Many countries are facing the advent of super-aging societies, where sarcopenia and frailty will become pertinent problems. The prevalence of comorbidities is a major problem in countries with aged populations as elderly people suffer from various diseases, such as diabetes, heart failure, chronic kidney disease and dementia. All of these diseases are associated with sarcopenia and frailty, and they frequently cause falls, fractures, and a decline in activities of daily living. Fractures in the elderly people are associated with bone fragility, which is influenced by diabetes and chronic kidney disease. Nutritional support for chronic disease patients and sarcopenic individuals with adequate energy and protein intake, vitamin D supplementation, blood glucose level management for individuals with diabetes, obesity prevention, nutritional education for healthy individuals, and the enlightenment of society could be crucial to solve the health-related problems in super-aging societies.
- sarcopenia
- frailty
- comorbidity
- diabetes
- chronic kidney disease (CKD)
- heart failure
- dementia
- vitamin D
- oral nutritional supplement (ONS)
- elderly people
1. Introduction
2. Can Nutrition Contribute to a Reduction in Sarcopenia, Frailty, and Comorbidities in a Super-Aged Society?
Researchers provide an overview of the literatures to determine whether nutrient deficiencies relate to the risk of diseases and whether nutrient intake can prevent the onset of diseases or enhance treatment outcomes (Figure 1). Malnutrition and nutrient deficiencies have been associated with an increased risk of CKD [90,91[42][43][44][45],92,93], stroke [157,158,159][46][47][48], osteoporosis [193[49][50],194], fractures [229[51][52][53],230,231], and dementia [183,184,185,186][54][55][56][57]. Nutritional interventions can reduce the risk and improve the prognosis of these diseases [97,98,99,193,232,233,234,235,236,237][49][58][59][60][61][62][63][64][65][66].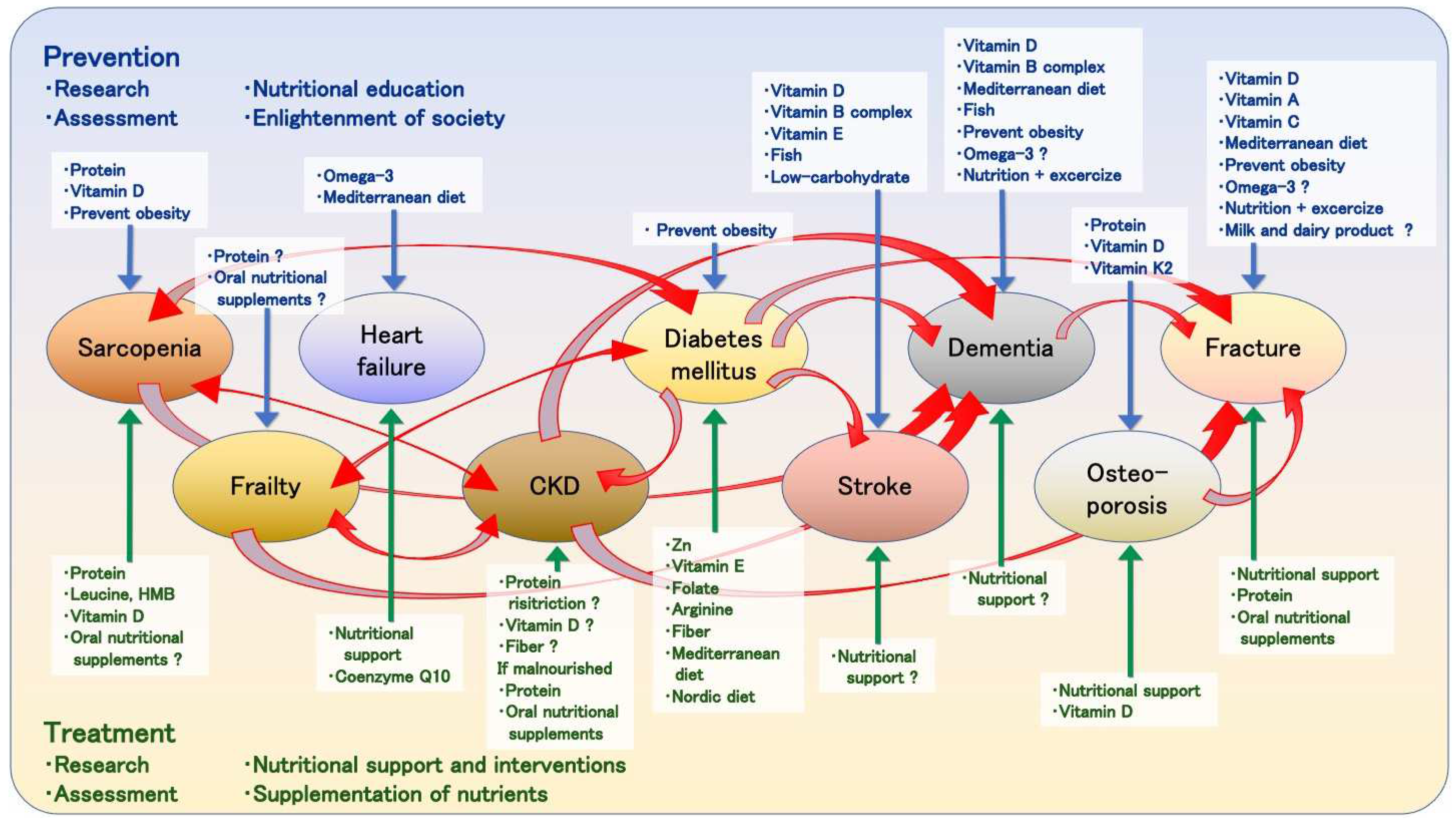
References
- The Department of Economic and Social Affairs of the United Nations. World Social Report 2023: Leaving No One behind in an Aging World; United Nations: New York, NY, USA, 2023.
- The World Bank. Population Ages 65 and above (% of Total). Available online: http://databank.worldbank.org/databases/population-dynamics (accessed on 16 May 2023).
- American Diabetes Association. Older Adults: Standards of Medical Care in Diabetes-2019. Diabetes Care 2019, 42, S139–S147.
- Sun, H.; Saeedi, P.; Karuranga, S.; Pinkepank, M.; Ogurtsova, K.; Duncan, B.B.; Stein, C.; Basit, A.; Chan, J.C.N.; Mbanya, J.C.; et al. IDF Diabetes Atlas: Global, Regional and Country-Level Diabetes Prevalence Estimates for 2021 and Projections for 2045. Diabetes Res. Clin. Pract. 2022, 183, 109119.
- Van Riet, E.E.S.; Hoes, A.W.; Wagenaar, K.P.; Limburg, A.; Landman, M.A.J.; Rutten, F.H. Epidemiology of Heart Failure: The Prevalence of Heart Failure and Ventricular Dysfunction in Older Adults over Time. A Systematic Review. Eur. J. Heart Fail. 2016, 18, 242–252.
- Emmons-Bell, S.; Johnson, C.; Roth, G. Prevalence, Incidence and Survival of Heart Failure: A Systematic Review. Heart 2022, 108, 1351–1360.
- Ohno, Y.; Ishimura, E.; Naganuma, T.; Kondo, K.; Fukushima, W.; Mui, K.; Inaba, M.; Hirota, Y. Prevalence of and Factors Associated with Chronic Kidney Disease (CKD) in Japanese Subjects without Notable Chronic Diseases, Undergoing an Annual Health Checkup. Kidney Blood Press. Res. 2012, 36, 139–148.
- Murphy, D.; McCulloch, C.E.; Lin, F.; Banerjee, T.; Bragg-Gresham, J.L.; Eberhardt, M.S.; Morgenstern, H.; Pavkov, M.E.; Saran, R.; Powe, N.R.; et al. Trends in Prevalence of Chronic Kidney Disease in the United States. Ann. Intern. Med. 2016, 165, 473–481.
- Betzler, B.K.; Sultana, R.; He, F.; Tham, Y.C.; Lim, C.C.; Wang, Y.X.; Nangia, V.; Tai, E.S.; Rim, T.H.; Bikbov, M.M.; et al. Impact of Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) GFR Estimating Equations on CKD Prevalence and Classification among Asians. Front. Med. 2022, 9, 957437.
- Zemedikun, D.T.; Gray, L.J.; Khunti, K.; Davies, M.J.; Dhalwani, N.N. Patterns of Multimorbidity in Middle-Aged and Older Adults: An Analysis of the UK Biobank Data. Mayo Clin. Proc. 2018, 93, 857–866.
- Wafa, H.A.; Wolfe, C.D.A.; Emmett, E.; Roth, G.A.; Johnson, C.O.; Wang, Y. Burden of Stroke in Europe: Thirty-Year Projections of Incidence, Prevalence, Deaths, and Disability-Adjusted Life Years. Stroke 2020, 51, 2418–2427.
- Avan, A.; Hachinski, V. Stroke and Dementia, Leading Causes of Neurological Disability and Death, Potential for Prevention. Alzheimer’s Dement. 2021, 17, 1072–1076.
- Tarvonen-Schröder, S.; Niemi, T.; Koivisto, M. Inpatient Rehabilitation after Acute Severe Stroke: Predictive Value of the National Institutes of Health Stroke Scale among Other Potential Predictors for Discharge Destination. Adv. Rehabil. Sci. Pract. 2023, 12, 27536351231157970.
- Makovski, T.T.; Schmitz, S.; Zeegers, M.P.; Stranges, S.; van den Akker, M. Multimorbidity and Quality of Life: Systematic Literature Review and Meta-Analysis. Ageing Res. Rev. 2019, 53, 100903.
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European Consensus on Definition and Diagnosis. Age Ageing 2019, 48, 16–31.
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.W.; Chou, M.Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e2.
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in Older Adults: Evidence for a Phenotype. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2001, 56, M146–M157.
- Bahat, G.; Ilhan, B. Sarcopenia and the Cardiometabolic Syndrome: A Narrative Review. Eur. Geriatr. Med. 2016, 7, 220–223.
- Stewart, R. Cardiovascular Disease and Frailty: What Are the Mechanistic Links? Clin. Chem. 2019, 65, 80–86.
- Bone, A.E.; Hepgul, N.; Kon, S.; Maddocks, M. Sarcopenia and Frailty in Chronic Respiratory Disease: Lessons from Gerontology. Chron. Respir. Dis. 2017, 14, 85–99.
- Sinclair, A.J.; Abdelhafiz, A.H.; Rodríguez-Mañas, L. Frailty and Sarcopenia—Newly Emerging and High Impact Complications of Diabetes. J. Diabetes Complicat. 2017, 31, 1465–1473.
- Pacifico, J.; Geerlings, M.A.J.; Reijnierse, E.M.; Phassouliotis, C.; Lim, W.K.; Maier, A.B. Prevalence of Sarcopenia as a Comorbid Disease: A Systematic Review and Meta-Analysis. Exp. Gerontol. 2020, 131, 110801.
- Pacifico, J.; Reijnierse, E.M.; Lim, W.K.; Maier, A.B. The Association between Sarcopenia as a Comorbid Disease and Incidence of Institutionalisation and Mortality in Geriatric Rehabilitation Inpatients: REStORing Health of Acutely Unwell AdulTs (RESORT). Gerontology 2021, 68, 498–508.
- Kim, S.H.; Jeong, J.B.; Kang, J.; Ahn, D.-W.; Kim, J.W.; Kim, B.G.; Lee, K.L.; Oh, S.; Yoon, S.H.; Park, S.J.; et al. Association between Sarcopenia Level and Metabolic Syndrome. PLoS ONE 2021, 16, e0248856.
- Chowdhury, R.; Peel, N.M.; Krosch, M.; Hubbard, R.E. Frailty and Chronic Kidney Disease: A Systematic Review. Arch. Gerontol. Geriatr. 2017, 68, 135–142.
- Sabatino, A.; Cuppari, L.; Stenvinkel, P.; Lindholm, B.; Avesani, C.M. Sarcopenia in Chronic Kidney Disease: What Have We Learned so Far? J. Nephrol. 2021, 34, 1347–1372.
- Ribeiro, H.S.; Neri, S.G.R.; Oliveira, J.S.; Bennett, P.N.; Viana, J.L.; Lima, R.M. Association between Sarcopenia and Clinical Outcomes in Chronic Kidney Disease Patients: A Systematic Review and Meta-Analysis. Clin. Nutr. 2022, 41, 1131–1140.
- Peng, T.C.; Chen, W.L.; Wu, L.W.; Chang, Y.W.; Kao, T.W. Sarcopenia and Cognitive Impairment: A Systematic Review and Meta-Analysis. Clin. Nutr. 2020, 39, 2695–2701.
- Landi, F.; Liperoti, R.; Russo, A.; Giovannini, S.; Tosato, M.; Capoluongo, E.; Bernabei, R.; Onder, G. Sarcopenia as a Risk Factor for Falls in Elderly Individuals: Results from the IlSIRENTE Study. Clin. Nutr. 2012, 31, 652–658.
- Yeung, S.S.Y.; Reijnierse, E.M.; Pham, V.K.; Trappenburg, M.C.; Lim, W.K.; Meskers, C.G.M.; Maier, A.B. Sarcopenia and Its Association with Falls and Fractures in Older Adults: A Systematic Review and Meta-Analysis. J. Cachexia Sarcopenia Muscle 2019, 10, 485–500.
- GBD 2019 Dementia Forecasting Collaborators. Estimation of the Global Prevalence of Dementia in 2019 and Forecasted Prevalence in 2050: An Analysis for the Global Burden of Disease Study 2019. Lancet Public Health 2022, 7, e105–e125.
- Scheltens, P.; Blennow, K.; Breteler, M.M.B.; de Strooper, B.; Frisoni, G.B.; Salloway, S.; Van der Flier, W.M. Alzheimer’s Disease. Lancet 2016, 388, 505–517.
- O’Brien, J.T.; Thomas, A. Vascular Dementia. Lancet 2015, 386, 1698–1706.
- Vishwanath, S.; Qaderi, V.; Steves, C.J.; Reid, C.M.; Hopper, I.; Ryan, J. Cognitive Decline and Risk of Dementia in Individuals with Heart Failure: A Systematic Review and Meta-Analysis. J. Card. Fail. 2022, 28, 1337–1348.
- Viggiano, D.; Wagner, C.A.; Martino, G.; Nedergaard, M.; Zoccali, C.; Unwin, R.; Capasso, G. Mechanisms of Cognitive Dysfunction in CKD. Nat. Rev. Nephrol. 2020, 16, 452–469.
- Bordier, L.; Doucet, J.; Boudet, J.; Bauduceau, B. Update on Cognitive Decline and Dementia in Elderly Patients with Diabetes. Diabetes Metab. 2014, 40, 331–337.
- Aranda, M.P.; Kremer, I.N.; Hinton, L.; Zissimopoulos, J.; Whitmer, R.A.; Hummel, C.H.; Trejo, L.; Fabius, C. Impact of Dementia: Health Disparities, Population Trends, Care Interventions, and Economic Costs. J. Am. Geriatr. Soc. 2021, 69, 1774–1783.
- Burks, H.B.; des Bordes, J.K.A.; Chadha, R.; Holmes, H.M.; Rianon, N.J. Quality of Life Assessment in Older Adults with Dementia: A Systematic Review. Dement. Geriatr. Cogn. Disord. 2021, 50, 103–110.
- Haagsma, J.A.; Olij, B.F.; Majdan, M.; van Beeck, E.F.; Vos, T.; Castle, C.D.; Dingels, Z.V.; Fox, J.T.; Hamilton, E.B.; Liu, Z.; et al. Falls in Older Aged Adults in 22 European Countries: Incidence, Mortality and Burden of Disease from 1990 to 2017. Inj. Prev. 2020, 26, i67–i74.
- Dyer, S.M.; Crotty, M.; Fairhall, N.; Magaziner, J.; Beaupre, L.A.; Cameron, I.D.; Sherrington, C.; Fragility Fracture Network (FFN) Rehabilitation Research Special Interest Group. A Critical Review of the Long-Term Disability Outcomes Following Hip Fracture. BMC Geriatr. 2016, 16, 158.
- Guzon-Illescas, O.; Perez Fernandez, E.; Crespí Villarias, N.; Quirós Donate, F.J.; Peña, M.; Alonso-Blas, C.; García-Vadillo, A.; Mazzucchelli, R. Mortality after Osteoporotic Hip Fracture: Incidence, Trends, and Associated Factors. J. Orthop. Surg. Res. 2019, 14, 203.
- Rahimlu, M.; Shab-Bidar, S.; Djafarian, K. Body Mass Index and All-Cause Mortality in Chronic Kidney Disease: A Dose-Response Meta-Analysis of Observational Studies. J. Ren. Nutr. 2017, 27, 225–232.
- Xiong, J.; Wang, M.; Zhang, Y.; Nie, L.; He, T.; Wang, Y.; Huang, Y.; Feng, B.; Zhang, J.; Zhao, J. Association of Geriatric Nutritional Risk Index with Mortality in Hemodialysis Patients: A Meta-Analysis of Cohort Studies. Kidney Blood Press. Res. 2018, 43, 1878–1889.
- Carrero, J.J.; Thomas, F.; Nagy, K.; Arogundade, F.; Avesani, C.M.; Chan, M.; Chmielewski, M.; Cordeiro, A.C.; Espinosa-Cuevas, A.; Fiaccadori, E.; et al. Global Prevalence of Protein-Energy Wasting in Kidney Disease: A Meta-Analysis of Contemporary Observational Studies from the International Society of Renal Nutrition and Metabolism. J. Ren. Nutr. 2018, 28, 380–392.
- Mihaescu, A.; Masood, E.; Zafran, M.; Khokhar, H.T.; Augustine, A.M.; Filippo, A.; Van Biesen, W.; Farrigton, K.; Carrero, J.J.; Covic, A.; et al. Nutritional Status Improvement in Elderly CKD Patients: A Systematic Review. Int. Urol. Nephrol. 2021, 53, 1603–1621.
- Huppertz, V.; Guida, S.; Holdoway, A.; Strilciuc, S.; Baijens, L.; Schols, J.M.G.A.; van Helvoort, A.; Lansink, M.; Muresanu, D.F. Impaired Nutritional Condition after Stroke from the Hyperacute to the Chronic Phase: A Systematic Review and Meta-Analysis. Front. Neurol. 2021, 12, 780080.
- Hu, J.; Chen, T.; Wang, Z.; Chen, X.; Lin, K.; Zhang, G.; Wu, J. Geriatric Nutritional Risk Index and the Prognosis of Patients with Stroke: A Meta-Analysis. Horm. Metab. Res. 2022, 54, 736–746.
- Mehta, A.; De Paola, L.; Pana, T.A.; Carter, B.; Soiza, R.L.; Kafri, M.W.; Potter, J.F.; Mamas, M.A.; Myint, P.K. The Relationship between Nutritional Status at the Time of Stroke on Adverse Outcomes: A Systematic Review and Meta-Analysis of Prospective Cohort Studies. Nutr. Rev. 2022, 80, 2275–2287.
- Shams-White, M.M.; Chung, M.; Du, M.; Fu, Z.; Insogna, K.L.; Karlsen, M.C.; LeBoff, M.S.; Shapses, S.A.; Sackey, J.; Wallace, T.C.; et al. Dietary Protein and Bone Health: A Systematic Review and Meta-Analysis from the National Osteoporosis Foundation. Am. J. Clin. Nutr. 2017, 105, 1528–1543.
- Zittermann, A.; Schmidt, A.; Haardt, J.; Kalotai, N.; Lehmann, A.; Egert, S.; Ellinger, S.; Kroke, A.; Lorkowski, S.; Louis, S.; et al. Protein Intake and Bone Health: An Umbrella Review of Systematic Reviews for the Evidence-Based Guideline of the German Nutrition Society. Osteoporos. Int. 2023, 1–19.
- Li, S.; Zhang, J.; Zheng, H.; Wang, X.; Liu, Z.; Sun, T. Prognostic Role of Serum Albumin, Total Lymphocyte Count, and Mini Nutritional Assessment on Outcomes after Geriatric Hip Fracture Surgery: A Meta-Analysis and Systematic Review. J. Arthroplast. 2019, 34, 1287–1296.
- Foo, M.X.E.; Wong, G.J.Y.; Lew, C.C.H. A Systematic Review of the Malnutrition Prevalence in Hospitalized Hip Fracture Patients and Its Associated Outcomes. JPEN J. Parenter. Enteral. Nutr. 2021, 45, 1141–1152.
- Liu, N.; Lv, L.; Jiao, J.; Zhang, Y.; Zuo, X.-L. Association between Nutritional Indices and Mortality after Hip Fracture: A Systematic Review and Meta-Analysis. Eur. Rev. Med. Pharmacol. Sci. 2023, 27, 2297–2304.
- Doorduijn, A.S.; van de Rest, O.; van der Flier, W.M.; Visser, M.; de van der Schueren, M.A.E. Energy and Protein Intake of Alzheimer’s Disease Patients Compared to Cognitively Normal Controls: Systematic Review. J. Am. Med. Dir. Assoc. 2019, 20, 14–21.
- Fetherstonhaugh, D.; Haesler, E.; Bauer, M. Promoting Mealtime Function in People with Dementia: A Systematic Review of Studies Undertaken in Residential Aged Care. Int. J. Nurs. Stud. 2019, 96, 99–118.
- Borders, J.C.; Blanke, S.; Johnson, S.; Gilmore-Bykovskyi, A.; Rogus-Pulia, N. Efficacy of Mealtime Interventions for Malnutrition and Oral Intake in Persons with Dementia: A Systematic Review. Alzheimer’s Dis. Assoc. Disord. 2020, 34, 366–379.
- Tangvik, R.J.; Bruvik, F.K.; Drageset, J.; Kyte, K.; Hunskår, I. Effects of Oral Nutrition Supplements in Persons with Dementia: A Systematic Review. Geriatr. Nurs. 2021, 42, 117–123.
- Jing, Z.; Wei-Jie, Y. Effects of Soy Protein Containing Isoflavones in Patients with Chronic Kidney Disease: A Systematic Review and Meta-Analysis. Clin. Nutr. 2016, 35, 117–124.
- Liu, P.J.; Ma, F.; Wang, Q.Y.; He, S.L. The Effects of Oral Nutritional Supplements in Patients with Maintenance Dialysis Therapy: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. PLoS ONE 2018, 13, e0203706.
- Mah, J.Y.; Choy, S.W.; Roberts, M.A.; Desai, A.M.; Corken, M.; Gwini, S.M.; McMahon, L.P. Oral Protein-Based Supplements versus Placebo or No Treatment for People with Chronic Kidney Disease Requiring Dialysis. Cochrane Database Syst. Rev. 2020, 5, CD012616.
- Liu, M.; Yang, J.; Yu, X.; Huang, X.; Vaidya, S.; Huang, F.; Xiang, Z. The Role of Perioperative Oral Nutritional Supplementation in Elderly Patients after Hip Surgery. Clin. Interv. Aging 2015, 10, 849–858.
- Peeters, C.M.M.; Visser, E.; Van de Ree, C.L.P.; Gosens, T.; Den Oudsten, B.L.; De Vries, J. Quality of Life after Hip Fracture in the Elderly: A Systematic Literature Review. Injury 2016, 47, 1369–1382.
- Ernst, A.; Wilson, J.M.; Ahn, J.; Shapiro, M.; Schenker, M.L. Malnutrition and the Orthopaedic Trauma Patient: A Systematic Review of the Literature. J. Orthop. Trauma 2018, 32, 491–499.
- Takahashi, K.; Momosaki, R.; Yasufuku, Y.; Nakamura, N.; Maeda, K. Nutritional Therapy in Older Patients with Hip Fractures Undergoing Rehabilitation: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2020, 21, 1364–1364.e6.
- Lai, W.-Y.; Chiu, Y.-C.; Lu, K.-C.; Huang, I.-T.; Tsai, P.-S.; Huang, C.-J. Beneficial Effects of Preoperative Oral Nutrition Supplements on Postoperative Outcomes in Geriatric Hip Fracture Patients: A PRISMA-Compliant Systematic Review and Meta-Analysis of Randomized Controlled Studies. Medicine 2021, 100, e27755.
- Szklarzewska, S.; Mottale, R.; Engelman, E.; De Breucker, S.; Preiser, J.-C. Nutritional Rehabilitation after Acute Illness among Older Patients: A Systematic Review and Meta-Analysis. Clin. Nutr. 2023, 42, 309–336.
- Komar, B.; Schwingshackl, L.; Hoffmann, G. Effects of Leucine-Rich Protein Supplements on Anthropometric Parameter and Muscle Strength in the Elderly: A Systematic Review and Meta-Analysis. J. Nutr. Health Aging 2015, 19, 437–446.
- Martínez-Arnau, F.M.; Fonfría-Vivas, R.; Cauli, O. Beneficial Effects of Leucine Supplementation on Criteria for Sarcopenia: A Systematic Review. Nutrients 2019, 11, 2504.
- Lee, S.Y.; Lee, H.J.; Lim, J.-Y. Effects of Leucine-Rich Protein Supplements in Older Adults with Sarcopenia: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Arch. Gerontol. Geriatr. 2022, 102, 104758.
- Guo, Y.; Fu, X.; Hu, Q.; Chen, L.; Zuo, H. The Effect of Leucine Supplementation on Sarcopenia-Related Measures in Older Adults: A Systematic Review and Meta-Analysis of 17 Randomized Controlled Trials. Front. Nutr. 2022, 9, 929891.
- Wu, H.; Xia, Y.; Jiang, J.; Du, H.; Guo, X.; Liu, X.; Li, C.; Huang, G.; Niu, K. Effect of Beta-Hydroxy-Beta-Methylbutyrate Supplementation on Muscle Loss in Older Adults: A Systematic Review and Meta-Analysis. Arch. Gerontol. Geriatr. 2015, 61, 168–175.
- Bear, D.E.; Langan, A.; Dimidi, E.; Wandrag, L.; Harridge, S.D.R.; Hart, N.; Connolly, B.; Whelan, K. β-Hydroxy-β-Methylbutyrate and Its Impact on Skeletal Muscle Mass and Physical Function in Clinical Practice: A Systematic Review and Meta-Analysis. Am. J. Clin. Nutr. 2019, 109, 1119–1132.
- Lin, Z.; Zhao, A.; He, J. Effect of β-Hydroxy-β-Methylbutyrate (HMB) on the Muscle Strength in the Elderly Population: A Meta-Analysis. Front. Nutr. 2022, 9, 914866.
- Zanini, B.; Simonetto, A.; Zubani, M.; Castellano, M.; Gilioli, G. The Effects of Cow-Milk Protein Supplementation in Elderly Population: Systematic Review and Narrative Synthesis. Nutrients 2020, 12, 2548.
- Da Camargo, L.R.; Doneda, D.; Oliveira, V.R. Whey Protein Ingestion in Elderly Diet and the Association with Physical, Performance and Clinical Outcomes. Exp. Gerontol. 2020, 137, 110936.
- Martin-Cantero, A.; Reijnierse, E.M.; Gill, B.M.T.; Maier, A.B. Factors Influencing the Efficacy of Nutritional Interventions on Muscle Mass in Older Adults: A Systematic Review and Meta-Analysis. Nutr. Rev. 2021, 79, 315–330.
- Gielen, E.; Beckwée, D.; Delaere, A.; De Breucker, S.; Vandewoude, M.; Bautmans, I.; Sarcopenia Guidelines Development Group of the Belgian Society of Gerontology and Geriatrics (BSGG). Nutritional Interventions to Improve Muscle Mass, Muscle Strength, and Physical Performance in Older People: An Umbrella Review of Systematic Reviews and Meta-Analyses. Nutr. Rev. 2021, 79, 121–147.
- Khor, P.Y.; Vearing, R.M.; Charlton, K.E. The Effectiveness of Nutrition Interventions in Improving Frailty and Its Associated Constructs Related to Malnutrition and Functional Decline among Community-Dwelling Older Adults: A Systematic Review. J. Hum. Nutr. Diet. 2022, 35, 566–582.
- Tieland, M.; Franssen, R.; Dullemeijer, C.; van Dronkelaar, C.; Kyung Kim, H.; Ispoglou, T.; Zhu, K.; Prince, R.L.; van Loon, L.J.C.; de Groot, L.C.P.G.M. The Impact of Dietary Protein or Amino Acid Supplementation on Muscle Mass and Strength in Elderly People: Individual Participant Data and Meta-Analysis of RCT’s. J. Nutr. Health Aging 2017, 21, 994–1001.
- Wu, P.-Y.; Huang, K.-S.; Chen, K.-M.; Chou, C.-P.; Tu, Y.-K. Exercise, Nutrition, and Combined Exercise and Nutrition in Older Adults with Sarcopenia: A Systematic Review and Network Meta-Analysis. Maturitas 2021, 145, 38–48.
- Liao, C.-D.; Wu, Y.-T.; Tsauo, J.-Y.; Chen, P.-R.; Tu, Y.-K.; Chen, H.-C.; Liou, T.-H. Effects of Protein Supplementation Combined with Exercise Training on Muscle Mass and Function in Older Adults with Lower-Extremity Osteoarthritis: A Systematic Review and Meta-Analysis of Randomized Trials. Nutrients 2020, 12, 2422.
- Conde Maldonado, E.; Marqués-Jiménez, D.; Casas-Agustench, P.; Bach-Faig, A. Effect of Supplementation with Leucine Alone, with Other Nutrients or with Physical Exercise in Older People with Sarcopenia: A Systematic Review. Endocrinol. Diabetes Nutr. 2022, 69, 601–613.
- Kirwan, R.P.; Mazidi, M.; Rodríguez García, C.; Lane, K.E.; Jafari, A.; Butler, T.; Perez de Heredia, F.; Davies, I.G. Protein Interventions Augment the Effect of Resistance Exercise on Appendicular Lean Mass and Handgrip Strength in Older Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Am. J. Clin. Nutr. 2022, 115, 897–913.
- Choi, M.; Kim, H.; Bae, J. Does the Combination of Resistance Training and a Nutritional Intervention Have a Synergic Effect on Muscle Mass, Strength, and Physical Function in Older Adults? A Systematic Review and Meta-Analysis. BMC Geriatr. 2021, 21, 639.
- Beaudart, C.; Dawson, A.; Shaw, S.C.; Harvey, N.C.; Kanis, J.A.; Binkley, N.; Reginster, J.Y.; Chapurlat, R.; Chan, D.C.; Bruyère, O.; et al. Nutrition and Physical Activity in the Prevention and Treatment of Sarcopenia: Systematic Review. Osteoporos. Int. 2017, 28, 1817–1833.
- Thomas, D.K.; Quinn, M.A.; Saunders, D.H.; Greig, C.A. Protein Supplementation Does Not Significantly Augment the Effects of Resistance Exercise Training in Older Adults: A Systematic Review. J. Am. Med. Dir. Assoc. 2016, 17, e1–e9.
- Courel-Ibáñez, J.; Vetrovsky, T.; Dadova, K.; Pallarés, J.G.; Steffl, M. Health Benefits of β-Hydroxy-β-Methylbutyrate (HMB) Supplementation in Addition to Physical Exercise in Older Adults: A Systematic Review with Meta-Analysis. Nutrients 2019, 11, 2082.
- Theodorakopoulos, C.; Jones, J.; Bannerman, E.; Greig, C.A. Effectiveness of Nutritional and Exercise Interventions to Improve Body Composition and Muscle Strength or Function in Sarcopenic Obese Older Adults: A Systematic Review. Nutr. Res. 2017, 43, 3–15.
- Yin, Y.-H.; Liu, J.Y.W.; Välimäki, M. Effectiveness of Non-Pharmacological Interventions on the Management of Sarcopenic Obesity: A Systematic Review and Meta-Analysis. Exp. Gerontol. 2020, 135, 110937.
- Antoniak, A.E.; Greig, C.A. The Effect of Combined Resistance Exercise Training and Vitamin D3 Supplementation on Musculoskeletal Health and Function in Older Adults: A Systematic Review and Meta-Analysis. BMJ Open 2017, 7, e014619.
- Cheng, S.-H.; Chen, K.-H.; Chen, C.; Chu, W.-C.; Kang, Y.-N. The Optimal Strategy of Vitamin D for Sarcopenia: A Network Meta-Analysis of Randomized Controlled Trials. Nutrients 2021, 13, 3589.
- Cintoni, M.; Grassi, F.; Palombaro, M.; Rinninella, E.; Pulcini, G.; Di Donato, A.; Salvatore, L.; Quero, G.; Tortora, G.; Alfieri, S.; et al. Nutritional Interventions during Chemotherapy for Pancreatic Cancer: A Systematic Review of Prospective Studies. Nutrients 2023, 15, 727.
- Bozzetti, F. Nutritional Interventions in Elderly Gastrointestinal Cancer Patients: The Evidence from Randomized Controlled Trials. Support Care Cancer 2019, 27, 721–727.
- Johnston, H.E.; Takefala, T.G.; Kelly, J.T.; Keating, S.E.; Coombes, J.S.; Macdonald, G.A.; Hickman, I.J.; Mayr, H.L. The Effect of Diet and Exercise Interventions on Body Composition in Liver Cirrhosis: A Systematic Review. Nutrients 2022, 14, 3365.
- Lu, Y.; Wang, Y.-J.; Lu, Q. The Effect of Oral Nutritional Supplement on Muscle Fitness of Patients Undergoing Dialysis: A Systematic Review and Meta-Analysis. J. Adv. Nurs. 2021, 77, 1716–1730.
- Bischoff, S.C.; Bernal, W.; Dasarathy, S.; Merli, M.; Plank, L.D.; Schütz, T.; Plauth, M. ESPEN Practical Guideline: Clinical Nutrition in Liver Disease. Clin. Nutr. 2020, 39, 3533–3562.
- Bischoff, S.C.; Barazzoni, R.; Busetto, L.; Campmans-Kuijpers, M.; Cardinale, V.; Chermesh, I.; Eshraghian, A.; Kani, H.T.; Khannoussi, W.; Lacaze, L.; et al. European Guideline on Obesity Care in Patients with Gastrointestinal and Liver Diseases—Joint ESPEN/UEG Guideline. Clin. Nutr. 2022, 41, 2364–2405.
- Liu, C.; Xu, H.; Chen, L.; Zhu, M. Exercise and Nutritional Intervention for Physical Function of the Prefrail: A Systematic Review and Meta-Analysis. J. Am. Med. Dir. Assoc. 2022, 23, 1431.e1–1431.e19.
- Sun, X.; Liu, W.; Gao, Y.; Qin, L.; Feng, H.; Tan, H.; Chen, Q.; Peng, L.; Wu, I.X.Y. Comparative Effectiveness of Non-Pharmacological Interventions for Frailty: A Systematic Review and Network Meta-Analysis. Age Ageing 2023, 52, afad004.
- De Moraes, M.B.; Avgerinou, C.; Fukushima, F.B.; Vidal, E.I.O. Nutritional Interventions for the Management of Frailty in Older Adults: Systematic Review and Meta-Analysis of Randomized Clinical Trials. Nutr. Rev. 2021, 79, 889–913.
- Thomson, K.; Rice, S.; Arisa, O.; Johnson, E.; Tanner, L.; Marshall, C.; Sotire, T.; Richmond, C.; O’Keefe, H.; Mohammed, W.; et al. Oral Nutritional Interventions in Frail Older People Who Are Malnourished or at Risk of Malnutrition: A Systematic Review. Health Technol. Assess 2022, 26, 1–112.
- Han, C.Y.; Miller, M.; Yaxley, A.; Baldwin, C.; Woodman, R.; Sharma, Y. Effectiveness of Combined Exercise and Nutrition Interventions in Prefrail or Frail Older Hospitalised Patients: A Systematic Review and Meta-Analysis. BMJ Open 2020, 10, e040146.
- Lorbergs, A.L.; Prorok, J.C.; Holroyd-Leduc, J.; Bouchard, D.R.; Giguere, A.; Gramlich, L.; Keller, H.; Tang, A.; Racey, M.; Ali, M.U.; et al. Nutrition and Physical Activity Clinical Practice Guidelines for Older Adults Living with Frailty. J. Frailty Aging 2022, 11, 3–11.
- Hwang, S.-H.; Lee, D.H.; Min, J.; Jeon, J.Y. Handgrip Strength as a Predictor of All-Cause Mortality in Patients with Chronic Kidney Disease Undergoing Dialysis: A Meta-Analysis of Prospective Cohort Studies. J. Ren. Nutr. 2019, 29, 471–479.
- Santana Gomes, T.; do Espirito Santo Silva, D.; Xavier Junior, G.F.; de Farias Costa, P.R.; Gusmão Sena, M.H.L.; Barreto Medeiros, J.M. Sarcopenia and Mortality in Patients with Chronic Non-Dialytic Renal Disease: Systematic Review and Meta-Analysis. J. Ren. Nutr. 2022, 32, 135–143.
- Kojima, G. Prevalence of Frailty in End-Stage Renal Disease: A Systematic Review and Meta-Analysis. Int. Urol. Nephrol. 2017, 49, 1989–1997.
- Takahashi, F.; Hashimoto, Y.; Kaji, A.; Sakai, R.; Kawate, Y.; Okamura, T.; Kitagawa, N.; Okada, H.; Nakanishi, N.; Majima, S.; et al. Association between Geriatric Nutrition Risk Index and The Presence of Sarcopenia in People with Type 2 Diabetes Mellitus: A Cross-Sectional Study. Nutrients 2021, 13, 3729.
- Wang, M.; Tan, Y.; Shi, Y.; Wang, X.; Liao, Z.; Wei, P. Diabetes and Sarcopenic Obesity: Pathogenesis, Diagnosis, and Treatments. Front. Endocrinol. 2020, 11, 568.
- Izzo, A.; Massimino, E.; Riccardi, G.; Della Pepa, G. A Narrative Review on Sarcopenia in Type 2 Diabetes Mellitus: Prevalence and Associated Factors. Nutrients 2021, 13, 183.
- Velázquez-Alva, M.C.; Irigoyen-Camacho, M.E.; Zepeda-Zepeda, M.A.; Lazarevich, I.; Arrieta-Cruz, I.; D’Hyver, C. Sarcopenia, Nutritional Status and Type 2 Diabetes Mellitus: A Cross-Sectional Study in a Group of Mexican Women Residing in a Nursing Home. Nutr. Diet. 2020, 77, 515–522.
- Shiroma, K.; Tanabe, H.; Takiguchi, Y.; Yamaguchi, M.; Sato, M.; Saito, H.; Tanaka, K.; Masuzaki, H.; Kazama, J.J.; Shimabukuro, M. A Nutritional Assessment Tool, GNRI, Predicts Sarcopenia and Its Components in Type 2 Diabetes Mellitus: A Japanese Cross-Sectional Study. Front. Nutr. 2023, 10, 1087471.
- Dai, S.; Shu, D.; Meng, F.; Chen, Y.; Wang, J.; Liu, X.; Xiao, X.; Guo, W.; Chen, F. Higher Risk of Sarcopenia in Older Adults with Type 2 Diabetes: NHANES 1999–2018. Obes. Facts 2023, 16, 237–248.
- Su, Y.; Yuki, M.; Otsuki, M. Prevalence of Stroke-Related Sarcopenia: A Systematic Review and Meta-Analysis. J. Stroke Cerebrovasc. Dis. 2020, 29, 105092.
- Beckwée, D.; Cuypers, L.; Lefeber, N.; De Keersmaecker, E.; Scheys, E.; Van Hees, W.; Perkisas, S.; De Raedt, S.; Kerckhofs, E.; Bautmans, I.; et al. Skeletal Muscle Changes in the First Three Months of Stroke Recovery: A Systematic Review. J. Rehabil. Med. 2022, 54, jrm00308.
- Harvey, N.C.; Orwoll, E.; Kwok, T.; Karlsson, M.K.; Rosengren, B.E.; Ribom, E.; Cauley, J.A.; Cawthon, P.M.; Ensrud, K.; Liu, E.; et al. Sarcopenia Definitions as Predictors of Fracture Risk Independent of FRAX®, Falls, and BMD in the Osteoporotic Fractures in Men (MrOS) Study: A Meta-Analysis. J. Bone Miner. Res. 2021, 36, 1235–1244.
- Kunutsor, S.K.; Seidu, S.; Voutilainen, A.; Blom, A.W.; Laukkanen, J.A. Handgrip Strength-a Risk Indicator for Future Fractures in the General Population: Findings from a Prospective Study and Meta-Analysis of 19 Prospective Cohort Studies. Geroscience 2021, 43, 869–880.
- Gandham, A.; Mesinovic, J.; Jansons, P.; Zengin, A.; Bonham, M.P.; Ebeling, P.R.; Scott, D. Falls, Fractures, and Areal Bone Mineral Density in Older Adults with Sarcopenic Obesity: A Systematic Review and Meta-Analysis. Obes. Rev. 2021, 22, e13187.
- Volkert, D.; Beck, A.M.; Cederholm, T.; Cruz-Jentoft, A.; Goisser, S.; Hooper, L.; Kiesswetter, E.; Maggio, M.; Raynaud-Simon, A.; Sieber, C.C.; et al. ESPEN Guideline on Clinical Nutrition and Hydration in Geriatrics. Clin. Nutr. 2019, 38, 10–47.
- Jiang, Z.; Zhang, X.; Yang, L.; Li, Z.; Qin, W. Effect of Restricted Protein Diet Supplemented with Keto Analogues in Chronic Kidney Disease: A Systematic Review and Meta-Analysis. Int. Urol. Nephrol. 2016, 48, 409–418.
- Rhee, C.M.; Ahmadi, S.-F.; Kovesdy, C.P.; Kalantar-Zadeh, K. Low-Protein Diet for Conservative Management of Chronic Kidney Disease: A Systematic Review and Meta-Analysis of Controlled Trials. J. Cachexia Sarcopenia Muscle 2018, 9, 235–245.
- Yan, B.; Su, X.; Xu, B.; Qiao, X.; Wang, L. Effect of Diet Protein Restriction on Progression of Chronic Kidney Disease: A Systematic Review and Meta-Analysis. PLoS ONE 2018, 13, e0206134.
- Chewcharat, A.; Takkavatakarn, K.; Wongrattanagorn, S.; Panrong, K.; Kittiskulnam, P.; Eiam-Ong, S.; Susantitaphong, P. The Effects of Restricted Protein Diet Supplemented with Ketoanalogue on Renal Function, Blood Pressure, Nutritional Status, and Chronic Kidney Disease-Mineral and Bone Disorder in Chronic Kidney Disease Patients: A Systematic Review and Meta-Analysis. J. Ren. Nutr. 2020, 30, 189–199.
- Shi, H.; Chen, H.; Zhang, Y.; Li, J.; Fu, K.; Xue, W.; Teng, W.; Tian, L. 25-Hydroxyvitamin D Level, Vitamin D Intake, and Risk of Stroke: A Dose-Response Meta-Analysis. Clin. Nutr. 2020, 39, 2025–2034.
- Vergatti, A.; Abate, V.; Zarrella, A.F.; Manganelli, F.; Tozza, S.; Iodice, R.; De Filippo, G.; D’Elia, L.; Strazzullo, P.; Rendina, D. 25-Hydroxy-Vitamin D and Risk of Recurrent Stroke: A Dose Response Meta-Analysis. Nutrients 2023, 15, 512.
- Dai, Z.; McKenzie, J.E.; McDonald, S.; Baram, L.; Page, M.J.; Allman-Farinelli, M.; Raubenheimer, D.; Bero, L.A. Assessment of the Methods Used to Develop Vitamin D and Calcium Recommendations-A Systematic Review of Bone Health Guidelines. Nutrients 2021, 13, 2423.
- Kazemian, E.; Pourali, A.; Sedaghat, F.; Karimi, M.; Basirat, V.; Sajadi Hezaveh, Z.; Davoodi, S.H.; Holick, M.F. Effect of Supplemental Vitamin D3 on Bone Mineral Density: A Systematic Review and Meta-Analysis. Nutr. Rev. 2023, 81, 511–530.
- Ni, H.; Zhang, S.; Niu, X.; Dai, S. Meta-Analysis of Effects of Nutritional Intervention Combined with Calcium Carbonate D3 Tablets on Bone Mineral Density, Bone Metabolism, and Curative Effect in Patients with Osteoporosis. Contrast Media Mol. Imaging 2022, 2022, 3670007.
- Feng, Y.; Cheng, G.; Wang, H.; Chen, B. The Associations between Serum 25-Hydroxyvitamin D Level and the Risk of Total Fracture and Hip Fracture. Osteoporos. Int. 2017, 28, 1641–1652.
- Wang, N.; Chen, Y.; Ji, J.; Chang, J.; Yu, S.; Yu, B. The Relationship between Serum Vitamin D and Fracture Risk in the Elderly: A Meta-Analysis. J. Orthop. Surg. Res. 2020, 15, 81.
- Habibi Ghahfarrokhi, S.; Mohammadian-Hafshejani, A.; Sherwin, C.M.T.; Heidari-Soureshjani, S. Relationship between Serum Vitamin D and Hip Fracture in the Elderly: A Systematic Review and Meta-Analysis. J. Bone Miner. Metab. 2022, 40, 541–553.
- Weaver, C.M.; Alexander, D.D.; Boushey, C.J.; Dawson-Hughes, B.; Lappe, J.M.; LeBoff, M.S.; Liu, S.; Looker, A.C.; Wallace, T.C.; Wang, D.D. Calcium plus Vitamin D Supplementation and Risk of Fractures: An Updated Meta-Analysis from the National Osteoporosis Foundation. Osteoporos. Int. 2016, 27, 367–376.
- Kong, S.H.; Jang, H.N.; Kim, J.H.; Kim, S.W.; Shin, C.S. Effect of Vitamin D Supplementation on Risk of Fractures and Falls According to Dosage and Interval: A Meta-Analysis. Endocrinol. Metab. 2022, 37, 344–358.
- Manoj, P.; Derwin, R.; George, S. What Is the Impact of Daily Oral Supplementation of Vitamin D3 (Cholecalciferol) plus Calcium on the Incidence of Hip Fracture in Older People? A Systematic Review and Meta-Analysis. Int. J. Older People Nurs. 2023, 18, e12492.
- Banerjee, D.; Chitalia, N.; Ster, I.C.; Appelbaum, E.; Thadhani, R.; Kaski, J.C.; Goldsmith, D. Impact of Vitamin D on Cardiac Structure and Function in Chronic Kidney Disease Patients with Hypovitaminosis D: A Randomized Controlled Trial and Meta-Analysis. Eur. Heart J. Cardiovasc. Pharm. 2021, 7, 302–311.
- Christodoulou, M.; Aspray, T.J.; Schoenmakers, I. Vitamin D Supplementation for Patients with Chronic Kidney Disease: A Systematic Review and Meta-Analyses of Trials Investigating the Response to Supplementation and an Overview of Guidelines. Calcif. Tissue Int. 2021, 109, 157–178.
- Karimi, E.; Bitarafan, S.; Mousavi, S.M.; Zargarzadeh, N.; Mokhtari, P.; Hawkins, J.; Meysamie, A.; Koohdani, F. The Effect of Vitamin D Supplementation on Fibroblast Growth Factor-23 in Patients with Chronic Kidney Disease: A Systematic Review and Meta-Analysis. Phytother. Res. 2021, 35, 5339–5351.
- Milajerdi, A.; Ostadmohammadi, V.; Amirjani, S.; Kolahdooz, F.; Asemi, Z. The Effects of Vitamin D Treatment on Glycemic Control, Serum Lipid Profiles, and C-Reactive Protein in Patients with Chronic Kidney Disease: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Int. Urol. Nephrol. 2019, 51, 1567–1580.
- Chai, B.; Gao, F.; Wu, R.; Dong, T.; Gu, C.; Lin, Q.; Zhang, Y. Vitamin D Deficiency as a Risk Factor for Dementia and Alzheimer’s Disease: An Updated Meta-Analysis. BMC Neurol. 2019, 19, 284.
- Jayedi, A.; Rashidy-Pour, A.; Shab-Bidar, S. Vitamin D Status and Risk of Dementia and Alzheimer’s Disease: A Meta-Analysis of Dose-Response. Nutr. Neurosci. 2019, 22, 750–759.
- Kalra, A.; Teixeira, A.L.; Diniz, B.S. Association of Vitamin D Levels with Incident All-Cause Dementia in Longitudinal Observational Studies: A Systematic Review and Meta-Analysis. J. Prev. Alzheimer’s Dis. 2020, 7, 14–20.
- Sanz-París, A.; Gómez-Candela, C.; Martín-Palmero, Á.; García-Almeida, J.M.; Burgos-Pelaez, R.; Matía-Martin, P.; Arbones-Mainar, J.M.; Study VIDA group. Application of the New ESPEN Definition of Malnutrition in Geriatric Diabetic Patients during Hospitalization: A Multicentric Study. Clin. Nutr. 2016, 35, 1564–1567.
- Sánchez-Rodríguez, D.; Marco, E.; Ronquillo-Moreno, N.; Miralles, R.; Vázquez-Ibar, O.; Escalada, F.; Muniesa, J.M. Prevalence of Malnutrition and Sarcopenia in a Post-Acute Care Geriatric Unit: Applying the New ESPEN Definition and EWGSOP Criteria. Clin. Nutr. 2017, 36, 1339–1344.
- Sanz-París, A.; Martín-Palmero, A.; Gomez-Candela, C.; García-Almeida, J.M.; Burgos-Pelaez, R.; Sanz-Arque, A.; Espina, S.; Arbones-Mainar, J.M. Study VIDA group GLIM Criteria at Hospital Admission Predict 8-Year All-Cause Mortality in Elderly Patients with Type 2 Diabetes Mellitus: Results From VIDA Study. JPEN J. Parenter. Enteral. Nutr. 2020, 44, 1492–1500.
- Wang, L.; Zhang, D.; Xu, J. Association between the Geriatric Nutritional Risk Index, Bone Mineral Density and Osteoporosis in Type 2 Diabetes Patients. J. Diabetes Investig. 2020, 11, 956–963.
- Çakmak, G.; Ganidağlı, S.; Efendioğlu, E.M.; Öztürk, E.; Öztürk, Z.A. Do Long-Term Complications of Type 2 Diabetes Increase Susceptibility to Geriatric Syndromes in Older Adults? Medicina 2021, 57, 968.
- López-Gómez, J.J.; Gutiérrez-Lora, C.; Izaola-Jauregui, O.; Primo-Martín, D.; Gómez-Hoyos, E.; Jiménez-Sahagún, R.; De Luis-Román, D.A. Real World Practice Study of the Effect of a Specific Oral Nutritional Supplement for Diabetes Mellitus on the Morphofunctional Assessment and Protein Energy Requirements. Nutrients 2022, 14, 4802.
- Matsuura, S.; Shibazaki, K.; Uchida, R.; Imai, Y.; Mukoyama, T.; Shibata, S.; Morita, H. Sarcopenia Is Associated with the Geriatric Nutritional Risk Index in Elderly Patients with Poorly Controlled Type 2 Diabetes Mellitus. J. Diabetes Investig. 2022, 13, 1366–1373.
- Petroni, M.L.; Brodosi, L.; Marchignoli, F.; Sasdelli, A.S.; Caraceni, P.; Marchesini, G.; Ravaioli, F. Nutrition in Patients with Type 2 Diabetes: Present Knowledge and Remaining Challenges. Nutrients 2021, 13, 2748.
- Wang, X.; Wu, W.; Zheng, W.; Fang, X.; Chen, L.; Rink, L.; Min, J.; Wang, F. Zinc Supplementation Improves Glycemic Control for Diabetes Prevention and Management: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Am. J. Clin. Nutr. 2019, 110, 76–90.
- Wang, Z.; Ronsmans, C.; Woolf, B. Triangulating Evidence for the Causal Impact of Single-Intervention Zinc Supplement on Glycaemic Control for Type 2 Diabetes: Systematic Review and Meta-Analysis of Randomised Controlled Trial and Two-Sample Mendelian Randomisation. Br. J. Nutr. 2023, 129, 1929–1944.
- Asbaghi, O.; Nazarian, B.; Yousefi, M.; Anjom-Shoae, J.; Rasekhi, H.; Sadeghi, O. Effect of Vitamin E Intake on Glycemic Control and Insulin Resistance in Diabetic Patients: An Updated Systematic Review and Meta-Analysis of Randomized Controlled Trials. Nutr. J. 2023, 22, 10.
- Lind, M.V.; Lauritzen, L.; Kristensen, M.; Ross, A.B.; Eriksen, J.N. Effect of Folate Supplementation on Insulin Sensitivity and Type 2 Diabetes: A Meta-Analysis of Randomized Controlled Trials. Am. J. Clin. Nutr. 2019, 109, 29–42.
- Yousefi Rad, E.; Nazarian, B.; Saboori, S.; Falahi, E.; Hekmatdoost, A. Effects of L-Arginine Supplementation on Glycemic Profile: Evidence from a Systematic Review and Meta-Analysis of Clinical Trials. J. Integr. Med. 2020, 18, 284–291.
- Karimi, E.; Hatami, E.; Ghavami, A.; Hadi, A.; Darand, M.; Askari, G. Effects of L-Arginine Supplementation on Biomarkers of Glycemic Control: A Systematic Review and Meta-Analysis of Randomised Clinical Trials. Arch. Physiol. Biochem. 2023, 129, 700–710.
- Reynolds, A.N.; Akerman, A.P.; Mann, J. Dietary Fibre and Whole Grains in Diabetes Management: Systematic Review and Meta-Analyses. PLoS Med. 2020, 17, e1003053.
- De Gennaro Colonna, V.; Bianchi, M.; Pascale, V.; Ferrario, P.; Morelli, F.; Pascale, W.; Tomasoni, L.; Turiel, M. Asymmetric Dimethylarginine (ADMA): An Endogenous Inhibitor of Nitric Oxide Synthase and a Novel Cardiovascular Risk Molecule. Med. Sci. Monit. 2009, 15, RA91–RA101.
- Liu, J.; Li, C.; Chen, W.; He, K.; Ma, H.; Ma, B.; Zhao, P.; Tian, L. Relationship between Serum Asymmetric Dimethylarginine Level and Microvascular Complications in Diabetes Mellitus: A Meta-Analysis. Biomed. Res. Int. 2019, 2019, 2941861.
- Sener, A.; Lebrun, P.; Blachier, F.; Malaisse, W.J. Stimulus-Secretion Coupling of Arginine-Induced Insulin Release: Insulinotropic Action of Agmatine. Biochem. Pharmacol. 1989, 38, 327–330.
- Khan, M.S.; Khan, F.; Fonarow, G.C.; Sreenivasan, J.; Greene, S.J.; Khan, S.U.; Usman, M.S.; Vaduganathan, M.; Fudim, M.; Anker, S.D.; et al. Dietary Interventions and Nutritional Supplements for Heart Failure: A Systematic Appraisal and Evidence Map. Eur. J. Heart Fail. 2021, 23, 1468–1476.
- Bianchi, V.E. Nutrition in Chronic Heart Failure Patients: A Systematic Review. Heart Fail. Rev. 2020, 25, 1017–1026.
- Esposito, K.; Maiorino, M.I.; Bellastella, G.; Chiodini, P.; Panagiotakos, D.; Giugliano, D. A Journey into a Mediterranean Diet and Type 2 Diabetes: A Systematic Review with Meta-Analyses. BMJ Open 2015, 5, e008222.
- Becerra-Tomás, N.; Blanco Mejía, S.; Viguiliouk, E.; Khan, T.; Kendall, C.W.C.; Kahleova, H.; Rahelić, D.; Sievenpiper, J.L.; Salas-Salvadó, J. Mediterranean Diet, Cardiovascular Disease and Mortality in Diabetes: A Systematic Review and Meta-Analysis of Prospective Cohort Studies and Randomized Clinical Trials. Crit. Rev. Food Sci. Nutr. 2020, 60, 1207–1227.
- Diabetes and Nutrition Study Group (DNSG) of the European Association for the Study of Diabetes (EASD). Evidence-Based European Recommendations for the Dietary Management of Diabetes. Diabetologia 2023, 66, 965–985.
- Buckinx, F.; Aubertin-Leheudre, M. Nutrition to Prevent or Treat Cognitive Impairment in Older Adults: A GRADE Recommendation. J. Prev. Alzheimer’s Dis. 2021, 8, 110–116.
- Fu, J.; Tan, L.-J.; Lee, J.E.; Shin, S. Association between the Mediterranean Diet and Cognitive Health among Healthy Adults: A Systematic Review and Meta-Analysis. Front. Nutr. 2022, 9, 946361.
- Kunutsor, S.K.; Laukkanen, J.A.; Whitehouse, M.R.; Blom, A.W. Adherence to a Mediterranean-Style Diet and Incident Fractures: Pooled Analysis of Observational Evidence. Eur. J. Nutr. 2018, 57, 1687–1700.
- Malmir, H.; Saneei, P.; Larijani, B.; Esmaillzadeh, A. Adherence to Mediterranean Diet in Relation to Bone Mineral Density and Risk of Fracture: A Systematic Review and Meta-Analysis of Observational Studies. Eur. J. Nutr. 2018, 57, 2147–2160.
- Bernasconi, A.A.; Wiest, M.M.; Lavie, C.J.; Milani, R.V.; Laukkanen, J.A. Effect of Omega-3 Dosage on Cardiovascular Outcomes: An Updated Meta-Analysis and Meta-Regression of Interventional Trials. Mayo Clin. Proc. 2021, 96, 304–313.
- McGrattan, A.; van Aller, C.; Narytnyk, A.; Reidpath, D.; Keage, H.; Mohan, D.; Su, T.T.; Stephan, B.; Robinson, L.; Siervo, M.; et al. Nutritional Interventions for the Prevention of Cognitive Impairment and Dementia in Developing Economies in East-Asia: A Systematic Review and Meta-Analysis. Crit. Rev. Food Sci. Nutr. 2022, 62, 1838–1855.
- Yang, L.; Zhao, F.; Sun, Y.; Wang, Z.; Li, Q.; Wang, H.; Lu, Y. N-3 Polyunsaturated Fatty Acids in Elderly with Mild Cognitive Impairment: A Systemic Review and Meta-Analysis. J. Alzheimer’s Dis. 2023, 1–15.
- Chen, L.; Li, Q.; Fang, X.; Wang, X.; Min, J.; Wang, F. Dietary Intake of Homocysteine Metabolism-Related B-Vitamins and the Risk of Stroke: A Dose-Response Meta-Analysis of Prospective Studies. Adv. Nutr. 2020, 11, 1510–1528.
- Cheng, P.; Wang, L.; Ning, S.; Liu, Z.; Lin, H.; Chen, S.; Zhu, J. Vitamin E Intake and Risk of Stroke: A Meta-Analysis. Br. J. Nutr. 2018, 120, 1181–1188.
- Gil Martínez, V.; Avedillo Salas, A.; Santander Ballestín, S. Vitamin Supplementation and Dementia: A Systematic Review. Nutrients 2022, 14, 1033.
- Malmir, H.; Shab-Bidar, S.; Djafarian, K. Vitamin C Intake in Relation to Bone Mineral Density and Risk of Hip Fracture and Osteoporosis: A Systematic Review and Meta-Analysis of Observational Studies. Br. J. Nutr. 2018, 119, 847–858.
- Ma, M.-L.; Ma, Z.-J.; He, Y.-L.; Sun, H.; Yang, B.; Ruan, B.-J.; Zhan, W.; Li, S.-X.; Dong, H.; Wang, Y.-X. Efficacy of Vitamin K2 in the Prevention and Treatment of Postmenopausal Osteoporosis: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Public Health 2022, 10, 979649.
- Zhang, X.; Zhang, R.; Moore, J.B.; Wang, Y.; Yan, H.; Wu, Y.; Tan, A.; Fu, J.; Shen, Z.; Qin, G.; et al. The Effect of Vitamin A on Fracture Risk: A Meta-Analysis of Cohort Studies. Int. J. Environ. Res. Public Health 2017, 14, 1043.
- Sun, Y.; Liu, C.; Bo, Y.; You, J.; Zhu, Y.; Duan, D.; Cui, H.; Lu, Q. Dietary Vitamin C Intake and the Risk of Hip Fracture: A Dose-Response Meta-Analysis. Osteoporos. Int. 2018, 29, 79–87.
- Global BMI Mortality Collaboration; Di Angelantonio, E.; Bhupathiraju, S.; Wormser, D.; Gao, P.; Kaptoge, S.; Berrington de Gonzalez, A.; Cairns, B.; Huxley, R.; Jackson, C.; et al. Body-Mass Index and All-Cause Mortality: Individual-Participant-Data Meta-Analysis of 239 Prospective Studies in Four Continents. Lancet 2016, 388, 776–786.
- Powell-Wiley, T.M.; Poirier, P.; Burke, L.E.; Després, J.-P.; Gordon-Larsen, P.; Lavie, C.J.; Lear, S.A.; Ndumele, C.E.; Neeland, I.J.; Sanders, P.; et al. Obesity and Cardiovascular Disease: A Scientific Statement from the American Heart Association. Circulation 2021, 143, e984–e1010.
- Strazzullo, P.; D’Elia, L.; Cairella, G.; Garbagnati, F.; Cappuccio, F.P.; Scalfi, L. Excess Body Weight and Incidence of Stroke: Meta-Analysis of Prospective Studies with 2 Million Participants. Stroke 2010, 41, e418–e426.
- Lee, C.M.; Woodward, M.; Batty, G.D.; Beiser, A.S.; Bell, S.; Berr, C.; Bjertness, E.; Chalmers, J.; Clarke, R.; Dartigues, J.-F.; et al. Association of Anthropometry and Weight Change with Risk of Dementia and Its Major Subtypes: A Meta-Analysis Consisting 2.8 Million Adults with 57 294 Cases of Dementia. Obes. Rev. 2020, 21, e12989.
- Tang, X.; Zhao, W.; Lu, M.; Zhang, X.; Zhang, P.; Xin, Z.; Sun, R.; Tian, W.; Cardoso, M.A.; Yang, J.; et al. Relationship between Central Obesity and the Incidence of Cognitive Impairment and Dementia from Cohort Studies Involving 5,060,687 Participants. Neurosci. Biobehav. Rev. 2021, 130, 301–313.
- Sadeghi, O.; Saneei, P.; Nasiri, M.; Larijani, B.; Esmaillzadeh, A. Abdominal Obesity and Risk of Hip Fracture: A Systematic Review and Meta-Analysis of Prospective Studies. Adv. Nutr. 2017, 8, 728–738.
- Zahedi, H.; Atayie, F.; Samii Kondrud, F.; Balali, A.; Beyene, J.; Tahery, N.; Asadi, M.; Sadeghi, O. Associations of Abdominal Obesity with Different Types of Bone Fractures in Adults: A Systematic Review and Dose-Response Meta-Analysis of Prospective Cohort Studies. Crit. Rev. Food Sci. Nutr. 2023, 21, 6456.
- Forlivesi, S.; Cappellari, M.; Bonetti, B. Obesity Paradox and Stroke: A Narrative Review. Eat Weight. Disord. 2021, 26, 417–423.
- Csige, I.; Ujvárosy, D.; Szabó, Z.; Lőrincz, I.; Paragh, G.; Harangi, M.; Somodi, S. The Impact of Obesity on the Cardiovascular System. J. Diabetes Res. 2018, 2018, 3407306.
- Kaiser, M.J.; Bauer, J.M.; Rämsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.S.; Charlton, K.E.; Maggio, M.; et al. Frequency of Malnutrition in Older Adults: A Multinational Perspective Using the Mini Nutritional Assessment. J. Am. Geriatr. Soc. 2010, 58, 1734–1738.
- Crichton, M.; Craven, D.; Mackay, H.; Marx, W.; de van der Schueren, M.; Marshall, S. A Systematic Review, Meta-Analysis and Meta-Regression of the Prevalence of Protein-Energy Malnutrition: Associations with Geographical Region and Sex. Age Ageing 2019, 48, 38–48.
- Vellas, B.; Villars, H.; Abellan, G.; Soto, M.E.; Rolland, Y.; Guigoz, Y.; Morley, J.E.; Chumlea, W.; Salva, A.; Rubenstein, L.Z.; et al. Overview of the MNA—Its History and Challenges. J. Nutr. Health Aging 2006, 10, 456–463, discussion 463–465.
- Kaiser, M.J.; Bauer, J.M.; Ramsch, C.; Uter, W.; Guigoz, Y.; Cederholm, T.; Thomas, D.R.; Anthony, P.; Charlton, K.E.; Maggio, M.; et al. Validation of the Mini Nutritional Assessment Short-Form (MNA-SF): A Practical Tool for Identification of Nutritional Status. J. Nutr. Health Aging 2009, 13, 782–788.
- Cederholm, T.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Fukushima, R.; Higashiguchi, T.; Baptista, G.; Barazzoni, R.; Blaauw, R.; Coats, A.; et al. GLIM Criteria for the Diagnosis of Malnutrition—A Consensus Report from the Global Clinical Nutrition Community. Clin. Nutr. 2019, 38, 207–217.
- Barazzoni, R.; Jensen, G.L.; Correia, M.I.T.D.; Gonzalez, M.C.; Higashiguchi, T.; Shi, H.P.; Bischoff, S.C.; Boirie, Y.; Carrasco, F.; Cruz-Jentoft, A.; et al. Guidance for Assessment of the Muscle Mass Phenotypic Criterion for the Global Leadership Initiative on Malnutrition (GLIM) Diagnosis of Malnutrition. Clin. Nutr. 2022, 41, 1425–1433.
- Compher, C.; Cederholm, T.; Correia, M.I.T.D.; Gonzalez, M.C.; Higashiguch, T.; Shi, H.P.; Bischoff, S.C.; Boirie, Y.; Carrasco, F.; Cruz-Jentoft, A.; et al. Guidance for Assessment of the Muscle Mass Phenotypic Criterion for the Global Leadership Initiative on Malnutrition Diagnosis of Malnutrition. JPEN J. Parenter. Enteral. Nutr. 2022, 46, 1232–1242.
- He, J.; Zhang, P.; Shen, L.; Niu, L.; Tan, Y.; Chen, L.; Zhao, Y.; Bai, L.; Hao, X.; Li, X.; et al. Short-Chain Fatty Acids and Their Association with Signalling Pathways in Inflammation, Glucose and Lipid Metabolism. Int. J. Mol. Sci. 2020, 21, 6356.
- Huda, M.N.; Kim, M.; Bennett, B.J. Modulating the Microbiota as a Therapeutic Intervention for Type 2 Diabetes. Front. Endocrinol. 2021, 12, 632335.
- Voroneanu, L.; Burlacu, A.; Brinza, C.; Covic, A.; Balan, G.G.; Nistor, I.; Popa, C.; Hogas, S.; Covic, A. Gut Microbiota in Chronic Kidney Disease: From Composition to Modulation towards Better Outcomes-A Systematic Review. J. Clin. Med. 2023, 12, 1948.
- Li, Y.J.; Chen, X.; Kwan, T.K.; Loh, Y.W.; Singer, J.; Liu, Y.; Ma, J.; Tan, J.; Macia, L.; Mackay, C.R.; et al. Dietary Fiber Protects against Diabetic Nephropathy through Short-Chain Fatty Acid-Mediated Activation of G Protein-Coupled Receptors GPR43 and GPR109A. J. Am. Soc. Nephrol. 2020, 31, 1267–1281.
- Chiavaroli, L.; Mirrahimi, A.; Sievenpiper, J.L.; Jenkins, D.J.A.; Darling, P.B. Dietary Fiber Effects in Chronic Kidney Disease: A Systematic Review and Meta-Analysis of Controlled Feeding Trials. Eur. J. Clin. Nutr. 2015, 69, 761–768.
- McFarlane, C.; Ramos, C.I.; Johnson, D.W.; Campbell, K.L. Prebiotic, Probiotic, and Synbiotic Supplementation in Chronic Kidney Disease: A Systematic Review and Meta-Analysis. J. Ren. Nutr. 2019, 29, 209–220.
