Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Conner Chen and Version 1 by Dorota Darmochwal-Kolarz.
Recurrent pregnancy loss is a common problem in the reproductive age population of women. It can be caused by many different conditions. This problem is addressed in international guidelines that take a slightly different approach to its diagnosis and treatment.
- recurrent pregnancy loss
- RPL
- pregnancy
1. Introduction
Recurrent pregnancy loss (RPL) is a common problem in the reproductive age population of women. It is a challenging clinical issue associated with psychological aspects. Miscarriages are very difficult for patients, their partners and clinicians. The management of the problem can be different; it depends on the cause of RPL. This issue was considered in guidelines published by the Royal College of Obstetricians and Gynaecologists (RCOG) in 2011 [1], American Society of Reproductive Medicine (ASRM) in 2012 [2] and European Society of Human Reproduction and Embryology (ESHRE) in 2017 [3,4][3][4]. All guidelines define several causes of recurrent pregnancy loss such as parental genetic disorders, uterine anatomical malformations, problems with the endocrine system, hemostatic dysfunctions and others. Many causes of miscarriages are being found, and it can be treated, but still, about 50% of RPL cases remain unexplained.
2. Definition of Recurrent Pregnancy Loss
A definition of miscarriage presented by the Royal College of Obstetricians and Gynaecologists guidelines, which were published in 2011, is a spontaneous loss of pregnancy in the uterus before the fetus reaches viability. It means that miscarriage happens until the 24th week of gestation. RCOG, in their Green-top Guideline No. 17, says that RPL is a miscarriage of three or more pregnancies. Moreover, the updated guideline states that miscarriages do not have to be consecutive to be defined as recurrent pregnancy loss. It affects 1% of couples trying to have a child. It is estimated that 1–2% of pregnancies in the second trimester of pregnancy will miscarry before the 23rd week and the 6th day of pregnancy [1,5][1][5]. The proposed definition of RPL is based on earlier research from 1990 published in The Lancet, which summarizes the results of epidemiological studies. The Lancet suggests that data should be collected up to 28 weeks of gestation, but it should also be possible to assess up to 20–22 weeks or a 500 g fetal weight [6]. In 2012, a publication of the American Society of Reproductive Medicine gave a definition of RPL as a miscarriage of two or more failed clinical pregnancies. ASRM estimates that the loss of two pregnancies will happen to 5% of women, and the loss of three or more pregnancies happens to about 1% [2]. The ESHRE from 2017 defines RPL as two or more pregnancies that do not have to be consecutive [3,4][3][4]. Another aspect of miscarriage that should be considered is how we understand the definition of pregnancy. ASRM includes in its definition the importance of ultrasounds and the histological confirmation of pregnancy [2], whereas the RCOG understands pregnancy from conception, which means that it includes biochemical pregnancy [1]. In ESHRE’s opinion, pregnancy needs confirmation with the use of serum or urinary chorionic gonadothropin, and it does not include ectopic and molar pregnancies [3,4][3][4]. It is important to consider because the risk of losing biochemical pregnancies is higher than that of losing clinical pregnancies (22% vs. 0.3%) [7]. ESHRE, to provide the definition, used the results of a study by van den Boogaard et al. in 2013 on whether the pregnancy losses are consecutive or whether two versus three losses are not associated with the risk of antiphospholipid syndrome (APS) [8], research by van den Boogaard et al. in 2010 which states that there is no difference in the possibility of carrier status (of a structural chromosomal abnormality) between couples who had two or three consecutive pregnancy losses and those who had two or three non-consecutive losses [9] and the study by Egerup et al. in 2016, which showed that there is some proof that whether the pregnancy losses are consecutive or not has an impact on prognosis in unexplained RPL [10]. There are some other definitions of recurrent pregnancy loss. One of them was offered by the French National College of Obstetricians and Gynecologists (CNGOF) in 2016. The CNGOF defines RPL as a history of three consecutive (or more) early miscarriages before the 14th week of gestation [11]. Another definition was accepted by the consensus of German Society of Gynecology and Obstetrics (DGGG), the Austrian Society of Gynecology and Obstetrics (ÖGGG) and the Swiss Society of Gynecology and Obstetrics (SGGG). The DGGG, the ÖGGG and the SGGG adopt the definition presented by the WHO, which defines recurrent pregnancy loss as three consecutive miscarriages before 20 weeks of gestation [12]. RPL definitions used in individual guidelines are compared in Table 1 [1,2,4][1][2][4].| RCOG (2011) | ASRM (2012) | ESHRE (2023) |
|---|---|---|
| Three or more failed pregnancies Do not have to be consecutive |
Two or more failed clinical pregnancies | Two or more failed pregnancies Do not have to be consecutive |
| Clinical pregnancy, also includes biochemical pregnancy |
Ultrasound and histological confirmation of pregnancy | Confirmation by serum or urinary chronic gonadothropin Do not include ectopic and molar pregnancies |
3. Epidemiology
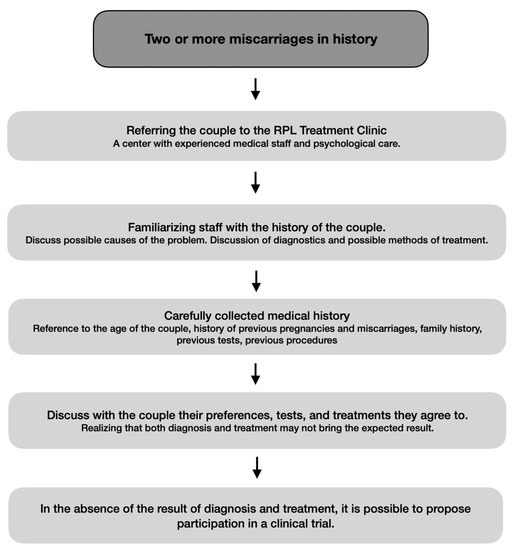
According to differences in the definitions of recurrent pregnancy loss, it is difficult to calculate the frequency of the problem. Miscarriages are a common problem which happen in one in four pregnancies [13], but RPL frequency is hard to define. It is assumed that the frequency of RPL occurs in 1–3% [7]. Due to RCOG’s guidelines, the most important risk factors for RPL are the mother’s age and the number of previous miscarriages. An advancing mother’s age is associated with quality and a lower number of oocytes. The research has shown that women aged 12–19 have a 13% risk of miscarriage, those aged 20–24 have an 11% risk, those aged 25–29 have a 12% risk, those aged 30–34 have a 15% risk, those aged 35–39 have a 25% risk, those aged 40–44 have a 51% risk and those aged ≥45 have a 93% risk. Moreover, an advanced father’s age also gives a higher risk of a miscarriage. Another issue that is taken into consideration is past reproductive history. The risk of further miscarriages is higher after each miscarriage, and after the third miscarriage, it reaches 40%. Also, the prognosis gets worse with the increase in the mother’s age [1]. Determining the epidemiology of RPL is difficult because most studies focus on spontaneous miscarriage, not RPL. Couples affected by RPL should receive tailored help. The procedure for diagnosis and treatment is included in Scheme 1 [4].References
- Royal College of Obstetricians and Gynaecologists (RCOG). The Investigation and Treatment of Couples with Recurrent First-trimester and Second-Trimester Miscarriage; Green-Top Guideline No. 17; RCOG: London, UK, 2011; Available online: https://www.rcog.org.uk/en/guidelines-research-services/guidelines/gtg17/ (accessed on 1 April 2011).
- Practice Committee of the American Society for Reproductive Medicine. Evaluation and treatment of recurrent pregnancy loss: A committee opinion. Fertil. Steril. 2012, 98, 1103–1111.
- European Society of Human Reproduction and Embryology (ESHRE). Recurrent Pregnancy Loss; ESHRE: Strombeek-Bever, Belgium, 2017; Available online: https://www.eshre.eu/Guidelines-and-Legal/Guidelines/Recurrent-pregnancy-loss.aspx (accessed on 1 November 2017).
- The ESHRE Guideline Group on RPL; Atik, R.B.; Christiansen, O.B.; Elson, J.; Kolte, A.M.; Lewis, S.; Middeldorp, S.; Mcheik, S.; Peramo, B.; Quenby, S.; et al. ESHRE guideline: Recurrent pregnancy loss: An update in 2022. Hum. Reprod. Open 2023, 2023, hoad002.
- Wyatt, P.R.; Owolabi, T.; Meier, C.; Huang, T. Age-specific risk of fetal loss observed in a second trimester serum screening population. Am. J. Obstet. Gynecol. 2005, 192, 240–246.
- Stirrat, G. Recurrent miscarriage. Lancet 1990, 336, 673–675.
- Chester, M.R.; Tirlapur, A.; Jayaprakasan, K. Current management of recurrent pregnancy loss. Obstet. Gynaecol. 2022, 24, 260–271.
- Van den Boogaard, E.; Cohn, D.M.; Korevaar, J.C.; Dawood, F.; Vissenberg, R.; Middeldorp, S.; Goddijn, M.; Farquharson, R.G. Number and sequence of preceding miscarriages and maternal age for the prediction of antiphospholipid syndrome in women with recurrent miscarriage. Fertil. Steril. 2013, 99, 188–192.
- Van den Boogaard, E.; Kaandorp, S.P.; Franssen, M.T.; Mol, B.W.; Leschot, N.J.; Wouters, C.H.; van der Veen, F.; Korevaar, J.C.; Goddijn, M. Consecutive or non-consecutive recurrent miscarriage: Is there any difference in carrier status? Hum. Reprod. 2010, 25, 1411–1414.
- Egerup, P.; Kolte, A.M.; Larsen, E.C.; Krog, M.; Nielsen, H.S.; Christiansen, O.B. Recurrent pregnancy loss: What is the impact of consecutive versus non-consecutive losses? Hum. Reprod. 2016, 31, 2428–2434.
- Delabaere, A.; Huchon, C.; Lavoue, V.; Lejeune, V.; Iraola, E.; Nedellec, S.; Gallot, V.; Capmas, P.; Beucher, G.; Subtil, D.; et al. Standardisation de la terminologie des pertes de grossesse: Consensus d’experts du Collège national des gynécologues et obstétriciens français (CNGOF). . J. Gynecol. Obstet. Biol. Reprod. 2014, 43, 756–763.
- Toth, B.; Würfel, W.; Bohlmann, M.; Zschocke, J.; Rudnik-Schöneborn, S.; Nawroth, F.; Schleußner, E.; Rogenhofer, N.; Wischmann, T.; von Wolff, M.; et al. Recurrent Miscarriage: Diagnostic and Therapeutic Procedures. Guideline of the DGGG, OEGGG and SGGG (S2k-Level, AWMF Registry Number 015/050). Geburtshilfe Frauenheilkd. 2018, 78, 364–381.
- Shields, R.; Hawkes, A.; Quenby, S. Clinical approach to recurrent pregnancy loss. Obstet. Gynaecol. Reprod. Med. 2020, 30, 331–336.
More