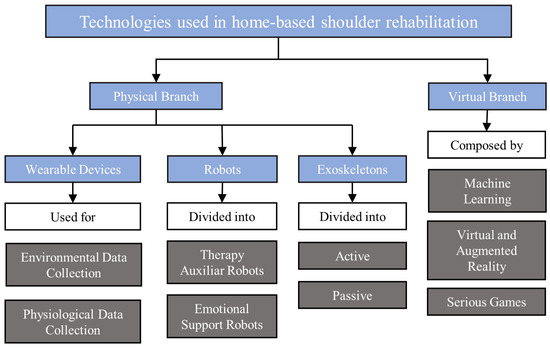
3. Considerations for Therapeutic Exercises in Home-Based Rehabilitation
Enhancing shoulder functionality through physical rehabilitation is a crucial aspect of achieving effective recovery following injury or surgery. This process entails engaging in appropriate rehabilitation exercises, which target various movement planes to enhance motor function [48][90]. By providing targeted stimuli, these exercises contribute to the improvement of patient fitness and functional ability, enabling them to achieve positive outcomes even when undertaking home-based rehabilitation or self-management without direct supervision from a healthcare professional [49][91].4. Guidelines for Home-Based Rehabilitation Systems
Developing effective home-based rehabilitation systems requires adherence to specific guidelines to ensure optimal user experience, safety, and positive rehabilitation outcomes. Below, rwesearchers propose a set of guidelines, which should be followed during the development process:-
User-centric design: Prioritize user needs and preferences when designing the system interface. Create an intuitive and user-friendly interface, which accommodates individuals with varying technological proficiency, ensuring easy navigation and engagement during home-based rehabilitation sessions.
-
Accessibility and inclusivity: Ensure that the system is accessible to a diverse range of users, including those with physical disabilities, visual impairments, and cognitive limitations. Incorporate features such as adjustable font sizes, voice guidance, and alternative input methods to enhance accessibility for all patients.
-
Customization and adaptability: Provide options for customization and adaptation of the system to meet individual patients’ specific needs. Allow for adjustments in difficulty levels, exercise intensity, and duration based on the patient’s progress and capabilities.
-
Equity and accessibility: It is important to consider the equitable access and availability of home-based rehabilitation systems to ensure that all individuals, regardless of socioeconomic status or geographical location, have equal opportunities for rehabilitation and benefit from the technology.Real-time feedback and guidance: Incorporate mechanisms to provide real-time feedback and guidance during exercises. Utilize visual cues, auditory signals, or haptic feedback to help patients perform exercises correctly and optimize their rehabilitation progress.
-
User autonomy and empowerment: Home-based rehabilitation systems should be designed to empower patients and promote their active involvement in their own care. The technology should support patient autonomy, allowing them to make informed decisions about their treatment and providing them with tools for self-management.Comprehensive progress tracking: Develop a robust system for tracking and recording patients’ progress over time. Monitor metrics such as exercise completion rates, duration, intensity, and improvements in performance. Utilize these data to personalize future exercise plans and set realistic goals for patients.
-
Safety measures and risk mitigation: Prioritize patient safety by integrating safety measures into the system. Use technologies such as motion sensors to detect incorrect movements or provide warnings when patients exceed safe ranges of motion. Implement risk mitigation strategies to prevent injury during exercises.
-
Transparent and explainable AI: If machine-learning algorithms are integrated into the rehabilitation systems, there is a need for transparency and explainability. Patients should have a clear understanding of how AI is being used, what factors influence treatment recommendations, and the basis for any decisions made by the system.Data privacy and security: Ensure that the system complies with data privacy regulations and incorporates robust security measures to protect patient information. Implement measures to safeguard sensitive data and provide patients with control over their data and their usage.
-
Clinical oversight and human interaction: While home-based rehabilitation systems offer the advantage of remote monitoring and independent practice, it is essential to maintain a balance between technology-driven interventions and the involvement of healthcare professionals. Regular clinical oversight and human interaction should be incorporated into the system to ensure patient safety, address individual needs, and provide timely support or intervention when required.Seamless integration with healthcare professionals: Enable seamless communication and data exchange between the home-based rehabilitation system and healthcare professionals involved in the patients’ care. Facilitate remote monitoring, feedback, and the ability to make informed adjustments to the rehabilitation program based on professional expertise.
-
Artificial intelligence and machine-learning integration: Explore opportunities to integrate artificial intelligence or machine-learning algorithms into the home-based rehabilitation system. Leverage artificial intelligence capabilities to analyze patient data, identify patterns, and provide personalized recommendations for exercise progression, adapting the rehabilitation program based on individual needs and response to treatment.
-
Scalability and compatibility: Design the system to be scalable and compatible with various devices and platforms. Accommodate different technologies and future advancements, ensuring flexibility and long-term viability of the home-based rehabilitation system.
4.1. Ethical Concerns
As technology continues to advance in the field of home-based rehabilitation systems, it is crucial to address the ethical considerations associated with their use. The following ethical concerns should be taken into account when developing and implementing such systems:-
Privacy and data security: Home-based rehabilitation systems often involve the collection and storage of sensitive personal health information. It is essential to ensure that robust data protection measures are in place to safeguard patient privacy and prevent unauthorized access or misuse of the data.
-
Informed consent: Patients participating in home-based rehabilitation programs should be adequately informed about the purpose, risks, benefits, and potential limitations of the technology being used. Informed consent should be obtained, outlining the scope of data collection, potential risks, and the patient’s right to withdraw from the program at any time.
