In the era of COVID-19, it is necessary to practice all possible measures in the clinical practice that prevents disease transmission. Dentistry bears a higher risk of cross-contamination as it deals with saliva- a potent disease-transmitting agent. Dental radiology setup is no exception, as saliva contamination is equally present here. We should undertake the following measures in order to have a safe working environment. :
1. Strict adherence to routine infection control measures
. 2. Preference should be given to the extra-oral projection techniques.
3. Ensure proper ventilation of the operator room.
4. Dooning and doffing of the PPE in a separate room
. 5. Proper disinfection and implementation of fallout period.
6. Preferably digital radiography and tele-radiography
- Dental Radiology, COVID-19, Infection Control
Note:All the information in this draft can be edited by authors. And the entry will be online only after the authors edit and submit it.
Definition:
This study intends to project a strategy about protocols, infrastructure, and daily activities in a dental radiology office that institutions can adopt with modifications according to their local scenario.
1. Introduction
On 31 December 2019, the China office of the World health organization (WHO) reported about the cases of ‘viral pneumonia’ in Wuhan, People’s Republic of China [1] Shortly, on 9 January 2020 Chinese researchers have identified the pathogen for this atypical pneumonia-like cases as novel Coronavirus [1,2][1][2]. This coronavirus belongs to the beta-corona virus family, which was initially given the name of 2019 novel coronavirus (2019-nCoV) [3]. After considerable brainstorming and research, they renamed this as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [4]. They gave the disease caused by it the name coronavirus disease 2019 (COVID-19) by WHO on 11 February 2020 [5]. Since then the cases of COVID-19 have been increasing tremendously around the world and WHO has recognized it as pandemic on 11 March 2020 [6]. This (SARS-CoV-2) has the potential to be transmitted rapidly from human to human. Symptoms such as fever, cough, shortness of breath, and diarrhea are manifested in most of the diagnosed cases [7,8][7][8].
COVID-19 era has brought a significant change in the daily routine of every individual. The world is seeing an economic crisis along with enormous death causalities. Collectively with the efforts of healthcare workers (HCWs), public and government agencies, they can minimize its spread. New guidelines and recommendations for infection control protocols need to be implemented with utmost priority. Similar to the medical set-up, the role of oral imaging in the dental set-up is indispensable in the diagnosis and treatment of elective and emergency cases. Among various possible routes of transmission of COVID-19, saliva seems to be a common factor in disease transmission and oral imaging [9]. Hence oral radiology offices can be a nidus for the spread of infection if they do not consider strict precautions. For the safety of radiology staff and patients, they recommend it to revise screening and clinical protocols of procedures [10].
Since COVID-19 is a new pandemic affecting worldwide, there are a lot of questions that need to be addressed only through scientific resources [11]. There are many uncertainties related to COVID-19 such as the patient’s carrier status in the pre-symptomatic or asymptomatic stage [12], the effectiveness of the potential vaccine, and stretch of this pandemic. Considering the gravity of COVID-19 and its potential to spread in the dental radiology office or institution, an attempt has been made to through light on how to combat COVID-19 in oral radiology clinics by modifying the layout. Additionally, this paper will highlight aspects to modify and implement new protocols in the oral radiology clinics both in academics and commercials set-up.
2. Dental Radiology and COVID-19
In the background of the COVID-19 pandemic, invariably every sector around the globe was forced to make changes in their work pattern and working environment. These changes are inevitable in order to return to work after months of lockdown. The nature and extent of changes depend on the amount of risk for disease transmission involved in a work set-up [24]. HCWs have always been at the forefront of battling the pandemic, and thus also remained at high risk for acquiring and transmitting disease [12,25,26][12][13][14]. Institutions involved in any form of health care delivery (academic, clinical care, or both) required to maintain a high standard of infection control protocol [27][15]. Dental radiology offices are no exception, and thus they have put various recommendations and guidelines forth in the lieu of COVID-19. The following section deals with the current update on recommendations applicable to dental radiology offices.
2.1. Source of Risks in Dental Radiology Office
Invariably all dental procedures involve close contact with the patient for a reasonably long duration and thus bear an increased potential for cross-contamination. Aerosol-producing dental procedures are considered to have a high risk for disease transmission, but fortunately, dental radiology set-up barely includes any such procedures [28][16]. However, most dental radiology set-up is air-conditioned with closed ventilation (no windows). Hence, inadvertently puts the HCWs in dental radiology units along with patients at risk [10]. The reflex of cough or sneeze produces aerosols that will stay suspended in the air of enclosed offices/clinics for a longer duration [14][17]. Researchers have identified the probability of < 5 microns (aerosol particles) can readily penetrate the airway up to the alveolar spaces [29][18]. Hence the above issues need to be considered in the preventive protocols in order to eliminate the disease progression.
2.2. Proposed Infrastructural Model/Layout for Dental Radiology Set-Up
The radiation exposure to the community is the primary concern while designing a dental radiology set-up. The thickness of the wall, incorporation of lead, especially while constructing the surroundings of the operatory rooms, and provision of lead barriers are some measures taken in minimizing radiation exposure. In this pandemic, considering the significance of infection control, the internal layout and ambiance need some modification. In the waiting area, they should make the sitting arrangement in such a way so that a physical distance of 2 meters can be maintained [3,8][3][8]. For maintaining hand hygiene, automatic or foot-controlled hand sanitizer dispenser should be stationed at key places. To reinforce the norms of distancing, etiquette to be displayed while speaking, and coughing and hand hygiene, they should place placards with an easy description of the measures at multiple, strategic places [10]. We should keep enclosed boxes of disposable masks and gloves in the waiting area and at the entrance of the operatory room. To avoid crowding, a prior appointment for a radiological investigation can be given. Separate rooms for each imaging modality and its respective console unit are mandatory [9]. In the case of multiple digital workstations, a distancing of 1 meter should be maintained. Isolated room for wearing and uncovering the PPEs is essential. The tactical placement of the old and new stock should be done so that new stock remains undisturbed till the potential virus remains viable on inanimate objects (Figure 1). To further set up the mitigation measures of cross-contamination, the layout of the health center can be modified to have separate entry and exit gates along with the placement of horizontal directional signage at multiple strategic places [30][19].
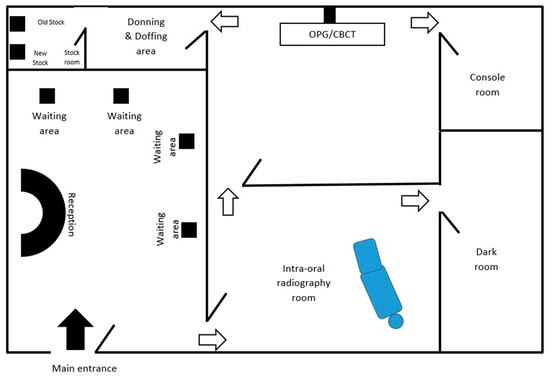
Figure 1.
The Layout of dental radiology office to ensure adherence to the infection control protocol.
2.3. General Recommendations, Practices and Protocols in Oral Radiology Clinics
Strict hand hygiene practice always remains a mainstay in the disease's prevention transmission, and it holds true for dental radiology offices as well. Alcohol-based disinfectants (70%) preferably in gel form are recommended to be used for at least 20 s [31][20]. Before entering the clinical area, the patient should undergo a screening triage which should include a temperature check and questions evaluating the risk status of the patient [9]. Recommendations suggest a cut-off temperature of 37.3°C and patients above the cut-off are considered suspected for COVID-19. In such a situation, we should advise the patient to undergo a screening test for COVID-19 and should remain in quarantine for about 14 days [25][13]. Additionally, the level of oxygen saturation can be assessed with a pulse oximeter. This will help identify patients with silent hypoxia [32][21]. In a scenario, wherein a patient has a positive contact history in the recent past (14 days), then it is advisable to undergo a confirmatory test for COVID-19 [25][13].
3. Conclusions
Saliva and aerosol are closely related to dentistry, and an established route of disease transmission. Among the dental radiographic imaging modalities, the highest risk of cross-contamination is associated with intraoral radiographic techniques. Hence, extraoral techniques such as panoramic and CBCT are preferred with caution for radiation exposure. Thus currently, in the pandemic of COVID-19, strict adherence to infection control protocol is the only way to decelerate the disease transmission. Academic institutes also need to adopt similar measures in their setting besides modification in the curriculum to meet the exceptional circumstances which are expected to stay with us for some years.
References
- Pneumonia of Unknown Cause–China. Available online: https://www.who.int/csr/don/05-january-2020-pneumonia-of-unkown-cause-china/en/ (accessed on 17 August 2020).
- Zhu, N.; Zhang, D.; Wand, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733.
- Tang, X.; Wu, C.; Li, X.; Song, Y.; Yao, X.; Wu, X.; Duan, Y.; Zhang, H.; Wang, Y.; Qian, Z.; et al. On the origin and continuing evolution of SARS-CoV-2. Natl. Sci. Rev. 2020, 6, 1012–1023.
- Ludwig, S.; Zarbock, A. Coronaviruses and SARS-CoV-2: A brief overview. Anesth Analg. 2020.
- Naming the Coronavirus Disease (COVID-19) and the Virus that Causes It. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it (accessed on 17 August 2020).
- Cucinotta, D.; Vanelli, M. WHO declares COVID-19 a pandemic. Acta Bio-Med. Atenei Parm. 2020, 91, 157–160.
- Ai, J.W.; Zi, H.; Wang, Y.; Huang, Q.; Wang, N.; Li, L.Y.; Pei, B.; Ji, J.; Zeng, X.T. Clinical Characteristics of COVID-19 Patients with Gastrointestinal Symptoms: An Analysis of Seven Patients in China. Front. Med. 2020, 7, 308.
- Riou, J.; Althaus, C.L. Pattern of early human-to-human transmission of Wuhan 2019 novel coronavirus (2019-nCoV), December 2019 to January 2020. Eurosurveillance 2020, 25, 2000058.
- Cral, W.G.; Lima, C.A.; Queluz, D.D. COVID-19 and oral radiology. Imaging Sci. Dent. 2020, 50, 181–182.
- Ilhan, B.; Bayrakdar, İ.S.; Orhan, K. Dental radiographic procedures during COVID-19 outbreak and normalization period: Recommendations on infection control. Oral Radiol. 2020, 29, 1–5.
- Srivastava, K.C.; Shrivastava, D.; Chhabra, K.G.; Naqvi, W.; Sahu, A. Facade of media and social media during covid-19: A review. Int. J. Res. Pharm. Sci. 2020, 11.
- Lai, C.C.; Shih, T.P.; Ko, W.C.; Tang, H.J.; Hsueh, P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int. J. Antimicrob Agents 2020, 55, 105924.
- Meng, L.; Hua, F.; Bian, Z. Coronavirus disease 2019 (COVID-19): Emerging and future challenges for dental and oral medicine. J. Dent. Res. 2020, 99, 481–487.
- Fallahi, H.R.; Keyhan, S.O.; Zandian, D.; Kim, S.G.; Cheshmi, B. Being a front-line dentist during the Covid-19 pandemic: A literature review. Maxillofac. Plast. Reconstr. Surg. 2020, 42, 1–9.
- Ahmed, M.A.; Jouhar, R.; Ahmed, N.; Adnan, S.; Aftab, M.; Zafar, M.S.; Khurshid, Z. Fear and practice modifications among dentists to combat Novel Coronavirus Disease (COVID-19) outbreak. Int. J. Environ. Res. Public Health 2020, 17, 2821.
- To, K.K.; Tsang, O.T.; Yip, C.C.; Chan, K.H.; Wu, T.C.; Chan, J.M.; Leung, W.S.; Chik, T.S.; Choi, C.Y.; Kandamby, D.H.; et al. Consistent detection of 2019 novel coronavirus in saliva. Clin. Infect. Dis. 2020, 71, 841–843.
- Jayaweera, M.; Perera, H.; Gunawardana, B.; Manatunge, J. Transmission of COVID-19 virus by droplets and aerosols: A critical review on the unresolved dichotomy. Environ. Res. 2020, 188, 109819.
- Tellier, R.; Li, Y.; Cowling, B.J.; Tang, J.W. Recognition of aerosol transmission of infectious agents: A commentary. BMC Infect. Dis. 2019, 19, 101.
- Recommendations for the Re-Opening of Dental Services: A Rapid Review of International Sources. Available online: https://oralhealth.cochrane.org/sites/oralhealth.cochrane.org/files/public/uploads/covid19_dental_.reopening_rapid_review_13052020.pdf (accessed on 6 May 2020).
- Wan, Y.L.; Schoepf, U.J.; Wu, C.C.; Giovagnoli, D.P.; Wu, M.T.; Hsu, H.H.; Chang, Y.C.; Yang, C.T.; Cherng, W.J. Preparedness and Best Practice in Radiology Department for COVID-19 and Other Future Pandemics of Severe Acute Respiratory Infection. J. Thorac. Imaging 2020, 35, 239–245.
- Mason, R.J. Pathogenesis of COVID-19 from a cell biology perspective. Eur. Respir. J. 2020, 55, 2000607.
