Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 3 by Dean Liu and Version 2 by Dean Liu.
General practitioners (GPs) play a crucial role in guiding patients’ health behaviors, including advising on weight loss. GPs have access to a variety of lifestyle, medical, and surgical approaches to weight loss to assist their patients.
- dietary advice
- GPs’ knowledge
- attitude
- practice
1. Content of Dietary Advice Reported
Researchers found that the majority of studies investigated general dietary advice for weight loss, while two studies focused on specific areas of diet, such as sugar-sweetened beverages [1] and added sugar [2]. Researchers identified 32 different types of dietary advice across all studies, with the most common being reduction in calorie intake and elimination diets (each mentioned in 4 articles). When further classifying the advice by dietary aspects such as quantity, quality, timing of food intake, and adherence to guidelines, researchers found that advice regarding food quality was the most frequently reported topic, with a wide range of approaches. This category encompassed 28 types of advice, including Mediterranean diets [3][4], whole foods [3][5], increasing fruits and vegetables [3][5][6], limiting added sugar [1][2], macronutrient modification [7], and reducing fat consumption [3][6][7].
Only one article reported advice regarding the timing of food intake [3]. Only two articles discussed adherence to guidelines [8][9]. Figure 1 illustrates the dietary advice reported in each eligible study.
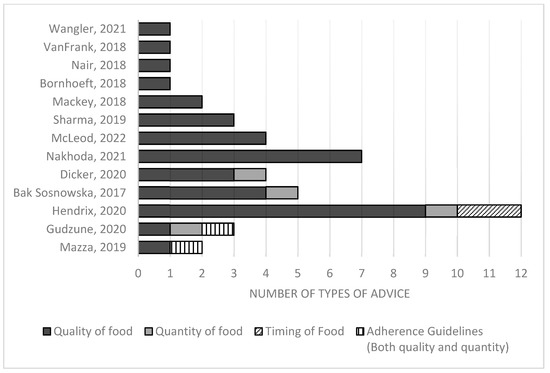
Figure 1. Number of different types of dietary advice reported in each article, classified by whether the advice was related to food quality, quantity, timing, or adherence to guidelines [1][2][3][4][5][6][7][8][9][10][11][12][13].
2. Knowledge of GPs
Although knowledge around dietary advice by GPs could be considered fundamental to attitudes and practices, only 5 out of 13 papers discussed GPs’ knowledge regarding dietary guidelines and best practice. In those that examined the knowledge of GPs, many found poor self-ratings in the area of dietary advice. For example, in a survey of 356 physicians from academic and community hospitals in the U.S., of whom 22.3% were family medicine specialists, McLeod et al. found that physicians had varying levels of knowledge regarding different dietary approaches and generally rated their own knowledge in this area as fair to poor. While 59% had good knowledge of the “portion control” approach to dietary weight loss, lower proportions of physicians reported good knowledge regarding other kinds of dietary advice, including the DASH diet (40.3%), macronutrient modification (24.7%), and saturated fat reduction (13.7%) [7]. In another study, Nakhoda et al. also reported that 80% of GPs in Iran felt they had limited nutritional knowledge [6]. Using an exploratory approach, Mazza et al. also reported that many GPs in Australia lacked familiarity with the NHMRC (National Health and Medical Research Council) obesity guidelines, including the dietary aspects advised in those guidelines, with one GP interviewed reporting their confusion about which diets to advise due to the abundance of conflicting information available [9].
3. Attitudes of GPs
Six papers were reviewed on the attitudes of GPs, including attitudes towards several different dietary approaches [2][5][6][7][12][13]. An international survey project, ACTION-IO (Awareness, Care, and Treatment in Obesity management—An International Observation), found that 84% of healthcare practitioners in Israel agreed that reducing calories is effective, while 38% and 46% agreed on elimination diets and specific diets, respectively, as being effective [12]. However, in Canada, healthcare practitioners believed that general improvement in eating habits was the most effective management approach, with lower proportions of positive attitudes towards elimination diets and specific diet programs (29% and 17%, respectively) [13].
An Iranian-based study of 500 physicians found that GPs had mixed attitudes and beliefs on various strategies to managing metabolic syndrome, including regarding weight reduction. About 21% agreed on the effectiveness of increasing vegetable and fruit intake, 72% on limiting starchy vegetables, and 82% on consuming a variety of whole grains. All (100%) agreed on limiting high-cholesterol foods and 97% on limiting high-fat dairy products [6]. When discussing the topic of added sugar, the physicians generally believed excessive consumption of added sugar significantly contributed to weight gain [2].
4. Practices of GPs
The practices of GPs in giving dietary advice were addressed in the majority of the articles reviewed (85%). Hendrix et al. conducted a survey of 1151 physicians in the U.S. (17.5% of whom were family practice members) who were part of a Facebook group. The survey asked about their dietary weight-loss strategies and what they recommended to their patients. The study discovered that a wide variety of dietary advice was recommended, with 21–35% of physicians advising intermittent fasting, 25–41% recommending a ketogenic diet, 30–40% suggesting low-carbohydrate calorie restriction, and 17–22% advising a Mediterranean diet [3]. In contrast, from an exploratory approach, Wangler et al. found that GPs recommended a healthy high-fiber diet and combined it with plenty of exercise to achieve successful outcomes for their patients [11].
Gudzune et al. examined 494 physicians who were diplomates of the American Board of Obesity Medicine (ABOM) to evaluate their adherence to multiple guidelines, including the American Heart Association (AHA), the American Association of Clinical Endocrinologists (AACE), the Obesity Medicine Association (OMA), and the Endocrine Society. They found that OMA guidelines had the highest adherence rate (65.6%), followed by AACE with 33%, the Endocrine Society with 31.6%, and the AHA with 30.8% [8]. Another study exploring adherence to guidelines was a qualitative study in Australia, which reported that GPs tried to follow what they remembered from the NHMRC guidelines and combined this with their own personal experience, such as advising their patients to cut down on certain foods [9].
VanFrank et al. conducted a more specific study focusing on GPs’ counseling related to sugar-sweetened beverages (SSBs) for weight control. Of the 1510 U.S. physicians involved (35.9% of whom were family practice members), almost all (98.5%) reported counseling patients on SSBs, including the calorie content of SSBs, added sugar, and advice about reducing the frequency of SSB consumption [1]. This finding is similar to that of Mackey et al., who also reported that 97% of family physicians advised against sugary beverage consumption and 82% advised limiting added sugar in food [2].
5. Disetary Advicussion e by GPs for Weight Control: Gaps and Challenges
The study aimed to investigate the dietary advice provided by GPs to their patients for weight control, as well as their knowledge, attitudes, and practices in this area. A previous systematic review has shown that this topic is rarely discussed in depth [14]. Moreover, prior studies have mainly focused on the barriers and facilitators of nutrition counseling without providing detailed information on the specific dietary advice given [15]. These gaps emphasize the need to gain a better understanding of the actual dietary practices of GPs.
Researchers identified 32 distinct types of dietary approaches, with some already included in established guidelines, while others were not. The dietary approaches were categorized into four main categories: quality, quantity, timing, and adherence to guidelines. This classification provides valuable insights into the dietary advice offered by general practitioners (GPs). It is noteworthy that while all the studies covered a wide range of advice pertaining to quality, less than half of them specifically addressed the quantity or the importance of reducing calorie intake, which is considered a crucial aspect of weight loss approaches. This suggests a potential shift in focus towards questions around what to eat rather than solely how much to eat. Recognizing the variety of dietary advice given by GPs to patients for weight control highlights the importance of the need for a more standardized approach in this area. Furthermore, only a limited number of studies reported advice regarding adherence to guidelines and the timing of food intake.
Importantly, the findings suggest that GPs may not always follow the guidelines. One study conducted by Hendrix et al. discovered various recent dietary approaches, including intermittent fasting, the ketogenic diet, the Mediterranean diet, and vegan diets to be frequently advised by GPs, with GPs more likely to advise dietary measures which they had personally found effective. 14 different approaches are reported, accounting for 50% of all identified weight control approaches [3]. Hendrix’s work provides valuable insights into emerging dietary trends considered by GPs and suggests that some GPs deviate from current dietary guidelines for weight loss. This lack of adherence to current dietary guidelines likely reflects GPs’ uncertainty regarding the effectiveness of these dietary approaches [16]. This may be in response to past failures in helping patients with losing weight Researchers also also revealed several other obstacles for GPs in providing adequate nutritional advice. Inadequate nutrition training during undergraduate and graduate medical education and a resulting lack of confidence and skills in assisting patients with weight loss were reported by GPs as a significant challenge to providing dietary advice revealed several other obstacles for GPs in providing adequate nutritional advice. Inadequate nutrition training during undergraduate and graduate medical education and a resulting lack of confidence and skills in assisting patients with weight loss were reported by GPs as a significant challenge to providing dietary advice [6][10]. Furthermore, time constraints and patient disinterest in weight loss were identified as additional barriers [9][13]. Enhancing GPs’ perceptions of obesity as a significant medical issue, irrespective of the presence of other chronic diseases, could help prioritize important conversations around weight with overweight patients [16]. The presence of a dietitian as part of the primary care team can alleviate time pressure and ensure that patients receive comprehensive weight-loss support and is frequently much valued by GPs in their practice [17].
References
- VanFrank, B.K.; Park, S.; Foltz, J.L.; McGuire, L.C.; Harris, D.M. Physician Characteristics Associated With Sugar-Sweetened Beverage Counseling Practices. Am. J. Health Promot. 2018, 32, 1365–1374.
- Mackey, C.; Plegue, M.A.; Deames, M.; Kittle, M.; Sonneville, K.R.; Chang, T. Family physicians’ knowledge, attitudes, and behaviors regarding the weight effects of added sugar. SAGE Open Med. 2018, 6, 2050312118801245.
- Hendrix, J.K.; Aikens, J.E.; Saslow, L.R. Dietary weight loss strategies for self and patients: A cross-sectional survey of female physicians. Obes. Med. 2020, 17, 100158.
- Bąk-Sosnowska, M.; Skrzypulec-Plinta, V. Health behaviors, health definitions, sense of coherence, and general practitioners’ attitudes towards obesity and diagnosing obesity in patients. Arch. Med. Sci. 2017, 13, 433–440.
- Bornhoeft, K. Perceptions, Attitudes, and Behaviors of Primary Care Providers Toward Obesity Management: A Qualitative Study. J. Community Health Nurs. 2018, 35, 85–101.
- Nakhoda, K.; Hosseinpour-Niazi, S.; Mirmiran, P. Nutritional knowledge, attitude, and practice of general physicians toward the management of metabolic syndrome in Tehran. Shiraz E Med. J. 2021, 22, e97514.
- McLeod, M.R.; Chionis, L.; Gregg, B.; Gianchandani, R.; Wolfson, J.A. Knowledge and attitudes of lower Michigan primary care physicians towards dietary interventions: A cross-sectional survey. Prev. Med. Reports 2022, 27, 101793.
- Gudzune, K.A.; Wickham, E.P.; Schmidt, S.L.; Stanford, F.C. Physicians certified by the American Board of Obesity Medicine provide evidence-based care. Clin. Obes. 2021, 11, e12407.
- Mazza, D.; McCarthy, E.; Carey, M.; Turner, L.; Harris, M. “90% of the time, it’s not just weight”: General practitioner and practice staff perspectives regarding the barriers and enablers to obesity guideline implementation. Obes. Res. Clin. Pract. 2019, 13, 398–403.
- Nair, D.; Hart, A. Family physicians’ perspectives on their weight loss nutrition counseling in a high obesity prevalence area. J. Am. Board Fam. Med. 2018, 31, 522–528.
- Wangler, J.; Jansky, M. Attitudes, behaviours and strategies towards obesity patients in primary care: A qualitative interview study with general practitioners in Germany. Eur. J. Gen. Pract. 2021, 27, 27–34.
- Dicker, D.; Kornboim, B.; Bachrach, R.; Shehadeh, N.; Potesman-Yona, S.; Segal-Lieberman, G. ACTION-IO as a platform to understand differences in perceptions, attitudes, and behaviors of people with obesity and physicians across countries-the Israeli experience. Isr. J. Health Policy Res. 2020, 9, 56.
- Sharma, A.M.; Bélanger, A.; Carson, V.; Krah, J.; Langlois, M.; Lawlor, D.; Lepage, S.; Liu, A.; Macklin, D.A.; MacKay, N.; et al. Perceptions of barriers to effective obesity management in Canada: Results from the ACTION study. Clin. Obes. 2019, 9, e12329.
- Walsh, K.; Grech, C.; Hill, K. Health advice and education given to overweight patients by primary care doctors and nurses: A scoping literature review. Prev. Med. Rep. 2019, 14, 100812.
- Vrkatić, A.; Grujičić, M.; Jovičić-Bata, J.; Novaković, B. Nutritional Knowledge, Confidence, Attitudes towards Nutritional Care and Nutrition Counselling Practice among General Practitioners. Healthcare 2022, 10, 2222.
- Warr, W.; Aveyard, P.; Albury, C.; Nicholson, B.; Tudor, K.; Hobbs, R.; Roberts, N.; Ziebland, S. A systematic review and thematic synthesis of qualitative studies exploring GPs’ and nurses’ perspectives on discussing weight with patients with overweight and obesity in primary care. Obes. Rev. 2021, 22, e13151.
- Abbott, S.; Parretti, H.M.; Greenfield, S. Experiences and perceptions of dietitians for obesity management: A general practice qualitative study. J. Hum. Nutr. Diet. 2021, 34, 494–503.
More
