You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is a comparison between Version 2 by Fanny Huang and Version 1 by Khaled A. Elsaid.
Proteoglycan 4 (PRG4) is a mucinous glycoprotein secreted by synovial fibroblasts and superficial zone chondrocytes, released into synovial fluid, and adsorbed on cartilage and synovial surfaces. PRG4′s roles include cartilage boundary lubrication, synovial homeostasis, immunomodulation, and suppression of inflammation. PRG4 supplementation may offer a new therapeutic option for gout.
- PRG4
- lubricin
- gout
1. Introduction
The pathophysiology of gout, the most common cause of inflammatory arthritis, includes intersections between genetics, urate homeostasis, innate immunity, and diseases of metabolism, and renal and cardiovascular function [1,2,3][1][2][3]. Urate is particularly limited in its solubility in joint tissues. Additionally, sustained hyperuricemia is a primary risk factor for deposition of monosodium urate (MSU) crystals in synovial joints, and a variety of soft tissues including bursae and tendons [2,3,4][2][3][4]. Inflammatory joint disease in gout is chronic, and characteristically punctuated clinically by bouts of acute and excruciatingly painful arthritis and soft tissue inflammation.
Acute inflammation in gout is driven via recognition of urate crystals by tissues’ monocytes/macrophages and their subsequent phagocytosis [5,6][5][6]. Activation of the NOD-, LRR- and pyrin domain-containing protein 3 (NLRP3) inflammasomes in tissue phagocytes underlies their acute response to urate crystals, resulting in the recruitment of pro-caspase-1 and its conversion to active caspase-1 [6]. Active caspase-1 converts pro-interleukin-1 beta (pro-IL-1β) to mature IL-1β, which drives inflammation in gout [4]. Synovium is comprised of a surface layer, the intima and an underlying subintima [7,8][7][8]. The intima of normal synovium is one to three cell layers thick, with two cell types: fibroblast-like synoviocytes and macrophages [7,8][7][8]. Synovial macrophages comprise heterogenous populations whose functions include the clearance of cell debris and foreign bodies, tissue immune surveillance, and the resolution of inflammation [9,10][9][10]. Importantly, cartilage-derived damage-associated molecular patterns (DAMPs) activate macrophages, and this contributes to the pathophysiology of synovitis [11].
2. Proteoglycan 4 (PRG4)/Lubricinx
The PRG4 gene is alternatively spliced and is responsible for the mucinous glycoproteins lubricin and superficial zone protein (SZP). Lubricin is secreted by synovial type B fibroblasts, and SZP by superficial zone chondrocytes [12,13,14,15][12][13][14][15]. PRG4 is a major component of synovial fluid (SF) and is localized on the surface of articular cartilage, where it functions as a boundary lubricant at near-zero sliding speeds and prevents cell and protein adhesions [13,16,17,18][13][16][17][18]. The boundary-lubricating property of PRG4 prevents friction-induced mitochondrial dysregulation and chondrocyte apoptosis [19,20][19][20]. PRG4 is also found in the synovium [21]. The full length synovial form of PRG4/lubricin has a semi-rigid structure. The protein core has 1404 amino acids with N and C termini and a central mucin domain that is heavily glycosylated via O-linked β(1–3) Gal-GalNac oligosaccharides (which account for ~50% of the mucin weight) and is responsible for its boundary-lubricating function [16,22][16][22] (Figure 1). The globular N- and C-termini of PRG4 may be involved in multiple biological functions [16]. In the N-terminus, there is a heparin-binding site, a chondroitin sulfate chain, and a somatomedin B-like domain [15,16][15][16]. The C-terminus contains a hemopexin-like domain [15,16][15][16]. In both domains, PRG4 has greater than 40% sequence similarity with vitronectin, though PRG4 has a unique repeating motif of KEPAPTT in which O-glycosylations are found [16]. Either the N- or C-terminus or both mediate PRG4’s anchoring to surfaces, which results in a brush-like conformation that provides optimal boundary lubrication [23]. The N-terminus is also the site of disulfide bonding, wherein PRG4 exists as monomers, dimers, and multimers, with improved boundary lubrication observed with multimeric PRG4 [24,25][24][25]. The concentration of PRG4 is normally high in SF (200 to 400 μg/mL) [26].
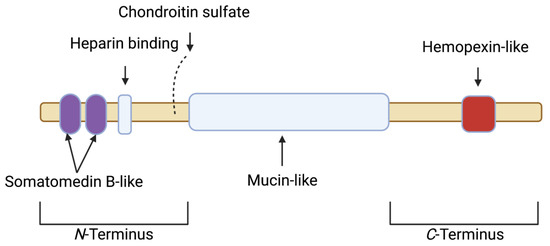
Figure 1. Schematic depicting the various motifs within the full length synovial 1404 amino acid proteoglycan 4 (PRG4) polypeptide. The N-terminus contains a somatomedin B-like domain, a heparin binding site and a chondroitin sulfate chain. The N-terminus is also the site for the disulfide bonding of PRG4 monomers. The central domain is mucin-like, and is responsible for boundary lubrication. The C-terminus contains a hemopexin-like domain.
The loss of function mutation in PRG4 is evident in the autosomal recessive disease camptodactylyl-arthropathy-coxa vara-pericarditis (CACP), a rare juvenile onset arthropathy [21,27][21][27]. The murine Prg4 knockout model displays key features of CACP disease, and the joints of Prg4 null animals exhibit synovial inflammation, hyperplasia, and fibrosis in addition to cartilage surface damage and chondrocyte apoptosis, which may not be completely reversed by Prg4 re-expression [21,28,29,30][21][28][29][30]. Human studies that have examined PRG4 SF levels in different cohorts of joint injuries, moderate OA, and advanced OA have reported either a decrease, no change, or an increase in SF PRG4 levels in reference to healthy subjects [31]. Studies that reported a decrease in SF PRG4 levels were more likely to include patients with anterior cruciate ligament or meniscal tears within one year of injury, whereas four out of five studies that reported an increase in SF PRG4 levels included patients with advanced OA [31]. It is unclear whether the different assays used in these studies to quantify SF PRG4 could differentiate between full-length and degraded protein.
Multiple studies in animals showed that cartilage, synovial PRG4 expression, or a combination thereof were reduced in mouse, rat and guinea pig models of naturally occurring and posttraumatic OA (PTOA) [32,33,34,35,36][32][33][34][35][36]. Using in vitro models, PRG4 expression in chondrocytes and synoviocytes was shown to be reduced by IL-1β and tumor necrosis factor (TNF), and increased by transforming growth factor beta 1 (TGF-β1) [37,38,39,40,41][37][38][39][40][41]. Furthermore, PRG4 is proteolytically degraded by multiple enzymes, e.g., elastase, and cathepsins B and G [36,42][36][42]. A summary of studies that showcase the disease-modifying effects of native and recombinant PRG4 in pre-clinical PTOA models is presented in Table 1 [43,44,45,46,47,48,49,50][43][44][45][46][47][48][49][50]. In addition, Prg4 gene therapy is efficacious in mitigating murine age and injury-related OA development [51,52,53][51][52][53].
Table 1. In vivo efficacy of native and recombinant PRG4/lubricin in pre-clinical models of post-traumatic osteoarthritis (PTOA) and the pharmacokinetic profile of recombinant human PRG4 as a potential biologic therapeutic for PTOA.
| Study | Model and Treatment(s) | Outcome(s) | ||||
|---|---|---|---|---|---|---|
| Flannery et al. [43] | Rat meniscectomy; I.A. recombinant human lubricin construct with one third KEPAPTT-like sequence 3× week or 1× week for 4 weeks. | Both treatments reduce cartilage degeneration and total joint scores. | ||||
| Jay et al. [44] | Rat ACLT; I.A. recombinant full-length lubricin, HSL or HSFL 2× week for 4 weeks. | HSL reduces cartilage degeneration scores; HSL and HSFL reduce uCTXII levels, and all lubricins enhance aggrecan synthesis. | ||||
| Teeple et al. [45] | Rat ACLT; I.A. hyaluronan, HSFL or hyaluronan + HSFL 2× week for 4 weeks. | HSFL alone or hyaluronan + HSFL reduce radiographic and cartilage degeneration scores with no effect by hyaluronan alone. | ||||
| Jay et al. [46] | Rat ACLT; I.A. HSL once on day 7 post-surgery and analysis at 10 weeks. | HSL enhances aggrecan synthesis, reduces uCTXII levels, and improves weight bearing in injured joints. | ||||
| Elsaid et al. [47] | Rat ACLT + forced exercise; HSFL on day 7 post-surgery and analysis at 5 weeks | Forced exercise aggravates cartilage damage and increases uCTXII excretion; HSFL treatment protects against ACLT + forced exercise cartilage damage. | ||||
| Elsaid et al. [48] | Rat ACLT; I.A. IL-1ra 4× week for one week; I.A. IL-1ra + rhPRG4 once on day 7 post-surgery and analysis at 5 weeks. | IL-1ra reduces synovial inflammation and increases lubricin levels in SF; rhPRG4 and IL-1ra synergistically reduce chondrocyte apoptosis. | ||||
| Waller et al. [49] | Minipig DMM; I.A. rhPRG4, hyaluronan or rhPRG4 + hyaluronan 3× week for one week and analysis at 26 weeks post-surgery. | rhPRG4 reduces medial tibial plateau macroscopic cartilage damage, uCTXII levels, SF, and serum IL-1β. | ||||
| Hurtig et al. [50] | Minipig ACLT; I.A. | 131 | I-rhPRG4 once with analysis at 10 min, 24, 72 h, 6, 13 and 20 days. | rhPRG4 joint elimination kinetics follows a two-compartment model with t | 1/2β | of 4.81 days. |
ACLT: anterior cruciate ligament transection; DMM: destabilization of the medial meniscus; HSL: human synoviocyte lubricin; HSFL: human synovial fluid lubricin; I.A.: intra-articular; IL-1β; interleukin-1 beta; IL-1ra: interleukin-1 receptor antagonist; rhPRG4: recombinant human proteoglycan 4; SF: synovial fluid; uCTXII: urinary C-terminal crosslinked telopeptide type II collagen.
Biologically, PRG4 binds transmembrane CD44 receptors and competes with high-molecular-weight hyaluronic acid (Hyaluronan) to do so. As a consequence of preferentially binding CD44, PRG4 reduces the mitogen-activated proliferation of mouse Prg4−/− synoviocytes and human synoviocytes from patients with OA and rheumatoid arthritis (RA) [54,55][54][55]. In OA synoviocytes, recombinant human PRG4 (rhPRG4) treatment reduces NF-κB nuclear translocation via inhibition of IκBα phosphorylation [55], with downstream reduction of the expression of matrix metalloproteinases (MMP1, MMP3, MMP9, MMP13) and cytokines IL-6 and IL-8 [55]. PRG4 also binds to the toll-like receptor (TLR) family of pattern recognition receptors [56[56][57],57], and PRG4 suppresses activation of TLR2 and TLR4 receptors by DAMPs in SF aspirates from patients with OA [57].
PRG4 plays a significant role in regulating synovial macrophages. In Prg4-deficient mice, macrophages accumulate in synovial tissues with age [58], while the tissue resident fraction is reduced. Total macrophages in the synovium skew to a predominantly CD86+ pro-inflammatory phenotype, and away from the CD206+ anti-inflammatory phenotype [58]. Prg4 re-expression in mice reduces total macrophages in synovial tissues and re-establishes homeostasis with an enrichment in anti-inflammatory CD206+ synovial macrophages [58]. Furthermore, Prg4 deficiency appears to prime acute synovitis, as demonstrated by enhanced inflammatory macrophage recruitment [58]. Interestingly, synovial macrophage depletion in otherwise Prg4-deficient mice reduces synovial hyperplasia and synovial fibrosis [58]. These collective observations support PRG4’s immunomodulatory and anti-inflammatory roles in the joint.
References
- Chen, X.M.; Yokose, C.; Rai, S.K.; Pillinger, M.H.; Choi, H.K. Contemporary Prevalence of Gout and Hyperuricemia in the United States and Decadal Trends: The National Health and Nutrition Examination Survey, 2007–2016. Arthritis Rheumatol. 2019, 71, 991–999.
- Dalbeth, N.; Merriman, T.R.; Stamp, L.K. Gout. Lancet 2016, 388, 2039–2052.
- Terkeltaub, R. What makes gouty inflammation so variable? BMC Med. 2017, 15, 158.
- So, A.; Dumusc, A.; Nasi, S. The role of IL-1 in gout: From bench to bedside. Rheumatology 2018, 57 (Suppl. S1), i12–i19.
- Martin, J.W.; Walton, M.; Harper, J. Resident macrophages initating and driving inflammation in a monosodium urate monohydrate crystal-induced murine peritoneal model of acute gout. Arthritis Rheum. 2009, 60, 281–289.
- Busso, N.; So, A. Mechanisms of inflammation in gout. Arthritis Res. Ther. 2010, 12, 206.
- Smith, M.D. The normal synovium. Open Rheumatol. J. 2011, 5, 100–106.
- Smith, M.D.; Barg, E.; Weedon, H.; Papengelis, V.; Smeets, T.; Tak, P.P.; Kraan, M.; Coleman, M.; Ahern, M.J. Microarchitecture and protective mechanisms in synovial tissue from clinically and arthroscopically normal knee joints. Ann. Rheum. Dis. 2003, 62, 303–307.
- Davies, L.C.; Taylor, P.R. Tissue-resident macrophages: Then and now. Immunology 2015, 144, 541–548.
- Davies, L.C.; Jenkins, S.J.; Allen, J.E.; Taylor, P.R. Tissue-resident macrophages. Nat. Immunol. 2013, 14, 986–995.
- Rosenberg, J.H.; Rai, V.; Dilisio, M.F.; Agrawal, D.K. Damage-associated molecular patterns in the pathogenesis of osteoarthritis: Potentially novel therapeutic targets. Mol. Cell. Biochem. 2017, 434, 171–179.
- Swann, D.A.; Silver, F.H.; Slayter, H.S.; Stafford, W.; Shore, E. The molecular structure and lubricating activity of lubricin isolated from bovine and human synovial fluids. Biochem. J. 1985, 225, 195–201.
- Jay, G.D.; Habertstroh, K.; Cha, C.J. Comparison of the boundary lubricating ability of bovine synovial fluid, lubricin, and Healon. J. Biomed. Mater. Res. 1998, 49, 414–418.
- Jay, G.D.; Britt, D.E.; Cha, C.J. Lubricin is a product of megakaryocyte stimulating factor gene expression by human synovial fibroblasts. J. Rheumatol. 2000, 27, 594–600.
- Flannery, C.R.; Hughes, C.E.; Schumacher, B.L.; Tudor, D.; Aydelotte, M.B.; Kuettner, K.E.; Caterson, B. Articular cartilage superficial zone protein (SZP) is homologous to megakaryocyte stimulating factor precursor and is a multifunctional proteoglycan with potential growth-promoting cytoprotective, and lubricating properties in cartilage metabolism. Biochem. Biophys. Res. Commun. 1999, 254, 535–541.
- Jay, G.D.; Waller, K.A. The biology of lubricin: Near frictionless joint motion. Matrix Biol. 2014, 39, 17–24.
- Ludwig, T.E.; Hunter, M.; Schmidt, T.A. Cartilage boundary lubrication synergism is mediated by hyaluronan concentration and PRG4 concentration and structure. BMC Musculoskelet. Disord. 2015, 16, 386.
- Damen, A.; Van Donkelaar, C.; Cardinaels, R.; Brandt, J.-M.; Schmidt, T.; Ito, K. Proteoglycan 4 reduces friction more than other synovial fluid components for both cartilage-cartilage and cartilage-metal articulation. Osteoarthr. Cartil. 2021, 29, 894–904.
- Waller, K.A.; Zhang, L.X.; Jay, G.D. Friction-induced mitochondrial dysregulation contributes to joint deterioration in Prg4 knockout mice. Int. J. Mol. Sci. 2017, 18, 1252.
- Larson, K.; Zhang, L.; Badger, G.; Jay, G. Early genetic restoration of lubricin expression in transgenic mice mitigates chondrocyte peroxynitrite release and caspase-3 activation. Osteoarthr. Cartil. 2017, 25, 1488–1495.
- Rhee, D.K.; Marcelino, J.; Baker, M.; Gong, Y.; Smits, P.; Lefebvre, V.; Jay, G.D.; Stewart, M.; Wang, H.; Warman, M.L.; et al. The secreted glycoprotein lubricin protects cartilage surfaces and inhibits synovial cell overgrowth. J. Clin. Investig. 2005, 115, 622–631.
- Jay, G.D.; Harris, D.A.; Cha, C.J. Boundary lubrication by lubricin is mediated by O-linked beta (1-3) Gal-GalNAc oligosaccharides. Glycoconj. J. 2001, 18, 807–815.
- Zappone, B.; Greene, G.W.; Oroudjev, E.; Jay, G.D.; Israelachvili, J.N. Molecular aspects of boundary lubrication by human lubricin: Effect of disulfide bonds with enzymatic digestion. Langmuir 2008, 24, 1495–1508.
- Abubacker, S.; Ponjevic, D.; Ham, H.O.; Messersmith, P.B.; Matyas, J.R.; Schmidt, T.A. Effect of disulfide bonding and multimerization on proteoglycan 4’s cartilage boundary lubricating ability and adsorption. Connect. Tissue Res. 2016, 57, 113–123.
- Schmidt, T.A.; Plaas, A.; Sandy, J. Disulfide-bonded multimers of proteoglycan 4(PRG4) are present in normal synovial fluids. Biochim. Biophys. Acta 2009, 1790, 375–384.
- Kosinska, M.K.; Ludwig, T.E.; Liebisch, G.; Zhang, R.; Siebert, H.-C.; Wilhelm, J.; Kaesser, U.; Dettmeyer, R.B.; Klein, H.; Ishaque, B.; et al. Articular joint lubricants during osteoarthritis and rheumatoid arthritis display altered levels and molecular species. PLoS ONE 2015, 10, e0125192.
- Rhee, D.K.; Marcelino, J.; Al-Mayouf, S.; Schelling, D.K.; Bartels, C.F.; Cui, Y.; Laxer, R.; Goldbach-Mansky, R.; Warman, M.L. Consequences of disease-causing mutations on lubricin protein synthesis, secretion, and post-translational processing. J. Biol. Chem. 2005, 280, 31325–31332.
- Waller, K.A.; Zhang, L.X.; Elsaid, K.A.; Fleming, B.C.; Warman, M.L.; Jay, G.D. Role of lubricin and boundary lubrication in the prevention of chondrocyte apoptosis. Proc. Natl. Acad. Sci. USA 2013, 110, 5852–5857.
- Hill, A.; Waller, K.A.; Cui, Y.; Allen, J.M.; Smits, P.; Zhang, L.X.; Ayturk, U.M.; Hann, S.; Lessard, S.G.; Zurakowski, D.; et al. Lubricin restoration in a mouse model of congenital deficiency. Arthritis Rheumatol. 2015, 67, 3070–3081.
- Qadri, M.; Jay, G.D.; Zhang, L.X.; Richendrfer, H.; Schmidt, T.A.; Elsaid, K.A. Proteoglycan-4 regulates fibroblast to myofibroblast transition and expression of fibrotic genes in the synovium. Arthritis Res. Ther. 2020, 22, 113.
- Watkins, A.; Reesink, H.L. Lubricin in experimental and naturally occurring osteoarthritis: A systematic review. Osteoarthr. Cartil. 2020, 28, 1303–1315.
- Musumeci, G.; Castrogiovanni, P.; Trovato, F.M.; Imbesi, R.; Giunta, S.; Szychlinska, M.A.; Loreto, C.; Castorina, S.; Mobasheri, A. Physical activity ameliorates cartilage degeneration in a rat model of aging: A study on lubricin. Scand. J. Med. Sci. Sport. 2015, 25, e222–e230.
- Wei, L.; Fleming, B.C.; Sun, X.; Teeple, E.; Wu, W.; Jay, G.D.; Elsaid, K.A.; Luo, J.; Machan, J.T.; Chen, Q. Comparison of differential biomarkers of osteoarthritis with and without posttraumatic injury in the hartley guinea pig model. J. Orthop. Res. 2010, 28, 900–906.
- Teeple, E.; Elsaid, K.A.; Fleming, B.C.; Jay, G.D.; Aslani, K.; Crisco, J.J.; Mechrefe, A.P. Coefficients of friction, lubricin, and cartilage damage in the anterior cruciate ligament-deficient guinea pig knee. J. Orthop. Res. 2008, 26, 231–237.
- Elsaid, K.A.; Machan, J.T.; Waller, K.; Fleming, B.C.; Jay, G.D. The impact of anterior cruciate ligament injury on lubricin metabolism and the effect of inhibiting tumor necrosis factor alpha on chondroprotection in an animal model. Arthritis Rheum. 2009, 60, 2997–3006.
- Elsaid, K.A.; Jay, G.D.; Chichester, C.O. Reduced expression and proteolytic susceptibility of lubricin/superficial zone protein may explain early elevation in the coefficient of friction in the joints with antigen-induced arthritis. Arthritis Rheum. 2007, 56, 108–116.
- Jones, A.R.; Flannery, C.R. Bioregulation of lubricin expression by growth factors and cytokines. Eur. Cell Mater. 2007, 13, 40–45.
- Schmidt, T.; Gastelum, N.; Han, E.; Nugent-Derfus, G.; Schumacher, B.; Sah, R. Differential regulation of proteoglycan 4 metabolism in cartilage by IL-1 alpha, IGF-1, and TGF-beta 1. Osteoarthr. Cartil. 2008, 16, 90–97.
- McNary, S.M.; Athanasiou, K.A.; Reddi, A.H. Transforming growth factor-β induced superficial zone protein accumulation in the surface zone of articular cartilage is dependent on the cytoskeleton. Tissue Eng. Part A 2014, 20, 921–929.
- Blewis, M.E.; Lao, B.J.; Schumacher, B.L.; Bugbee, W.D.; Sah, R.L.; Firestein, G.S. Interactive cytokine regulation of synoviocyte lubricant secretion. Tissue Eng. Part A 2010, 16, 1329–1337.
- Cuellar, A.; Reddi, A.H. Stimulation of superficial zone protein/lubricin/PRG4 by transforming growth factor-β in superficial zone articular chondrocytes and modulation by glycosaminoglycans. Tissue Eng. Part A 2015, 21, 1973–1981.
- Huang, S.; Thomsson, K.A.; Jin, C.; Alweddi, S.; Struglics, A.; Rolfson, O.; Björkman, L.I.; Kalamajski, S.; Schmidt, T.A.; Jay, G.D.; et al. Cathepsin g degrades both glycosylated and unglycosylated regions of lubricin, a synovial mucin. Sci. Rep. 2020, 10, 4215.
- Flannery, C.R.; Zollner, R.; Corcoran, C.; Jones, A.R.; Root, A.; Rivera-Bermúdez, M.A.; Blanchet, T.; Gleghorn, J.P.; Bonassar, L.J.; Bendele, A.M.; et al. Prevention of cartilage degeneration in a rat model of osteoarthritis by intraarticular treatment with recombinant lubricin. Arthritis Rheum. 2009, 60, 840–847.
- Jay, G.D.; Fleming, B.C.; Watkins, B.A.; McHugh, K.A.; Anderson, S.C.; Zhang, L.X.; Teeple, E.; Waller, K.A.; Elsaid, K.A. Prevention of cartilage degeneration and restoration of chondroprotection by lubricin tribosupplementation in the rat following anterior cruciate ligament transection. Arthritis Rheum. 2010, 62, 2382–2391.
- Teeple, E.; Elsaid, K.A.; Jay, G.D.; Zhang, L.; Badger, G.J.; Akelman, M.; Bliss, T.F.; Fleming, B.C. Effects of supplemental intra-articular lubricin and hyaluronic acid on the progression of posttraumatic arthritis in the anterior cruciate ligament-deficient rat knee. Am. J. Sport. Med. 2011, 39, 164–172.
- Jay, G.D.; Elsaid, K.A.; Kelly, K.A.; Anderson, S.C.; Zhang, L.; Teeple, E.; Waller, K.; Fleming, B.C. Prevention of cartilage degeneration and gait asymmetry by lubricin tribosupplementation in the rat following anterior cruciate ligament transection. Arthritis Rheum. 2012, 64, 1162–1171.
- Elsaid, K.; Zhang, L.; Waller, K.; Tofte, J.; Teeple, E.; Fleming, B.; Jay, G. The impact of forced joint exercise on lubricin biosynthesis from articular cartilage following ACL transection and intra-articular lubricin’s effect in exercised joints following ACL transection. Osteoarthr. Cartil. 2012, 20, 940–948.
- Elsaid, K.A.; Zhang, L.; Shaman, Z.; Patel, C.; Schmidt, T.A.; Jay, G.D. The impact of early intra-articular administration of interleukin-1 receptor antagonist on lubricin metabolism and cartilage degeneration in an anterior cruciate ligament transection model. Osteoarthr. Cartil. 2015, 23, 114–121.
- Waller, K.A.; Chin, K.E.; Jay, G.D.; Zhang, L.X.; Teeple, E.; McAllister, S.; Badger, G.J.; Schmidt, T.A.; Fleming, B.C. Intra-articular recombinant human proteoglycan-4 mitigates cartilage damage after destabilization of the medial meniscus in the Yucatan minipig. Am. J. Sport. Med. 2017, 45, 1512–1521.
- Hurtig, M.; Zaghoul, I.; Sheardown, H.; Schmidt, T.A.; Liu, L.; Zhang, L.; Elsaid, K.A.; Jay, G.D. Two compartment pharmacokinetic model describes the intra-articular delivery and retention of rhPRG4 following ACL transection in the Yucatan mini pig. J. Orthop. Res. 2019, 37, 386–396.
- Ruan, M.Z.C.; Erez, A.; Guse, K.; Dawson, B.; Bertin, T.; Chen, Y.; Jiang, M.-M.; Yustein, J.; Gannon, F.; Lee, B.H.L. Proteoglycan 4 expression protects against the development of osteoarthritis. Sci. Transl. Med. 2013, 5, 176ra34.
- Ruan, M.Z.; Cerullo, V.; Cela, R.; Clarke, C.; Lundgren-Akerlund, E.; Barry, M.A.; Lee, B.H. Treatment of osteoarthritis using a helper-dependent adenoviral vector. Mol. Ther. Methods Clin. Dev. 2016, 3, 16008.
- Stone, A.; Grol, M.W.; Ruan, M.Z.C.; Dawson, B.; Chen, Y.; Jiang, M.-M.; Song, I.-W.; Jayaram, P.; Cela, R.; Gannon, F.; et al. Combinatorial Prg4 and IL-1ra gene therapy protects against hyperalgesia and cartilage degeneration in post-traumatic osteoarthritis. Hum. Gene Ther. 2019, 30, 225–235.
- Al-Sharif, A.; Jamal, M.; Zhang, L.X.; Larson, K.; Schmidt, T.A.; Jay, G.D.; Elsaid, K.A. Lubricin/proteoglycan 4 binding to CD44 receptor: A mechanism of the suppression of proinflammatory cytokine-induced synoviocyte proliferation by lubricin. Arthritis Rheumatol. 2015, 67, 1503–1513.
- Alquraini, A.; Jamal, M.; Zhang, L.; Schmidt, T.; Jay, G.D.; Elsaid, K.A. The autocrine role of proteoglycan-4 (PRG4) in modulating osteoarthritic synoviocyte proliferation and expression of matrix degrading enzymes. Arthritis Res. Ther. 2017, 19, 89.
- Iqbal, S.M.; Leonard, C.; Regmi, S.C.; De Rantere, D.; Tailor, P.; Ren, G.; Ishida, H.; Hsu, C.; Abubacker, S.; Pang, D.S.; et al. Lubricin/Proteoglycan 4 binds and regulates the activity of toll-like receptors in vitro. Sci. Rep. 2016, 6, 18910.
- Alquraini, A.; Garguilo, S.; D’souza, G.; Zhang, L.X.; Schmidt, T.A.; Jay, G.D.; Elsaid, K.A. The interaction of lubricin/proteoglycan 4 (PRG4) with toll-like receptors 2 and 4: An anti-inflammatory role of PRG4 in synovial fluid. Arthritis Res. Ther. 2015, 17, 353.
- Qadri, M.; Jay, G.D.; Zhang, L.X.; Schmidt, T.A.; Totonchy, J.; Elsaid, K.A. Proteoglycan-4 is an essential regulator of synovial macrophage polarization and inflammatory macrophage joint infiltration. Arthritis Res. Ther. 2021, 23, 241.
More
