You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is a comparison between Version 2 by Camila Xu and Version 1 by Carmine Izzo.
Obesity is defined when the body mass index (BMI) exceeds a value of 30 kg/m2. It is implicated in slowing improved life expectancy and increasing cardiovascular (CV) risk.
- obesity
- cardiovascular risk
- cardiometabolic complications
- lifestyle interventions
1. Introduction
Obesity is defined when the body mass index (BMI) exceeds a value of 30 kg/m2 [1]. This condition is a growing public health epidemic across the world. Accordingly, the available data suggest that the global burden of obesity has more than tripled since 1975 [2], not only in first-world countries; indeed, recent evidence shows that obesity is spreading in low-and middle-income countries [3]. Specifically, around 42% of adults in the US are obese, while prevalence has increased to about 25% in the United Kingdom [4]. Italy follows this trend with an increase of almost 30% in the adult obese population in the last three decades [5].
2. Relationship between Obesity and Cardiovascular Disease
Obesity is a multifactorial condition influenced by a range of social and environmental factors. While individual behaviors, such as diet and physical activity, play a role in obesity development, broader determinants related to society and the environment also significantly contribute.
The social and environmental determinants of obesity include various aspects.
First, lower socioeconomic status is associated with a higher prevalence of obesity. Factors such as limited access to healthy food options, higher levels of food insecurity, and reduced opportunities for physical activity contribute to the higher obesity rates observed in disadvantaged populations. Socioeconomic disparities can influence dietary choices, availability of resources, and overall health-related behaviors [6].
Another important factor includes the food environment, which consists of the availability and accessibility to healthy food options in communities. Areas characterized by a high density of fast-food outlets, limited access to grocery stores offering fresh produce, and a lack of affordable healthy food options are associated with higher obesity rates. These “food deserts” make it challenging for individuals to make nutritious choices, leading to a higher consumption of energy-dense, nutrient-poor foods [7,8][7][8].
Cultural norms and social norms influence and play a role in shaping dietary preferences and behaviors. Societal norms that prioritize large portion sizes, frequent consumption of high-calorie foods, and sedentary lifestyles can contribute to the development of obesity. Additionally, social networks and peer influence can impact food choices and physical activity patterns [9].
Limited education and low health literacy levels can hinder individuals’ understanding of nutrition and the importance of a healthy lifestyle. Insufficient knowledge about healthy food choices, portion sizes, and the benefits of regular physical activity can contribute to obesity. Educational interventions and improving health literacy can empower individuals to make informed decisions and adopt healthier behaviors [10].
Environmental determinants of obesity include the built environment, such as the design and layout of neighborhoods and urban spaces that can affect physical activity levels. Accessible sidewalks, bike lanes, parks, and recreational facilities can promote active lifestyles. Conversely, neighborhoods lacking these features, characterized by limited safety and opportunities for physical activity, can discourage exercise and contribute to sedentary behaviors [11].
Moreover, transportation infrastructure in terms of availability and quality of public transportation systems influence physical activity levels. Communities with inadequate public transportation options may rely more on sedentary modes of transportation, such as cars, leading to reduced opportunities for physical activity [12].
In modern society, advertising and marketing and, in particular, aggressive marketing of unhealthy foods, especially towards children, can contribute to poor dietary choices and increased consumption of energy-dense foods. Exposure to advertisements promoting sugary beverages, fast food, and unhealthy snacks can influence eating behaviors and contribute to obesity [13].
Finally, the work environment, including occupational factors, such as sedentary work environments and long working hours, can limit opportunities for physical activity and contribute to a sedentary lifestyle. Workplace policies and environments that promote physical activity, such as standing desks or workplace wellness programs, can help mitigate the impact of sedentary jobs [14].
Obesity is implicated in recent slowing in improved life expectancy [15] and increases the risk of several chronic diseases (diabetes, hypertension, coronary heart disease) [16,17,18,19][16][17][18][19]. On average, in the populations studied (largely Caucasians), obesity class III (BMI ≥ 40 kg/m2) shortens life expectancy by approximately 10 years, and obesity class I (BMI 30–34.9 kg/m2) reduces life duration by around 3 years, relative to normal weight, with the number of years lost varying according to age, sex, and severity of obesity [1,20,21][1][20][21]. Specifically, the metabolic syndrome, a concurrence of disturbed glucose and insulin metabolism, overweight and abdominal fat distribution, mild dyslipidemia, and hypertension, is most important because of its association with cardiovascular disease (CVD) [22,23][22][23]. More precisely, CV risk is high/very high with obesity class I, very high with class II, and extremely high with class III in Caucasian populations [1]. However, BMI indicates the overall excess body weight, while waist circumference better defines fat distribution and abdominal body fat [24,25][24][25]. Additionally, BMI is inadequate for defining body composition and the difference between fat mass and fat-free mass; specifically, the CV risk differs according to the type of ectopic deposition [1,24,26,27][1][24][26][27]. Specifically, the distribution of adipose tissue has clinical importance, because central adiposity, especially visceral obesity, is more deleterious, while lower body fat deposition may be actually protective [28]. However, the implementation of fat distribution assessment in clinical practice remains a challenge: the instruments used have a high acquisition cost and specialized professionals are needed to use them [29].
Genetic and population-based cohort analysis has revealed a direct relationship between adiposity and other high-risk CV traits, including aortic diseases, HF, deep vein thrombosis, hypertensive heart disease, peripheral artery diseases, and atrial fibrillation (AF) [26,30][26][30]. Indeed, several obesity-related mechanisms drive structural, functional, humoral, and hemodynamic alterations believed to underpin the development of CVD (Figure 1) [1]. Specifically, there is a causal association between adipose tissue and CVD: obesity is the causal pathway of several traditional CV risk factors such as atherogenic dyslipidemia, hypertension and diabetes; moreover, obesity-related OSA contributes to CVD risk with the promotion of hypoxia, cardiac dysrhythmias, insulin resistance, and hypertension [31,32,33,34][31][32][33][34]. Obesity often leads to a deterioration of adipose tissue plasticity, which is linked to fibrosis, inflammation, progenitor cell senescence, and catecholamine resistance [35]. On the other hand, obesity may indirectly cause CVD, mediated through different obesity-associated comorbidities: an excessive increase in body weight prejudices mobility and physical activity and/or worsens musculoskeletal comorbidities and subsequently reduces energy expenditure, resulting in a vicious cycle of weight gain and rising CV risk [36,37,38][36][37][38]; moreover, total blood volume and cardiac output are higher in people with overweight/obesity, contributing to structural and functional changes to the heart and vascular system (left ventricular hypertrophy (LVH), left ventricular diastolic dysfunction and predisposition to HF [37,38,39,40][37][38][39][40]).
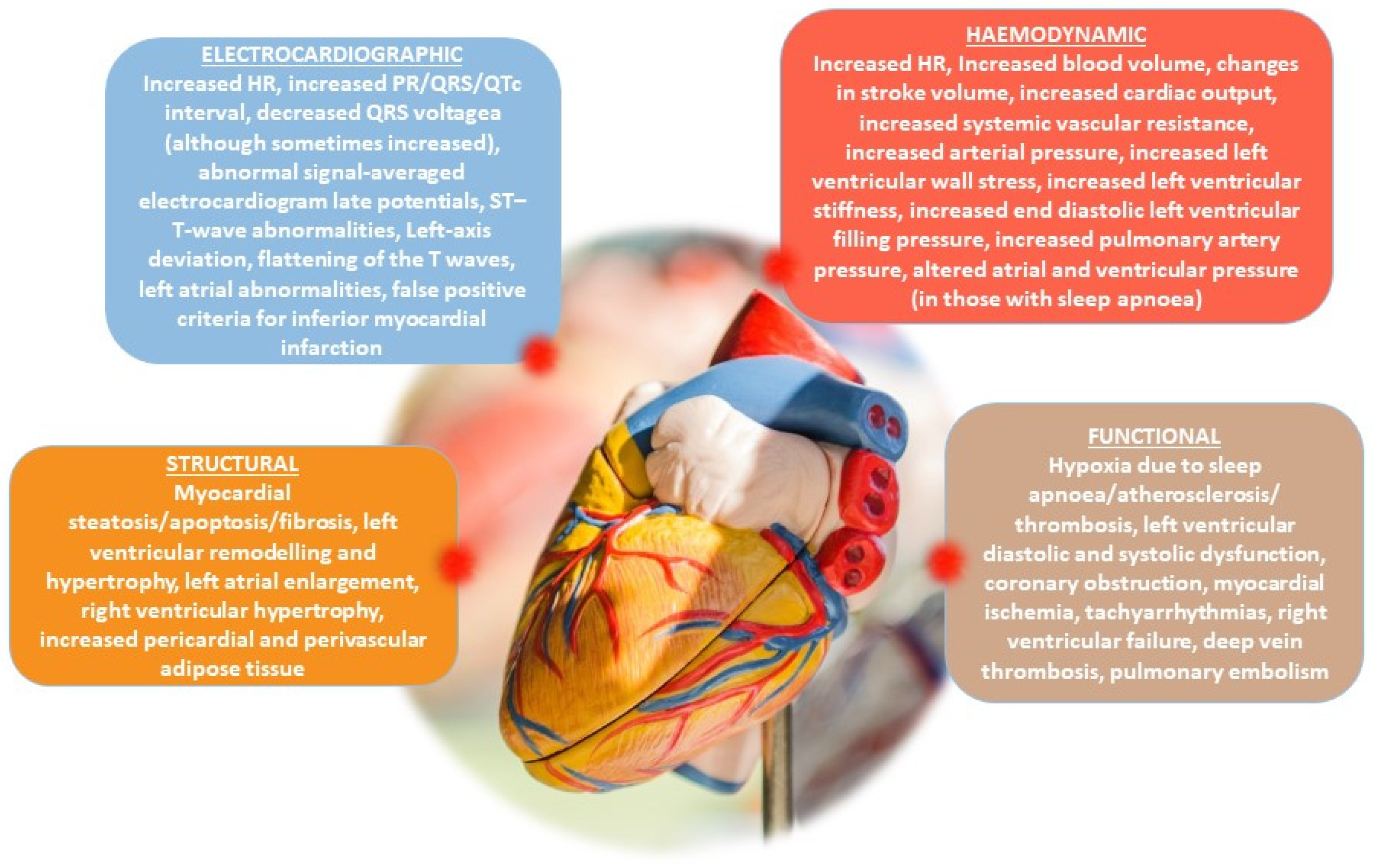
Figure 1.
The key electrocardiographic, hemodynamic, structural and functional changes associated with obesity.
These obesity-associated changes in cardiac function have been described as the “cardiomyopathy of obesity” [41]. Sensitive measures of contractile function, such as left ventricular fractional shortening, systolic velocity, and myocardial strain (circumferential and longitudinal), are impaired in the setting of obesity and/or metabolic syndrome [42,43,44,45][42][43][44][45]. Notably, cardiac functional responses to physiologic perturbations (e.g., exercise), pathologic conditions (e.g., myocardial ischemia) [46[46][47][48],47,48], or pharmacologic stimuli (e.g., catecholamines, glucagon-like-peptide-1 mimetics) [49] are also known to be significantly influenced by an obese/metabolic syndrome phenotype. Investigators in this field have identified relevant and important molecular pathways linking obesity to CV continuum and cardiac dysfunction; in particular, alterations in myocardial Ca2+ handling via changes in the functional expression of SERCA2A and ryanodine (RyR2) receptors [50,51][50][51] have been of interest. Also of note is a growing interest in modifications in the regulation of myocardial titin (which influences the passive and restoring force of the cardiac sarcomere and can contribute to hypertrophic signaling) as a potential target or mediator of obesity-associated cardiac dysfunction [50,52,53][50][52][53]. Moreover, it has been reported that weight loss through lifestyle interventions in obese patients with heart failure may result in improvements in the New York Heart Association classification, quality of life and exercise capacity [54].
One added possibility is that progressive vascular disease further influences these heart changes through mechanisms specific to the atherosclerotic process or microvascular dysfunction, independent of the obese state [55,56,57][55][56][57].
There is a growing recognition of the importance of population-level interventions, and individualized care plans with a multidisciplinary approach are recommended [25,58,59][25][58][59]; indeed, the multidisciplinary interventions describe major changes in body composition, and the recurring pattern in clinical trials is an energy reduction and control in the percentage of intake of macronutrients along with the performance of regularly structured exercise [60].
References
- Lopez-Jimenez, F.; Almahmeed, W.; Bays, H.; Cuevas, A.; Di Angelantonio, E.; le Roux, C.W.; Sattar, N.; Sun, M.C.; Wittert, G.; Pinto, F.J.; et al. Obesity and cardiovascular disease: Mechanistic insights and management strategies. A joint position paper by the World Heart Federation and World Obesity Federation. Eur. J. Prev. Cardiol. 2022, 29, 2218–2237.
- Congdon, P.; Amugsi, D. Editorial: The obesity epidemic: Causes, context, prevention. Front. Public Health 2022, 10, 1030180.
- Goryakin, Y.; Lobstein, T.; James, W.P.; Suhrcke, M. The impact of economic, political and social globalization on overweight and obesity in the 56 low and middle income countries. Soc. Sci. Med. 2015, 133, 67–76.
- Ng, M.; Fleming, T.; Robinson, M.; Thomson, B.; Graetz, N.; Margono, C.; Mullany, E.C.; Biryukov, S.; Abbafati, C.; Abera, S.F.; et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2014, 384, 766–781.
- d’Errico, M.; Pavlova, M.; Spandonaro, F. The economic burden of obesity in Italy: A cost-of-illness study. Eur. J. Health Econ. 2022, 23, 177–192.
- McLaren, L. Socioeconomic status and obesity. Epidemiol. Rev. 2007, 29, 29–48.
- Larson, N.I.; Story, M.T.; Nelson, M.C. Neighborhood environments: Disparities in access to healthy foods in the U.S. Am. J. Prev. Med. 2009, 36, 74–81.
- Story, M.; Kaphingst, K.M.; Robinson-O’Brien, R.; Glanz, K. Creating healthy food and eating environments: Policy and environmental approaches. Annu. Rev. Public Health 2008, 29, 253–272.
- Swinburn, B.A.; Sacks, G.; Hall, K.D.; McPherson, K.; Finegood, D.T.; Moodie, M.L.; Gortmaker, S.L. The global obesity pandemic: Shaped by global drivers and local environments. Lancet 2011, 378, 804–814.
- Morland, K.; Diez Roux, A.V.; Wing, S. Supermarkets, other food stores, and obesity: The atherosclerosis risk in communities study. Am. J. Prev. Med. 2006, 30, 333–339.
- Popkin, B.M.; Duffey, K.; Gordon-Larsen, P. Environmental influences on food choice, physical activity and energy balance. Physiol. Behav. 2005, 86, 603–613.
- Giskes, K.; van Lenthe, F.; Avendano-Pabon, M.; Brug, J. A systematic review of environmental factors and obesogenic dietary intakes among adults: Are we getting closer to understanding obesogenic environments? Obes. Rev. 2011, 12, e95–e106.
- Epstein, L.H.; Jankowiak, N.; Nederkoorn, C.; Raynor, H.A.; French, S.A.; Finkelstein, E. Experimental research on the relation between food price changes and food-purchasing patterns: A targeted review. Am. J. Clin. Nutr. 2012, 95, 789–809.
- Sallis, J.F.; Glanz, K. Physical activity and food environments: Solutions to the obesity epidemic. Milbank Q. 2009, 87, 123–154.
- Preston, S.H.; Vierboom, Y.C.; Stokes, A. The role of obesity in exceptionally slow US mortality improvement. Proc. Natl. Acad. Sci. USA 2018, 115, 957–961.
- Visco, V.; Pascale, A.V.; Virtuoso, N.; Mongiello, F.; Cinque, F.; Gioia, R.; Finelli, R.; Mazzeo, P.; Manzi, M.V.; Morisco, C.; et al. Serum Uric Acid and Left Ventricular Mass in Essential Hypertension. Front. Cardiovasc. Med. 2020, 7, 570000.
- Sorriento, D.; Rusciano, M.R.; Visco, V.; Fiordelisi, A.; Cerasuolo, F.A.; Poggio, P.; Ciccarelli, M.; Iaccarino, G. The Metabolic Role of GRK2 in Insulin Resistance and Associated Conditions. Cells 2021, 10, 167.
- Di Pietro, P.; Lizio, R.; Izzo, C.; Visco, V.; Damato, A.; Venturini, E.; De Lucia, M.; Galasso, G.; Migliarino, S.; Rasile, B.; et al. A Novel Combination of High-Load Omega-3 Lysine Complex (AvailOm((R))) and Anthocyanins Exerts Beneficial Cardiovascular Effects. Antioxidants 2022, 11, 896.
- Visco, V.; Izzo, C.; Mancusi, C.; Rispoli, A.; Tedeschi, M.; Virtuoso, N.; Giano, A.; Gioia, R.; Melfi, A.; Serio, B.; et al. Artificial Intelligence in Hypertension Management: An Ace up Your Sleeve. J. Cardiovasc. Dev. Dis. 2023, 10, 74.
- Grover, S.A.; Kaouache, M.; Rempel, P.; Joseph, L.; Dawes, M.; Lau, D.C.; Lowensteyn, I. Years of life lost and healthy life-years lost from diabetes and cardiovascular disease in overweight and obese people: A modelling study. Lancet Diabetes Endocrinol. 2015, 3, 114–122.
- Peto, R.; Whitlock, G.; Jha, P. Effects of obesity and smoking on U.S. life expectancy. N. Engl. J. Med. 2010, 362, 855–856.
- Di Pietro, P.; Izzo, C.; Abate, A.C.; Iesu, P.; Rusciano, M.R.; Venturini, E.; Visco, V.; Sommella, E.; Ciccarelli, M.; Carrizzo, A.; et al. The Dark Side of Sphingolipids: Searching for Potential Cardiovascular Biomarkers. Biomolecules 2023, 13, 168.
- Lakka, H.M.; Laaksonen, D.E.; Lakka, T.A.; Niskanen, L.K.; Kumpusalo, E.; Tuomilehto, J.; Salonen, J.T. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 2002, 288, 2709–2716.
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Back, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337.
- Perone, F.; Pingitore, A.; Conte, E.; Halasz, G.; Ambrosetti, M.; Peruzzi, M.; Cavarretta, E. Obesity and Cardiovascular Risk: Systematic Intervention Is the Key for Prevention. Healthcare 2023, 11, 902.
- Neeland, I.J.; Poirier, P.; Despres, J.P. Cardiovascular and Metabolic Heterogeneity of Obesity: Clinical Challenges and Implications for Management. Circulation 2018, 137, 1391–1406.
- Izzo, C.; Vitillo, P.; Di Pietro, P.; Visco, V.; Strianese, A.; Virtuoso, N.; Ciccarelli, M.; Galasso, G.; Carrizzo, A.; Vecchione, C. The Role of Oxidative Stress in Cardiovascular Aging and Cardiovascular Diseases. Life 2021, 11, 60.
- Lee, M.J.; Wu, Y.; Fried, S.K. Adipose tissue heterogeneity: Implication of depot differences in adipose tissue for obesity complications. Mol. Asp. Med. 2013, 34, 1–11.
- Fruhbeck, G.; Busetto, L.; Dicker, D.; Yumuk, V.; Goossens, G.H.; Hebebrand, J.; Halford, J.G.C.; Farpour-Lambert, N.J.; Blaak, E.E.; Woodward, E.; et al. The ABCD of Obesity: An EASO Position Statement on a Diagnostic Term with Clinical and Scientific Implications. Obes. Facts 2019, 12, 131–136.
- Fall, T.; Mendelson, M.; Speliotes, E.K. Recent Advances in Human Genetics and Epigenetics of Adiposity: Pathway to Precision Medicine? Gastroenterology 2017, 152, 1695–1706.
- Di Pietro, P.; Carrizzo, A.; Sommella, E.; Oliveti, M.; Iacoviello, L.; Di Castelnuovo, A.; Acernese, F.; Damato, A.; De Lucia, M.; Merciai, F.; et al. Targeting the ASMase/S1P pathway protects from sortilin-evoked vascular damage in hypertension. J. Clin. Investig. 2022, 132, e146343.
- Ciccarelli, M.; Giallauria, F.; Carrizzo, A.; Visco, V.; Silverio, A.; Cesaro, A.; Calabro, P.; De Luca, N.; Mancusi, C.; Masarone, D.; et al. Artificial intelligence in cardiovascular prevention: New ways will open new doors. J. Cardiovasc. Med. 2023, 24, e106–e115.
- Tietjens, J.R.; Claman, D.; Kezirian, E.J.; De Marco, T.; Mirzayan, A.; Sadroonri, B.; Goldberg, A.N.; Long, C.; Gerstenfeld, E.P.; Yeghiazarians, Y. Obstructive Sleep Apnea in Cardiovascular Disease: A Review of the Literature and Proposed Multidisciplinary Clinical Management Strategy. J. Am. Heart Assoc. 2019, 8, e010440.
- Patel, S.R. The complex relationship between weight and sleep apnoea. Thorax 2015, 70, 205–206.
- Sakers, A.; De Siqueira, M.K.; Seale, P.; Villanueva, C.J. Adipose-tissue plasticity in health and disease. Cell 2022, 185, 419–446.
- Thijssen, E.; van Caam, A.; van der Kraan, P.M. Obesity and osteoarthritis, more than just wear and tear: Pivotal roles for inflamed adipose tissue and dyslipidaemia in obesity-induced osteoarthritis. Rheumatology 2015, 54, 588–600.
- Wilding, J.P.H.; Jacob, S. Cardiovascular outcome trials in obesity: A review. Obes. Rev. 2021, 22, e13112.
- Bays, H.E. Adiposopathy is “sick fat” a cardiovascular disease? J. Am. Coll. Cardiol. 2011, 57, 2461–2473.
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Despres, J.P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation 2021, 143, e984–e1010.
- Bays, H.E.; Taub, P.R.; Epstein, E.; Michos, E.D.; Ferraro, R.A.; Bailey, A.L.; Kelli, H.M.; Ferdinand, K.C.; Echols, M.R.; Weintraub, H.; et al. Ten things to know about ten cardiovascular disease risk factors. Am. J. Prev. Cardiol. 2021, 5, 100149.
- Tune, J.D.; Goodwill, A.G.; Sassoon, D.J.; Mather, K.J. Cardiovascular consequences of metabolic syndrome. Transl. Res. 2017, 183, 57–70.
- Almeida, A.L.; Teixido-Tura, G.; Choi, E.Y.; Opdahl, A.; Fernandes, V.R.; Wu, C.O.; Bluemke, D.A.; Lima, J.A. Metabolic syndrome, strain, and reduced myocardial function: Multi-ethnic study of atherosclerosis. Arq. Bras. Cardiol. 2014, 102, 327–335.
- Aurigemma, G.P.; Silver, K.H.; Priest, M.A.; Gaasch, W.H. Geometric changes allow normal ejection fraction despite depressed myocardial shortening in hypertensive left ventricular hypertrophy. J. Am. Coll. Cardiol. 1995, 26, 195–202.
- Wong, C.Y.; O’Moore-Sullivan, T.; Leano, R.; Byrne, N.; Beller, E.; Marwick, T.H. Alterations of left ventricular myocardial characteristics associated with obesity. Circulation 2004, 110, 3081–3087.
- Avelar, E.; Cloward, T.V.; Walker, J.M.; Farney, R.J.; Strong, M.; Pendleton, R.C.; Segerson, N.; Adams, T.D.; Gress, R.E.; Hunt, S.C.; et al. Left ventricular hypertrophy in severe obesity: Interactions among blood pressure, nocturnal hypoxemia, and body mass. Hypertension 2007, 49, 34–39.
- Thakker, G.D.; Frangogiannis, N.G.; Bujak, M.; Zymek, P.; Gaubatz, J.W.; Reddy, A.K.; Taffet, G.; Michael, L.H.; Entman, M.L.; Ballantyne, C.M. Effects of diet-induced obesity on inflammation and remodeling after myocardial infarction. Am. J. Physiol. Heart Circ. Physiol. 2006, 291, H2504–H2514.
- Hoshida, S.; Yamashita, N.; Otsu, K.; Kuzuya, T.; Hori, M. Cholesterol feeding exacerbates myocardial injury in Zucker diabetic fatty rats. Am. J. Physiol. Heart Circ. Physiol. 2000, 278, H256–H262.
- Mozaffari, M.S.; Schaffer, S.W. Myocardial ischemic-reperfusion injury in a rat model of metabolic syndrome. Obesity 2008, 16, 2253–2258.
- Moberly, S.P.; Mather, K.J.; Berwick, Z.C.; Owen, M.K.; Goodwill, A.G.; Casalini, E.D.; Hutchins, G.D.; Green, M.A.; Ng, Y.; Considine, R.V.; et al. Impaired cardiometabolic responses to glucagon-like peptide 1 in obesity and type 2 diabetes mellitus. Basic. Res. Cardiol. 2013, 108, 365.
- Sassoon, D.J.; Goodwill, A.G.; Noblet, J.N.; Conteh, A.M.; Herring, B.P.; McClintick, J.N.; Tune, J.D.; Mather, K.J. Obesity alters molecular and functional cardiac responses to ischemia/reperfusion and glucagon-like peptide-1 receptor agonism. Basic. Res. Cardiol. 2016, 111, 43.
- Dincer, U.D.; Araiza, A.; Knudson, J.D.; Shao, C.H.; Bidasee, K.R.; Tune, J.D. Dysfunction of cardiac ryanodine receptors in the metabolic syndrome. J. Mol. Cell Cardiol. 2006, 41, 108–114.
- Hamdani, N.; Franssen, C.; Lourenco, A.; Falcao-Pires, I.; Fontoura, D.; Leite, S.; Plettig, L.; Lopez, B.; Ottenheijm, C.A.; Becher, P.M.; et al. Myocardial titin hypophosphorylation importantly contributes to heart failure with preserved ejection fraction in a rat metabolic risk model. Circ. Heart Fail. 2013, 6, 1239–1249.
- Zile, M.R.; Baicu, C.F.; Ikonomidis, J.S.; Stroud, R.E.; Nietert, P.J.; Bradshaw, A.D.; Slater, R.; Palmer, B.M.; Van Buren, P.; Meyer, M.; et al. Myocardial stiffness in patients with heart failure and a preserved ejection fraction: Contributions of collagen and titin. Circulation 2015, 131, 1247–1259.
- McDowell, K.; Petrie, M.C.; Raihan, N.A.; Logue, J. Effects of intentional weight loss in patients with obesity and heart failure: A systematic review. Obes. Rev. 2018, 19, 1189–1204.
- Knudson, J.D.; Dincer, U.D.; Bratz, I.N.; Sturek, M.; Dick, G.M.; Tune, J.D. Mechanisms of coronary dysfunction in obesity and insulin resistance. Microcirculation 2007, 14, 317–338.
- Berwick, Z.C.; Dick, G.M.; Tune, J.D. Heart of the matter: Coronary dysfunction in metabolic syndrome. J. Mol. Cell Cardiol. 2012, 52, 848–856.
- Murthy, V.L.; Naya, M.; Foster, C.R.; Gaber, M.; Hainer, J.; Klein, J.; Dorbala, S.; Blankstein, R.; Di Carli, M.F. Association between coronary vascular dysfunction and cardiac mortality in patients with and without diabetes mellitus. Circulation 2012, 126, 1858–1868.
- Lloyd-Jones, D.M.; Hong, Y.; Labarthe, D.; Mozaffarian, D.; Appel, L.J.; Van Horn, L.; Greenlund, K.; Daniels, S.; Nichol, G.; Tomaselli, G.F.; et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: The American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation 2010, 121, 586–613.
- Salas-Salvado, J.; Rubio, M.A.; Barbany, M.; Moreno, B. SEEDO 2007 Consensus for the evaluation of overweight and obesity and the establishment of therapeutic intervention criteria. Med. Clin. 2007, 128, 184–196.
- Perez, E.A.; Gonzalez, M.P.; Martinez-Espinosa, R.M.; Vila, M.D.M.; Reig Garcia-Galbis, M. Practical Guidance for Interventions in Adults with Metabolic Syndrome: Diet and Exercise vs. Changes in Body Composition. Int. J. Environ. Res. Public Health 2019, 16, 3481.
More
