You're using an outdated browser. Please upgrade to a modern browser for the best experience.
Please note this is a comparison between Version 1 by Zuzana Siroka and Version 3 by Lindsay Dong.
Cases of ingestion of indoor poisonous plants are relatively common among animals and lead to both acute cases of poisoning and long-term exposure to harmful substances and chronic damage to the animal’s health. Plants produce a large number of secondary metabolites, which serve to protect the plant from attacks by insects, parasitic plants, fungi or, for example, during reproduction. However, these metabolites can be toxic if ingested by animals or humans. Toxicologically effective components found in plants are mainly alkaloids, glycosides, saponins, terpenes and others.
For the full References please check the original article (https://www.mdpi.com/2072-6651/15/5/346).
- aroid plants
- bulb plants
- euphorbias
- lily
- cyclamen
1. Introduction
Toxically effective components found in plants are mainly alkaloids, glycosides, saponins, terpenes and others [1][2]. In plants, they are found in different proportions and quantities, which, in addition to the type of plant or cultivar in the case of cultivated plants, also depends on external conditions, such as, e.g., temperature, exposure to light or soil composition [3]. Factors that influence the possibility of poisoning in animals include the resistance/sensitivity of certain animal species (e.g., insufficient glucuronidation in cats), as well as the individuality of animals (health condition, nutrition, genetic predisposition, tendency to eat plants in non-herbivorous species, etc.). The age of the animal (the young tend to be more severely affected due to their curiosity and lack of detoxifying enzymes), boredom (especially in single household pets), changes in the household and new plants introduced are other important factors influencing the risk of plant poisoning [1][4]. The prevailing type of plants involved in poisoning may depend also on their popularity, as there are variable trends among plant growers.









2. House Plants
2.1. Aroid Plants (Araceae)
Plants from the arum family include, for example, dieffenbachia/dumbcane (Dieffenbachia spp., Figure 1), monstera plants (Monstera deliciosa, Figure 2, M. aff. adansonii or Monkey Mask, Figure 3, karsteniana, etc., or Raphidophora tetrasperma, known as Monstera minima), philodendrons (Philodendron spp., Figure 4), the syngonium/arrowhead plant (Syngonium spp., Figure 5), the anthurium/flamingo flower (Anthurium spp., Figure 6), peace lily (Spatiphyllum, Figure 7), calla lily (Zantedeschia aethiopica, Figure 8), devil’s ivy (Epipremnum spp., incorrectly called pothos, Figure 9), satin pothos/silver pothos (Scindapsus spp.), caladium/elephant ears (Caladium spp.), Chinese evergreen (Aglaonema spp., Figure 10), alocasia/elephant ears (Alocasia spp.), etc.
Figure 1.
Dieffenbachia seguine
Cool beauty (contains calcium oxalates; author: Zuzana Siroka).

Figure 2.
Monstera deliciosa
(contains calcium oxalates; author: Zuzana Siroka).

Figure 3.
Monstera aff. adansonii
, monkey mask (contains calcium oxalates; author: Zuzana Siroka).

Figure 4.
Philodendron selloum
Green princess (contains calcium oxalates; author: Zuzana Siroka).

Figure 5.
Syngonium podophyllum
(contains calcium oxalates; author: Zuzana Siroka).

Figure 6.
Anthurium andreanum
(contains calcium oxalates; author: Lenka Divisova).

Figure 7.
Spatiphyllum wallissii
(contains calcium oxalates; author: Lenka Divisova).

Figure 8.
Zantedeschia aethiopica
(contains calcium oxalates; author: Lenka Divisova).
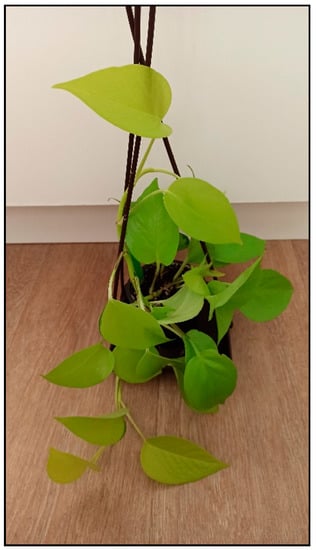
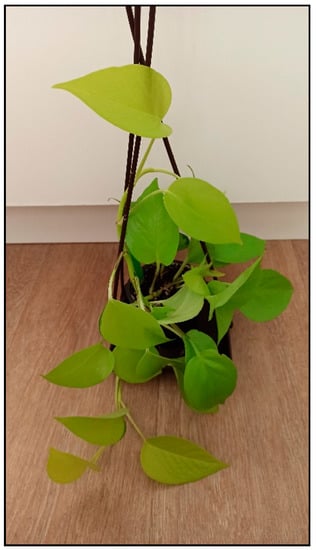
Figure 9.
Epipremnum aureum
Neon (contains calcium oxalates; author: Zuzana Siroka).

Figure 10.
Aglaonema commutatum
(contains calcium oxalates; author: Lenka Divisova).
These plants contain oxalate crystals (oxalates, mainly calcium salts), usually in the form of raphides (needles grooved at both ends) in the ejector cells, as well as oxalic acid and proteolytic enzymes. Oxalates in the form of sharp crystals have irritating effects on the skin and mucous membranes, which, due to their shape, become stuck in the tissues and release histamine from the mast cells, which is then responsible for the symptoms of poisoning. With chronic consumption, oxalates lead to kidney and urinary tract damage. Oxalic acid in excess can cause hypocalcemia. Bromeliad plants, such as tillandsia/air plants (Tilandsia), the urn plant (Aechmea spp.) and vriesea/the flaming sword plant (Vriesea), oxalis/shamrock (Oxalis spp.) or begonia tubers (Begonia tuberhybrida) have similar effects.
2.2. Euphorbia/Spurge Plants (Euphorbiaceae)
Indoor plants from this family include, for example, the poinsettia/Christmas star plant (Euphorbia pulcherrima, Figure 11), crown of thorns (Euphorbia milii, Figure 12), Madagascar jewel plant (Euphorbia leuconera, Figure 13) or croton (Codiaeum variegatum, Figure 14). Poisonings are described in dogs, cats, small rodents and birds. Poisonings are usually mild compared to the toxicity caused by outdoor spurges.


Figure 11.
Euphorbia pulcherrima
(contains diterpens; author: Lenka Divisova).
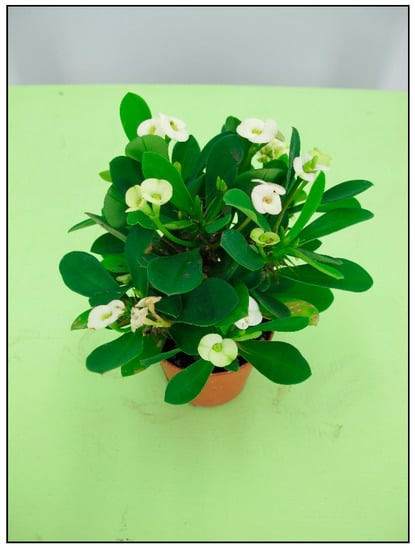
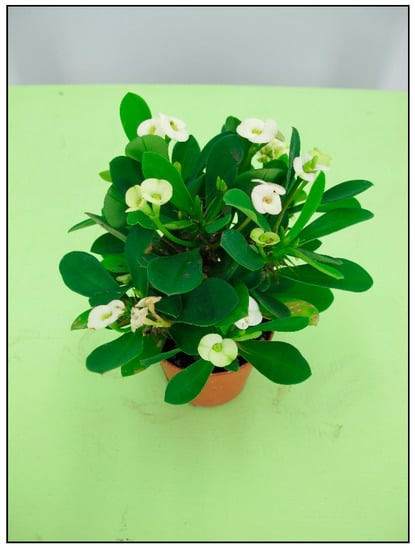
Figure 12.
Euphorbia milii
(contains diterpens; author: Lenka Divisova).


Figure 13.
Euphorbia leuconera
(contains diterpens; author: Zuzana Siroka).


Figure 14.
Codiaeum variegatum
(contains diterpens; author: Lenka Divisova).
After injury, the plants exude latex milk, which contains diterpenes, which are dermatotoxic (causing itching, swelling, rashes, and blisters) and belong to the co-carcinogens (which intensify the carcinogenic effect of other substances and agents).
2.3. Cyclamens (Cyclamen
spp.
)
These plants belong to the Primulaceae family. Persian cyclamen (Cyclamen persicum, Figure 15) is mainly grown as a houseplant.


Figure 15.
Cyclamen persicum
(contains saponins; author: Zuzana Siroka).
The tubers of these plants contain saponins, e.g., cyclamine, which, unlike most saponins, is well-absorbed from the GIT. Cyclamine has a strong hemolytic effect.
The mechanism of action of saponins is interference with lipids in the cell membrane and a change in its permeability and later integrity. In this way, the cells of the mucous membranes and the skin are affected locally, and after absorption, lysis of erythrocytes also occurs.

2.4. Dracaena (Dracaena
spp.
), Cordyline (Cordyline
spp.), Snake Plant/Mother-In-Law’s Tongue (San
), Snake Plant/Mother-In-Law’s Tongue (Sansevieria
sevieria spp.
)
There are many species and color varieties of dracaena plant (Figure 16 and Figure 17) and cordyline plant. Like mother-in-law’s tongues (Figure 18), they belong to the asparagus family (Asparagaceae), but sometimes they are also included in the agave family (Agavaceae); these families are intermingled. One of the species belonging to this group is Dracaena sanderiana (Figure 19), which is sold under the misleading name lucky bamboo.
Figure 16.
Dracaena marginata
(contains saponins; author: Lenka Divisova).


Figure 17.
Dracaena
spp. (contains saponins; author: Lenka Divisova).


Figure 18.
Sansevieria trifasciata
(contains saponins; author: Lenka Divisova).


Figure 19.
Dracaena sanderiana
Lucky bamboo (contains saponins; author: Zuzana Siroka).
All these plants contain saponins with an irritating and potentially hemolytic effect. The mechanism of action of saponins is, as mentioned above (see cyclamens), interference with lipids in the cell membrane and a change in its permeability and later integrity.

2.5. Bulb Plants
In households, bulb plants appear most often during winter and early spring as single-use decorative plants (e.g., tulips, daffodils, hyacinths, crocuses, and grape hyacinths; Figure 20, Figure 21 and Figure 22), or year-round plants, e.g., clivias (Clivia minata, Figure 23), hippeastrum/Barbados lily (Hippeastrum x hortorum, Figure 24) or amaryllis (Amaryllis belladonna). These plants usually belong to the Amaryllidaceae or Liliaceae families (formerly a joint family).
Figure 20.
Narcissus pseudonarcissus
(contains neurotoxic alkaloids; author: Lenka Divisova).


Figure 21.
Crocus vernus
(contains alkaloids; author: Zuzana Siroka).


Figure 22.
Muscari armeniacum
(contains alkaloids; author: Zuzana Siroka).
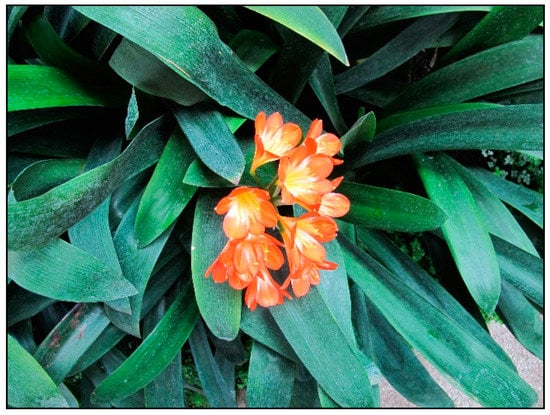
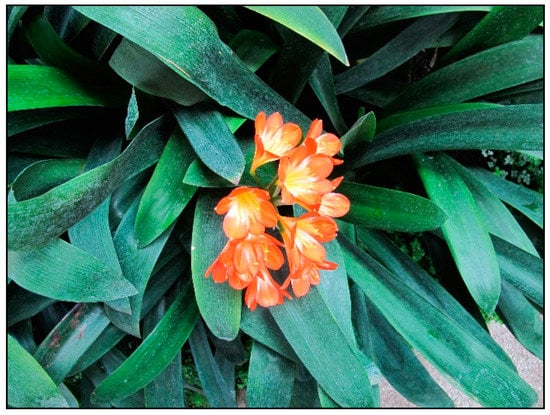
Figure 23.
Clivia minata
(contains alkaloids; author: Lenka Divisova).


Figure 24.
Hippeastrum x hortorum
(contains alkaloids; author: Zuzana Siroka).
These plants contain alkaloids, e.g., lycorine, galantamine, tazetine, and oxalate crystals, usually in the form of raphides. The highest concentrations of the active ingredients are usually in the bulb. The exact mechanism of action of substances in most of these plants is not precisely known, but alkaloids are often neurotoxic and cytotoxic. The effect of galantamine, which acts as a reversible inhibitor of acetylcholinesterase (acetylcholine accumulates in the synapse), has been studied. Lycorine also inhibits cholinesterases, inhibits proteosynthesis and further induces apoptosis. Tulips mainly contain locally acting glycosidic substances called tuliposides, which cause allergic reactions and mild to severe contact dermatitis.

2.6. Lilies (Easter Lily, Asiatic, Oriental and Other Lily Hybrids, generally Lilium
spp.
)
Lilies (Figure 25) are bulb plants that belong to the Liliaceae family; in addition to garden growing, they can be also kept as potted indoor plants and often appear in homes as cut flowers. Although they can also cause mild gastrointestinal symptoms due to oxalates, the main risk resulting from consumption lies in the possibility of developing kidney damage or even kidney failure, which is described specifically in cats. The substance that causes renal toxicity is unknown.
Figure 25.
Lilium
hybrid (toxic substance is unknown; author Zuzana Siroka).
It is assumed that poisoning in cats is caused by the lack of some metabolizing enzymes, so in cats an alternative metabolic pathway possibly results in the formation of a toxic metabolite, which does not occur in other animal species. The entire plant, including the pollen, is poisonous, with the lethal dose for a cat being approximately two leaves or petals of the plant.

2.7. Common/English Ivy (Hedera helix)
The mechanism of action of saponins is interference with lipids in the cell membrane and a change in its permeability and later integrity. The cells of the mucous membranes and the skin are affected locally, and after absorption hemolysis also occurs. In ivy, damage to hepatocytes is also possible, but usually does not occur in acute poisonings. Polyins (mainly falcarinol and its derivates) are irritants and allergens which interact with proteins in the cells. These are also found in other indoor plants from the Araliaceae family such as Fatsia japonica (Figure 26), ivy tree (Fatshedera), Schefflera arboricola or actinophylla (Figure 27).
Figure 26.
Fatsia japonica
(contains saponins; author: Zuzana Siroka).


Figure 27.
Schefflera arboricola
(contains saponins; author: Lenka Divisova).
2.8. Mistletoe (Viscum album)
During Christmas time, poisonings from white mistletoe used for decorative purposes are encountered. This semi-parasitic plant belongs to the Loranthaceae family and contains alkaline proteins, polypeptidic viscotoxins and lectins, which are also proteinaceous in nature. Lectins bind to ribosomes and thereby inhibit them which results in the inhibition of proteosynthesis. Lectins also damage the cell membrane and have a hemagglutination effect. Viscotoxins damage DNA synthesis, affect the permeability of cell membranes and are cytotoxic and hepatotoxic. Since mistletoe is a semi-parasitic plant, its toxicity can also depend on the species of tree it grows on.
2.9. Oleander/Nerium (Nerium oleander)
Among other plants causing winter poisoning in domestic animals and summer poisoning in rodents or tortoises kept in summer enclosures is oleander (Figure 28
), which must be kept indoors during the winter in many mild- to cold-climate countries, because it is not frost-resistant. It belongs to the dogbane family (Apocynaceae) and contains cardiac glycosides. These are also found in indoor plants such as kalanchoe (
Kalanchoe blossfeldiana
,
Figure 29
) or desert rose (
Adenium obesum
,
Figure 30
).


Figure 28.
Nerium oleander
(contains cardiac glucosides; author: Zuzana Siroka).


Figure 29.
Kalanchoe blossfeldiana
(contains cardiac glucosides; author: Lenka Divisova).


Figure 30.
Adenium obesum
(contains cardiac glycosides; author: Lenka Divisova).
The bitter taste of most cardiac glycosides often does not have a sufficient deterrent effect, but sometimes their ingestion leads to protracted vomiting and thus the absorbed dose is reduced. Cardiac glycosides undergo enterohepatic circulation.
2.10. Plants Containing Pyrrolizidine Alkaloids
Among the indoor plants, these substances are mainly contained in the genus Senecio (e.g., string of pearls, S. rowleyanus, Figure 31, or S. barbertonicus) from the Asteraceae family. Rabbits and rodents (with the exception of the rat) are relatively less sensitive to these plants. Poisoning usually manifests itself only after chronic consumption of such plants, while acute poisonings are rare. Poisonings from house senecios are less frequent and less serious than outdoor senecio/ragwort poisonings.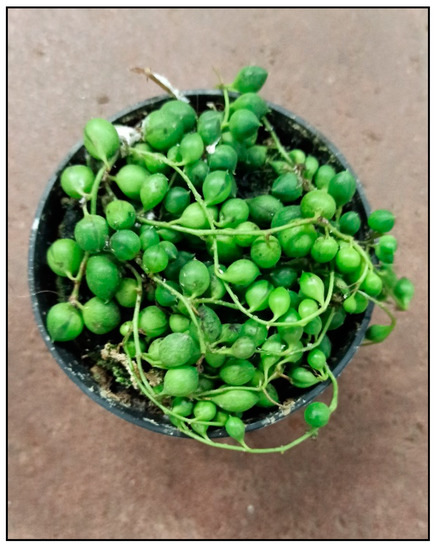
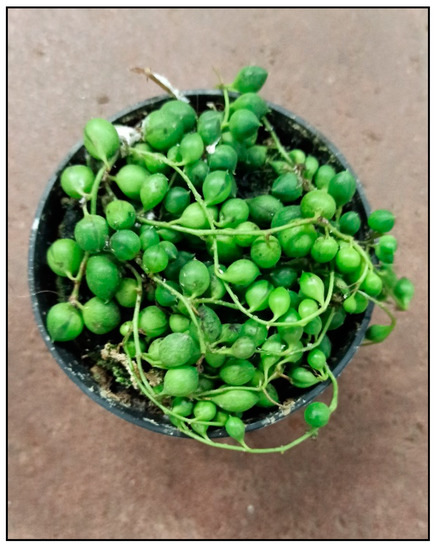
Figure 31.
Senecio rowleyanus
(contains pyrrolizidine alkaloids; author: Zuzana Siroka).
In the liver, pyrrolizidine alkaloids are metabolized by cytochrome P450, which bioactivates them by forming reactive pyrroles from them. These then act as alkylating agents and damage cellular proteins, RNA and DNA by forming adducts and cross-links, resulting in the loss of function of proteins and nucleic acids. The result is cytotoxicity (mainly the liver is damaged), mutagenicity and carcinogenicity. Sometimes, the lungs are also affected. The resulting formation of reactive oxygen species and the binding of pyrrolizidine alkaloids to the SH groups of proteins and enzymes probably further contribute to organ damage.

2.11. Plants Causing Allergic Reactions and Other Toxic Plants
2.11.1. Allergenic Plants
Allergic reactions are usually caused by skin contact with the plant, but can also occur after ingesting the plant. The most common symptom is skin irritation. Representatives of this type of toxicity include some wax plants (Hoya spp.), chrysanthemums (Chrysanthemum spp.), coleus (Coleus spp.), ficuses/fig plants (Ficus elastica—Figure 32, Ficus benjamina—Figure 33, Ficus benghalensis, Ficus lyrata, etc.), poison primrose (Primula obconica), African milk bush (Synadenium grantii), aralia (Polyscias spp.), geranium (Pelargonium spp.), spiderwort and creeping inch plants (Tradescantia and Callisia spp.). or citrus plants.
Figure 32.
