Systemic lupus erythematosus (SLE), the prototype of systemic autoimmune diseases is characterized by extreme heterogeneity with a variable clinical course. Renal involvement may be observed and affects the outcome. Hydroxychloroquine should be administered to every lupus patient irrespective of organ involvement. Conventional immunosuppressive therapy includes corticosteroids, methotrexate, cyclophosphamide, mycophenolate mofetil, azathioprine, cyclosporine and tacrolimus. However, despite conventional immunosuppressive treatment, flares occur and broad immunosuppression is accompanied by multiple side effects. Flare occurrence, target organ involvement, side effects of broad immunosuppression and increased knowledge of the pathogenetic mechanisms involved in SLE pathogenesis as well as the availability of biologic agents has led to the application of biologic agents in SLE management. Biologic agents targeting various pathogenetic paths have been applied. B cell targeting agents have been used successfully. Belimumab, a B cell targeting agent, has been approved for the treatment of SLE. Rituximab, an anti-CD20 targeting agent is also used in SLE. Anifrolumab, an interferon I receptor-targeting agent has beneficial effects on SLE. In conclusion, biologic treatment is applied in SLE and should be further evaluated with the aim of a good treatment response and a significant improvement in quality of life.
- systemic lupus erythematosus
- treatment
- hydroxychloroquine
- corticosteroids
- biologic agents
- belimumab
- rituximab
- anifrolumab
- tocilizumab
- baricitinib
1. Introduction
23. Systemic Lupus Erythematosus Treatment
2.1. Hydroxychloroquine
3.1. Hydroxychloroquine
Hydroxychloroquine, an antimalarial, when taken by soldiers during the Second World War for the prevention of malaria, was shown to improve musculoskeletal complaints. Thus, it was utilized in the treatment of rheumatic conditions. Hydroxychloroquine is now considered the standard-of-care treatment of SLE, as it was shown to significantly reduce mortality in all ethnic groups [12][13][14][13,14,15], unless there are contraindications to it [15][16][16,17]. It is utilized in the treatment of discoid lupus and SLE [17][18]. Hydroxychloroquine modulates the immune response by modulating macrophage and other antigen presenting cell function [18][19][19,20] and by blocking Toll-like receptors on dendritic cells [20][21].2.2. Glucocorticoids
3.2. Glucocorticoids
Glucocorticoids are used in SLE at every dose level, including large, medium and small doses. Large bolus doses may be used as needed in cases of disease flare or target organ involvement and small doses as maintenance treatment [21][28] to reduce disease activity and disease burden accumulation. They act via a genomic pathway, involving transrepressive and transactivating modes of action on the cell nucleus, and via a non-genomic pathway [22][29]. However, they induce broad immunosuppression, and their use is accompanied by side effects.2.3. Azathioprine
3.3. Azathioprine
Azathioprine is administered in SLE as a conventional immunosuppressive agent that aids in steroid sparing. It may be administered as maintenance treatment in renal disease in lupus [23][32] and in lupus flares. Its administration is safe during pregnancy but unsafe during lactation [24][33].2.4. Methotrexate
3.4. Methotrexate
If low dose glucocorticoids do not control the disease, methotrexate may be applied as an immunosuppressive agent, which contributes to steroid sparing [25][26][34,35]. Methotrexate has an antifolate mechanism of action [27][36]. It is indicated in lupus patients who display an inadequate response to hydroxychloroquine and in patients with cutaneous and articular involvement [28][37] without renal disease. Methotrexate enters cells through a folate transporter [26][35]. Once within the cell, methotrexate as monoglutamate forms polyglutamates, a more potent drug form which inhibits various enzymes, leading to increased adenosine levels [29][38], the decreased production of ammonium and H2O2 and decreased synthesis of purines, methionine and DNA. Adenosine is a molecule with anti-inflammatory effects [30][39].2.5. Mycophenolate Mofetil
3.5. Mycophenolate Mofetil
Mycophenolate mofetil (MMF) inhibits inosine 5-monophosphate dehydrogenase, thereby inhibiting the synthesis of guanine. Thus, B cells, T cells and fibroblasts are decreased. MMF also reduces transforming growth factor β and fibronectin synthesis, thereby exhibiting antifibrotic effects [31][43]. MMF inhibits the expression of cell adhesion molecules, thereby interfering with the recruitment of lymphocytes and monocytes in the sites of inflammation. It may also induce T cell apoptosis [32][44]. The first trial in lupus with MMF was performed in 2000. Thereafter, MMF became a standard drug for the treatment of lupus nephritis [33][45].2.6. Cyclophosphamide
3.6. Cyclophosphamide
Cyclophosphamide is an alkylating drug which acts on DNA and leads to the death of activated lymphocytes while simultaneously having a protective effect on glomeruli [34][35][55,56]. Cyclophosphamide displays side effects such as leukopenia, an increased infection risk, bladder toxicity and an increased cancer risk [36][57]. Cyclophosphamide may be applied as induction therapy for flares or target organ involvement [37][38][53,58].2.7. Calcineurin Inhibitors
3.7. Calcineurin Inhibitors
Calcineurin inhibitors tacrolimus and cyclosporine have been applied as immunosuppressives in organ transplantation. They modulate the immune response mainly by inhibiting T cell activation. Additionally, they reduce albuminuria and preserve renal function [39][59]. In SLE without renal involvement, cyclosporine contributes to lowering steroid dosage, reduced disease activity and flare prevention [40][60] by modulating T cell function [41][42][61,62].2.8. Intravenous Immunoglobulin
3.8. Intravenous Immunoglobulin
Therapeutic intravenous immunoglobulin (IVIg) is a product which contains human multi-specific immunoglobulin G. IVIg has been used successfully in lupus patients leading to a reduction in disease activity [43][70]. IVIg was shown to be effective for various manifestations in SLE. It was shown to be effective for renal disease in SLE, as well as target organ manifestations, such as thrombocytopenia, refractory neuropsychiatric lupus [44][71] and lupus myocarditis [45][72]. IVIg may act via various mechanisms, including the inhibition of autoreactive B lymphocytes [46][73].34. Biologic Treatment in Systemic Lupus Erythematosus
3.1. B Cell Targeted Treatment
4.1. B Cell Targeted Treatment
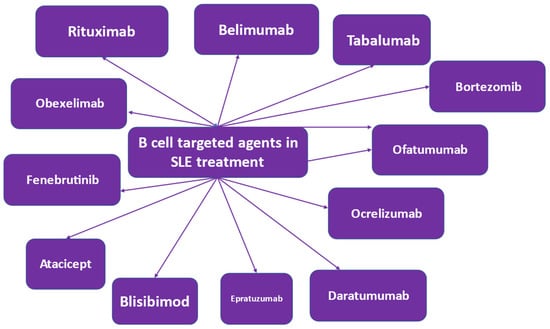
SLE pathophysiology is characterized by B cell involvement [47][48][89,90]. Therefore, various therapeutic strategies targeting the B cell have been applied [49][50][91,92]. B lymphocytes are involved in antibody-dependent and antibody-independent mechanisms in SLE pathogenesis. Autoantibodies are produced by B cells, which are self-reacting, thereby triggering an inflammatory response. In terms of health benefits, B cells produce protective antibodies [51][93]. In SLE, autoantibodies are produced, which are involved in triggering an inflammatory response via multiple mechanisms, including the induction of cytokine and interferon production by innate immune cells [52][94]. This immune mechanism is disturbed in SLE patients and is further disrupted by the abnormal functioning of other immune cells [53][95]. Novel treatment methods that target the B cell have been developed or are in development [49][50][91,92] (Figure 13).