Magnesium deficiency and stress are both common conditions among the general population, which, over time, can increase the risk of health consequences. Clinical and pre-clinical evidence suggest that stress could increase magnesium loss, causing a deficiency; and in turn, magnesium deficiency could enhance the body’s susceptibility to stress, resulting in a magnesium and stress vicious circle.
- stress
- magnesium
- hypomagnesemia
- magnesium deficiency
- vicious circle
- dietary intake
- magnesium supplementation
1. Introduction
Stress and magnesium deficiency are common health conditions among the general population[1][2]. Interestingly, clinical symptoms of magnesium deficiency and stress are very similar, notably fatigue, anxiety, irritability, nervousness, muscle cramps, gastrointestinal spasms and headache [3][4]. Of note, low magnesium status has been associated with stressful conditions, and conversely, chronic exposure to stressful stimuli results in magnesium loss [5]. This bidirectional cause-effect relationship between magnesium and stress was first described in the early 1990s [5][6] and referred to as the vicious circle. Nowadays, considerable pre-clinical and clinical evidence support the beneficial effect of magnesium supplementation in different types of stress.
2.
Magnesium: biological role and homeostasis
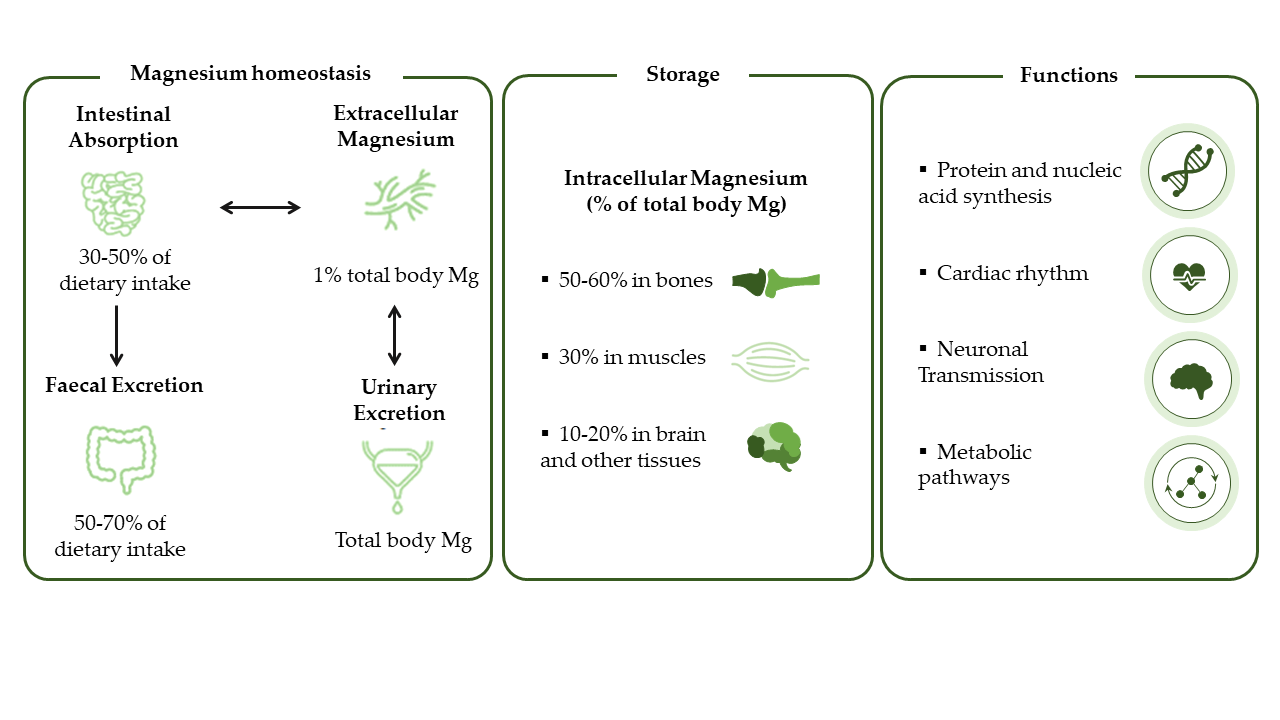
Magnesium is an essential micronutrient for humans [7] involved in almost all major metabolic and biochemical processes (Figure 1), and acting as a cofactor in hundreds of enzymatic reactions [8]. About 50–60% of body magnesium is stored in the bones, with the remainder distributed in soft tissues such as muscles [9][10] and the brain [11][12]. Only 1% of the total magnesium is extracellular and 0.3% of this circulates in serum [13]. In clinical practice, normal serum magnesium values are considered to be within the 0.7–1.0 mmol/L range [14]. Magnesium deficiency is generally defined when serum concentrations drop below 0.7 mmol/L [15].
Magnesium homeostasis is tightly regulated and relies on the dynamic balance between intestinal absorption, kidney excretion and bone storage (Figure 1) [16]. However, chronic latent magnesium deficiency (serum levels <0.85 mmol/L) may occur despite normal magnesium levels in serum and remain undetected (non-specific symptoms) with a potential long-term impact on health [7][17].
Figure 1. Magnesium homeostasis. Figure adapted from Jahnen-Dechent, 2012 [17].
Among the factors contributing to magnesium deficiency (e.g. lifestyle; some medicines; pathological conditions), clinical evidence also suggest that chronic stress may cause magnesium loss [18][19][20][21]. A recent study found that nearly half (~44%) of the subjects screened for stress had chronic latent magnesium deficiency [22].
In addition, multiple studies have consistently shown that the dietary intake of magnesium is often inadequate and does not reach the recommended dietary allowances (Table 1) [3][23][24][25] across different countries worldwide [26][27][28]. This trend is further increased by the consumption of processed food typical of Western diets, with magnesium being depleted by up to 80–90% [3][15].
Table 1. Current magnesium recommended daily allowance across countries.
|
Country |
Magnesium, mg/day |
|
|
Men |
Women |
|
|
Italy [29] |
240 |
240 |
|
Russia [30] |
300 |
300 |
|
Japan [31] |
320−340 |
220−230 |
|
Poland [32] |
400–420 |
310–320 |
|
USA and Canada [33] |
400–420 |
310–320 |
|
France [34] |
420 |
360 |
Values shown refer to adult population only (≥19 years).
3. Stress and interaction with magnesium status
Stress is considered as an ongoing and adaptive system that enables an individual to assess, cope and predict constantly changing conditions. However, the capacity of this stress system is limited and can be overloaded, resulting in poor health outcomes, particularly those related to mental illness like depression or cognitive deficits [35]. The hypothalamic-pituitary-adrenal (HPA) axis and the autonomic nervous system, comprising of sympathetic nervous system (SNS) and parasympathetic nervous system (PSN), have been identified as the mediators of the so-called “neurobiological stress model” [36][37][38]. In this model, important mediators like catecholamines (released from the sympathetic nerves and the adrenal medulla), together with the glucocorticoids (mainly cortisol, released from the adrenal cortex) regulate the stress response [36][37]. Cortisol also interacts with the serotonergic pathway and modulates the release of serotonin (5-hydroxytryptamine or 5-HT) neurotransmitter in response to acute or chronic stressors [39]. In addition to the regulation through feedback mechanisms, the HPA axis is also modulated by other central systems, particularly by the inhibitory action of the γ-aminobutyric acid (GABA), and the excitatory effect of glutamate [40].
The generalized unsafety theory of stress (GUTS) is a new psychological and cognitive theoretical model proposed by Brosschot in 2016 [41] that revises and expands the stress theory. Based on neurobiological and evolutionary evidence, GUTS hypothesizes that stressors are not necessary for a chronic stress response to occur but the perception of an unsafe state is enough. In GUTS, PNS is the key system controlling the stress response (particularly the vagus nerve and the prefrontal cortex activity) [41]
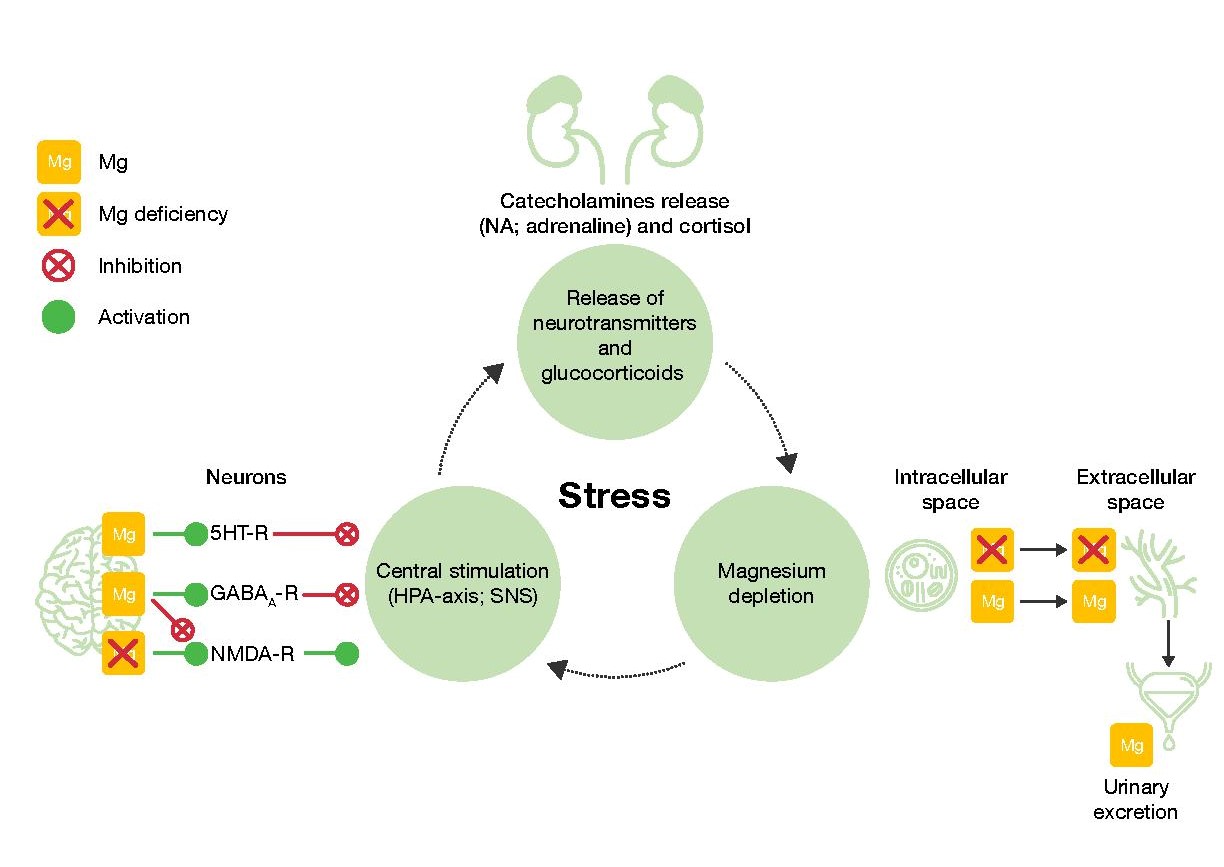
Of note, magnesium interacts with all the stress mediators mentioned above [11][42][43][44] overall serving an inhibitory function in the regulation and central neurotransmission of the stress response (neurobiological model), or by modulating the autonomic nervous system (GUTS model) [45][46][47]
Comprehensively, both pre-clinical and clinical studies’ results point to the bi-directional relationship between magnesium levels and stress: magnesium deficiency can induce symptoms and increase susceptibility to stress, and acute and chronic stress can precipitate magnesium deficiency. Summary of the preclinical and clinical evidence are shown in Tables 2 and 3, respectively.
Table 2. Summary of the pre-clinical and clinical evidence supporting the impact of stress on magnesium homeostasis.
|
|
Evidence of the impact of stress on magnesium homeostasis |
|||
|
|
Population tested |
Stress stimulus |
Impact on magnesium |
|
|
Pre-clinical |
Cats (N=30) |
Withdrawal of blood; infusion of catecholamines ; potassium poisoning |
↑Blood Mg [48] |
|
|
Guinea pigs (41) |
Noise |
↑Serum Mg, ↓Erythrocytes Mg [49] |
||
|
Rats (88) |
Noise |
↑Serum Mg, ↓Erythrocytes Mg [50] |
||
|
Rats |
Noise |
↓Serum Mg, ↓Erythrocytes Mg [51] |
||
|
Dogs |
Physical exercise, temperature |
↓Serum Mg [52] |
||
|
Rats |
Ethanol/Restraint stress |
↓Serum Mg [53] |
||
|
Rats |
Cold |
↓ Tissue content of Mg [54] |
||
|
Sheep |
Dietary Mg restriction, cold |
↓Plasma Mg [55] |
||
|
Clinical |
Adults (N=8) |
Adrenaline infusion |
↓Plasma Mg [56] |
|
|
Young adults (N=35) |
Chronic or sub-chronic psychological stress |
↓Plasma Mg [18] |
||
|
Healthy men (N=16) |
Chronic sleep deprivation |
↓Erythrocyte Mg [19] |
||
|
Young adults (N=35) |
University exams |
↑Urinary Mg [20] |
||
|
Young adults (N=30) |
University exams |
↓Erythrocyte Mg [21] |
||
|
Young adults (N=25) |
Noise |
↑Urinary Mg ↑Serum Mg [57] |
||
|
|
Healthy men (56) |
Noise |
↑Serum Mg, ↓Erythrocytes Mg; ↑Urinary Mg [58] |
|
|
|
Healthy men |
Short- and long-term physical exercise |
↑Plasma Mg [59] |
|
Mg, magnesium.
Table 3. Summary of the pre-clinical and clinical evidence supporting magnesium status on stress susceptibility. a Only symptoms shown in ≥70% of women at baseline are reported.
|
Evidence of the impact of magnesium status on stress susceptibility |
||||
|
|
Population tested |
Mg status |
Stress stimulus |
Impact on stress mediator/ stress |
|
Pre-clinical |
Rats (N=84) |
Mg-deficient |
Noise |
↑Catecholamines (NA, adrenaline, dopamine) [60] |
|
Mice (N=120) |
Mg-deficient |
Genetic selection |
↑NA [61] |
|
|
Mice (N=80) |
Mg-deficient |
Genetic selection; forced swimming test; four-plate test |
↑NA [62] |
|
|
Mice (N=100) |
Mg-deficient |
Genetic selection; immobilization test |
↑Gastric ulcers [63] |
|
|
Mice (N=20/test) |
Dietary Mg restriction |
Hyperthermia; open field test; light/dark test; hyponeophagia test |
↑CRH; ↑ACHT [64] |
|
|
Mice |
Mg-deficient |
Light dark test |
Depression-like behaviour [64][65] |
|
|
Rats |
Dietary Mg restriction |
Forced swimming test |
Depression-like behaviour [66][67] |
|
|
Rats |
Dietary Mg restriction |
Open field test |
||
|
Clinical |
Women (N=100) |
Mg-deficient |
- |
Chronic emotional stress; irritability; fatigue; sleep disturbance; headachea [68] |
|
Adults (N=264) |
Mg-deficient |
- |
Severe stress [22] |
|
|
Adults (N=100) |
Mg-deficient |
Poor sleep quality |
↑CRP [69] |
|
|
Adults (N=109) |
Mg-deficient |
- |
Depression/anxiety [70] |
|
ACHTH, adrenocorticotropic hormone; CRH, corticotrophin-releasing hormone; CRP, C-reactive protein; Mg, magnesium; NA, noradrenaline.
Noteworthy, magnesium supplementation has proven beneficial effects for the treatment of symptoms of psychological daily stress (fatigue, irritability, sleep) [68], magnesium may reduce serum cortisol levels [71], and improve stress relief in people with severe stress [72].
4.
Proposed model for the vicious circle of stress and magnesium deficiency
In summary, magnesium acts on several key physiological steps involved in the response to stressful stimuli, and also exerts long-term neuroprotective and anti-oxidant effects against stress
- Magnesium and HPA. 5-HT transmission: Magnesium directly enhances the interaction between 5-HT and its membrane receptor [36], and is also an important cofactor in the synthesis of 5-HT [36]. Glutamatergic transmission: Magnesium inhibits the glutamate directly and indirectly by blocking the glutamate N-methyl-D-aspartate (NMDA) receptor and by enhancing its reuptake in the synaptic vesicles [65]. GABA transmission: A GABA-agonistic activity of magnesium has been observed, although the mechanism has not yet been elucidated [65]. Cortisol: Magnesium indirectly reduces the release of ACTH, therefore decreasing cortisol levels [65].
- Magnesium and neuroprotection. Studies have shown positive impact of magnesium on the expression of brain-derived neurotrophic factor, a growth factor involved in neural development and activity [73][74].
- Magnesium and oxidative stress. Magnesium may be involved in suppressing the production of free radicals in various tissues including the brain [11].
In response to a stressful stimulus, stress hormones are released causing an increase of magnesium extracellular levels [36]. As a consequence, higher magnesium concentrations are excreted through the kidneys [57]. When the stressor persists over time, this mechanism may contribute to magnesium (intracellular) depletion and deficiency [56][65], and trigger the stress and magnesium vicious circle as illustrated in Figure 2.
Figure 2. The vicious circle of stress and magnesium. GABAA-R, γ-aminobutyric acid-A receptor; Mg, magnesium; NMDA-R, N-methyl-D-aspartate receptor; NA, noradrenaline; SNS, sympathetic nervous system, 5HT-R, 5-hydroxytryptamine receptor.
5. Conclusion
To conclude, while there is good evidence from animal and human studies of the bi-directional link between magnesium and stress, further research is needed to better understand the impact of this correlation and the benefit of magnesium supplementation on general health. This research is fundamental to further support adequate magnesium dietary needs, particularly in the stressed population.
The entry is from 10.3390/nu12123672
References
- Ronald C. Kessler; Sergio Aguilar-Gaxiola; Jordi Alonso; Somnath Chatterji; Sing Lee; Johan Ormel; T. Bedirhan Üstün; Philip S. Wang; The global burden of mental disorders: An update from the WHO World Mental Health (WMH) Surveys. Epidemiologia e Psichiatria Sociale 2009, 18, 23-33, 10.1017/s1121189x00001421.
- Phuong-Chi T. Pham; Son V. Pham; Jeffrey M. Miller; Hypomagnesemia in Patients with Type 2 Diabetes. Clinical Journal of the American Society of Nephrology 2007, 2, 366-373, 10.2215/cjn.02960906.
- James J DiNicolantonio; James H. O’Keefe; William Wilson; Subclinical magnesium deficiency: a principal driver of cardiovascular disease and a public health crisis. Open Heart 2018, 5, e000668, 10.1136/openhrt-2017-000668.
- Stress effects on the body . merican Psychological Association.. Retrieved 2021-1-18
- M S Seelig; Consequences of magnesium deficiency on the enhancement of stress reactions; preventive and therapeutic implications (a review).. Journal of the American College of Nutrition 1994, 13, 429-446, 10.1080/07315724.1994.10718432.
- L Galland; Magnesium, stress and neuropsychiatric disorders.. Magnesium and trace elements 1991, 10, 287-301.
- Rebecca Costello; Taylor C Wallace; Rebecca B Costello; Magnesium. Advances in Nutrition: An International Review Journal 2016, 7, 199-201, 10.3945/an.115.008524.
- Snigdha T. Reddy; Sandeep Soman; Jerry Yee; Magnesium Balance and Measurement. Advances in Chronic Kidney Disease 2018, 25, 224-229, 10.1053/j.ackd.2018.03.002.
- Nutrition And Allergies (Nda) Efsa Panel On Dietetic Products; Scientific Opinion on Dietary Reference Values for magnesium. EFSA Journal 2015, 13, 25, 10.2903/j.efsa.2015.4186.
- Sidsel-Marie Glasdam; Stinne Glasdam; Günther H.J. Peters; The Importance of Magnesium in the Human Body. Advances in Virus Research 2016, 73, 169-193, 10.1016/bs.acc.2015.10.002.
- Ryu Yamanaka; Yutaka Shindo; K. Oka; Magnesium Is a Key Player in Neuronal Maturation and Neuropathology. International Journal of Molecular Sciences 2019, 20, 3439, 10.3390/ijms20143439.
- Mounir Ghabriel; Robert Vink; Magnesium transport across the blood-brain barriers. Magnesium in the Central Nervous System 2011, NA, 59-74, 10.1017/upo9780987073051.004.
- Willi Jahnen-Dechent; Markus Ketteler; Magnesium basics. Clinical Kidney Journal 2012, 5, i3-i14, 10.1093/ndtplus/sfr163.
- L Spätling; H G Classen; W R Külpmann; F Manz; P M Rob; H F Schimatschek; W Vierling; J Vormann; A Weigert; K Wink; et al. [Diagnosing magnesium deficiency. Current recommendations of the Society for Magnesium Research].. Fortschritte der Medizin. Originalien 2000, NA, 49-53.
- Jeroen H. F. De Baaij; Joost G. J. Hoenderop; René J. M. Bindels; Magnesium in Man: Implications for Health and Disease. Physiological Reviews 2015, 95, 1-46, 10.1152/physrev.00012.2014.
- Ross, C.A.; Caballero, B.; Cousins, R.J.; Tucker, K.L.; Ziegler, T.R.. Modern Nutrition in Health and Disease; Lippincott Williams & Wilkins: Baltimore, 2014; pp. 159-175..
- Ronald J Elin; Assessment of magnesium status for diagnosis and therapy.. Magnesium Research 2010, 23, 194-198, 10.1684/mrh.2010.0213.
- Ibolja Cernak; V Savic; J Kotur; V Prokic; B Kuljic; D Grbovic; M Veljovic; Alterations in magnesium and oxidative status during chronic emotional stress.. Magnesium research 2000, 13, 29-36.
- Kazuhiko Tanabe; Naohiko Osada; Noriyuki Suzuki; Masaru Nakayama; Yasuhiro Yokoyama; Akiko Yamamoto; Misa Oya; Taizo Murabayashi; Masanobu Yamamoto; Kazuto Omiya; et al.Haruki ItohMasahiro Murayama Erythrocyte magnesium and prostaglandin dynamics in chronic sleep deprivation. Clinical Cardiology 1997, 20, 265-268, 10.1002/clc.4960200315.
- G Grases; J A Pérez-Castelló; P Sanchis; A Casero; J Perelló; B Isern; E Rigo; F Grases; Anxiety and stress among science students. Study of calcium and magnesium alterations.. Magnesium research 2006, 19, 102-106.
- Bonpei Takase; Takashi Akima; Akimi Uehata; Fumitaka Ohsuzu; Akira Kurita; Effect of chronic stress and sleep deprivation on both flow-mediated dilation in the brachial artery and the intracellular magnesium level in humans. Clinical Cardiology 2004, 27, 223-227, 10.1002/clc.4960270411.
- Noah, L.; Pickering, G.; Mazur, A.; Dubray, C.; Hitier, S.; Dualé, C.; Pouteau, E.; Impact of magnesium supplementation, in combination with vitamin B6, on stress and magnesium status: secondary data from a randomised controlled trial. Magnesium Research Journal. 2020, accepted. in publication , NA.
- Forrest Nielsen; The Problematic Use of Dietary Reference Intakes to Assess Magnesium Status and Clinical Importance. Biological Trace Element Research 2018, 188, 52-59, 10.1007/s12011-018-1573-x.
- Christine Bergman; Darlene Gray-Scott; Jau-Jiin Chen; Susan Meacham; What is Next for the Dietary Reference Intakes for Bone Metabolism Related Nutrients Beyond Calcium: Phosphorus, Magnesium, Vitamin D, and Fluoride?. Critical Reviews in Food Science and Nutrition 2009, 49, 136-144, 10.1080/10408390701764468.
- Jürgen Vormann; Magnesium: nutrition and metabolism. Molecular Aspects of Medicine 2003, 24, 27-37, 10.1016/s0098-2997(02)00089-4.
- Dana E. King; Arch G. Mainous; Mark E. Geesey; Robert F. Woolson; Dietary Magnesium and C-reactive Protein Levels. Journal of the American College of Nutrition 2005, 24, 166-171, 10.1080/07315724.2005.10719461.
- G. B. M. Mensink; R. Fletcher; M. Gurinovic; I. Huybrechts; L. Lafay; L. Serra-Majem; L. Szponar; I. Tetens; J. Verkaik-Kloosterman; A. Baka; et al.A. M. Stephen Mapping low intake of micronutrients across Europe. British Journal of Nutrition 2013, 110, 755-773, 10.1017/s000711451200565x.
- Agence nationale de sécurité sanitaire de l’alimentation de l’environnement et du travail (ANSES). AVIS de l'ANSES du 13 mars 2015 relatif à l’évaluation des apports en vitamines et minéraux issus de l'alimentation non enrichie, de l’alimentation enrichie et des compléments alimentaires dans la population française : estimation des apports usuels, des prévalences d'inadéquation et des risques de dépassement des limites de sécurité (Saisine n°2012-SA-0142). ANSES, Ed. 2015.
- Società Italiana di Nutrizione Umana-SINU. LARN – Livelli di assunzione di riferimento per la popolazione italiana: MINERALI. Assunzione raccomandata per la popolazione (PRI in grassetto) e assunzione adeguata (AI in corsivo): valori su base giornaliera. Availabe online: https://sinu.it/2019/07/09/minerali-assunzione-raccomandata-per-la-popolazione-pri-e-assunzione-adeguataai/
- Tutel'ian, V.A. Norms of physiological requirements in energy and nutrients in various groups of population in Russian Federation. Vopr Pitan 2009, 78, 4-15.
- Ministry of Health Labour and Welfare. Dietary Reference Intakes for Japanese (2015). Office, J.G.P., Ed. 2015.
- Jarosz M. Nutritional guidelines for the Polish population. National Food and Nutrition Institute, Ed. National Food and Nutrition Institute,: Warsaw, 2017.
- Standing Commitee on the Scientific Evaluation of Dietary Reference Intakes Institute of Medicine. Dietary reference intakes for calcium, phosphorus, magnesium, vitamin D, and fluoride. In Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride, Washington, D.N.A.P., Ed. The National Academies Press: 1997; pp. 190-249
- Avis de l’ANSES. Actualisation des repères du PNNS: élaborationdes références nutritionnelles. (ANSES), Ed. 2016.
- Bruce S. McEwen; Huda Akil; Revisiting the Stress Concept: Implications for Affective Disorders. The Journal of Neuroscience 2020, 40, 12-21, 10.1523/jneurosci.0733-19.2019.
- Vink, R., Nechifor, M.,. Magnesium in the central nervous system: Chapter 19; University of Adelaide Press: Adelaide , 2011; pp. na.
- George Chrousos; Stress and disorders of the stress system. Nature Reviews Endocrinology 2009, 5, 374-381, 10.1038/nrendo.2009.106.
- Bruce S. McEwen; Protective and Damaging Effects of Stress Mediators. New England Journal of Medicine 1998, 338, 171-179, 10.1056/nejm199801153380307.
- Laurence Lanfumey; Raymond Mongeau; Charles Cohen-Salmon; Michel Hamon; Corticosteroid–serotonin interactions in the neurobiological mechanisms of stress-related disorders. Neuroscience & Biobehavioral Reviews 2008, 32, 1174-1184, 10.1016/j.neubiorev.2008.04.006.
- James P. Herman; Nancy K. Mueller; Helmer Figueiredo; Role of GABA and Glutamate Circuitry in Hypothalamo-Pituitary-Adrenocortical Stress Integration. Annals of the New York Academy of Sciences 2004, 1018, 35-45, 10.1196/annals.1296.004.
- Jos F. Brosschot; Bart Verkuil; Julian F. Thayer; The default response to uncertainty and the importance of perceived safety in anxiety and stress: An evolution-theoretical perspective. Journal of Anxiety Disorders 2016, 41, 22-34, 10.1016/j.janxdis.2016.04.012.
- Bartłomiej Pochwat; Bernadeta Szewczyk; Magdalena Sowa-Kućma; Agata Siwek; Urszula Doboszewska; Wojciech Piekoszewski; Piotr Gruca; Mariusz Papp; Gabriel Nowak; Antidepressant-like activity of magnesium in the chronic mild stress model in rats: alterations in the NMDA receptor subunits. The International Journal of Neuropsychopharmacology 2013, 17, 393-405, 10.1017/s1461145713001089.
- Robert Vink; Magnesium in the CNS: recent advances and developments.. Magnesium Research 2016, 29, 95-101, 10.1684/mrh.2016.0408.
- Anastasia A. Zheltova; Maria V. Kharitonova; Igor Iezhitsa; Alexander A. Spasov; Magnesium deficiency and oxidative stress: an update. BioMedicine 2016, 6, 20, 10.7603/s40681-016-0020-6.
- G. G. Somjen; E. N. Baskerville; Effect of Excess Magnesium on Vagal Inhibition and Acetylcholine Sensitivity of the Mammalian Heart in situ and in vitro. Nature 1968, 217, 679-680, 10.1038/217679a0.
- N Toda; T C West; Interaction between Na, Ca, Mg, and vagal stimulation in the S-A node of the rabbit. American Journal of Physiology-Legacy Content 1967, 212, 424-430, 10.1152/ajplegacy.1967.212.2.424.
- Yoshinobu Murasato; Yuji Harada; Masaharu Ikeda; Yasuhide Nakashima; Yoshiaki Hayashida; Effect of Magnesium Deficiency on Autonomic Circulatory Regulation in Conscious Rats. Hypertension 1999, 34, 247-252, 10.1161/01.hyp.34.2.247.
- H.-G. Classen; P. Marquardt; M. Späth; K.-A. Schumacher; Hypermagnesemia Following Exposure to Acute Stress. Pharmacology 1971, 5, 287-294, 10.1159/000136201.
- H. Ising; M. Handrock; R. Fischer; M. Dombrowski; Increased noise trauma in guinea pigs through magnesium deficiency. European Archives of Oto-Rhino-Laryngology 1982, 236, 139-146, 10.1007/bf00454034.
- Z. Joachims; W Babisch; H Ising; T Günther; M Handrock; Dependence of noise‐induced hearing loss upon perilymph magnesium concentration. The Journal of the Acoustical Society of America 1983, 74, 104-108, 10.1121/1.389726.
- Ising, H.; Interaction of noise-induced stress and Mg decrease. Artery 1981, 9, 205-211.
- Izumi Ando; Kaoru Karasawa; Shinichi Yokota; Takao Shioya; Hiroshi Matsuda; Akane Tanaka; Analysis of serum magnesium ions in dogs exposed to external stress: A pilot study. Open Veterinary Journal 2017, 7, 367-374, 10.4314/ovj.v7i4.13.
- Farzana Yasmin; Darakhshan J Haleem; M A Haleem; Effects of repeated restraint stress on serum electrolytes in ethanol-treated and water-treated rats.. pakistan journal of pharmaceutical sciences 2007, 20, 51-55.
- O. Héroux; D. Peter; A. Heggtveit; Long-term Effect of Suboptimal Dietary Magnesium on Magnesium and Calcium Contents of Organs, on Cold Tolerance and on Lifespan, and its Pathological Consequences in Rats. The Journal of Nutrition 1977, 107, 1640-1652, 10.1093/jn/107.9.1640.
- Yoshiaki Terashima; Ray E. Tucker; Lawrence E. Deetz; Robert M. DeGregorio; Russell B. Muntifering; George E. Mitchell; Plasma Magnesium Levels as Influenced by Cold Exposure in Fed or Fasted Sheep. The Journal of Nutrition 1982, 112, 1914-1920, 10.1093/jn/112.10.1914.
- Kenneth F. Whyte; George J. Addis; Robert Whitesmith; John L. Reid; Adrenergic control of plasma magnesium in man. Clinical Science 1987, 72, 135-138, 10.1042/cs0720135.
- F Mocci; P. Canalis; P A Tomasi; F. Casu; S. Pettinato; The effect of noise on serum and urinary magnesium and catecholamines in humans.. Occupational Medicine 2001, 51, 56-61, 10.1093/occmed/51.1.56.
- H. Ising; D. Dienel; T Günther; B. Markert; Health effects of traffic noise. International Archives of Occupational and Environmental Health 1980, 47, 179-190, 10.1007/bf00716376.
- H. Joborn; G. Åkerström; S. Ljunghall; EFFECTS OF EXOGENOUS CATECHOLAMINES AND EXERCISE ON PLASMA MAGNESIUM CONCENTRATIONS. Clinical Endocrinology 1985, 23, 219-226, 10.1111/j.1365-2265.1985.tb00217.x.
- Joan Caddell; Rose Kupiecki; Deborah L. Proxmire; Paul Satoh; Bruce Hutchinson; Plasma Catecholamines in Acute Magnesium Deficiency in Weanling Rats. The Journal of Nutrition 1986, 116, 1896-1901, 10.1093/jn/116.10.1896.
- Amyard, N.; Leyris, A.; Monier, C.; Francès, H.; Boulu, R.G.; Henrotte, J.G. Brain catecholamines, serotonin and their metabolites in mice selected for low (MGL) and high (MGH) blood magnesium levels. Magnesium research 1995, 8, 5-9.
- Jean G Henrotte; Gisèle Franck; Monique Santarromana; Henriette Francès; Denise Mouton; Roland Motta; Mice Selected for Low and High Blood Magnesium Levels: A New Model for Stress Studies. Physiology & Behavior 1997, 61, 653-658, 10.1016/s0031-9384(96)00506-9.
- Jean G Henrotte; Nicole Aymard; Monique Allix; Roger Boulu; Effect of Pyridoxine and Magnesium on Stress-Induced Gastric Ulcers in Mice Selected for Low or High Blood Magnesium Levels. Annals of Nutrition and Metabolism 1995, 39, 285-290, 10.1159/000177874.
- S.B. Sartori; N. Whittle; A. Hetzenauer; N. Singewald; Magnesium deficiency induces anxiety and HPA axis dysregulation: Modulation by therapeutic drug treatment. Neuropharmacology 2012, 62, 304-312, 10.1016/j.neuropharm.2011.07.027.
- H. Murck; Magnesium and Affective Disorders. Nutritional Neuroscience 2002, 5, 375-389, 10.1080/1028415021000039194.
- Spasov, A.A.; Iezhitsa, I.N.; Kharitonova, M.V.; Kravchenko, M.S. Depression-like and anxiety-related behaviour of rats fed with magnesium-deficient diet. Zh Vyssh Nerv Deiat Im I P Pavlova 2008, 58, 476-485.
- Iezhitsa, I.N.; Spasov, A.A.; Kharitonova, M.V.; Kravchenko, M.S. Effect of magnesium chloride on psychomotor activity, emotional status, and acute behavioural responses to clonidine, d-amphetamine, arecoline, nicotine, apomorphine, and L-5-hydroxytryptophan. Nutr Neurosci 2011, 14, 10-24, doi:10.1179/174313211x12966635733277.
- Akarachkova, E. The role of magnesium deficiency in the formation of clinical manifestation of stress in women Problems of women health 2013, 8.
- Forrest H Nielsen; LuAnn Johnson; Huawei Zeng; Magnesium supplementation improves indicators of low magnesium status and inflammatory stress in adults older than 51 years with poor quality sleep.. Magnesium Research 2011, 23, 172-176, 10.1684/mrh.2010.0220.
- Adrienne K. Forsyth; Peter G. Williams; Frank P. Deane; Nutrition status of primary care patients with depression and anxiety. Australian Journal of Primary Health 2012, 18, 172-176, 10.1071/py11023.
- Dušanka Zogović; Vesna Pešić; Gordana Dmitrašinović; Marijana Dajak; Bosiljka Plećaš; Bojan Batinić; Dejana Popovic; Svetlana Ignjatovic; Pituitary-Gonadal, Pituitary-Adrenocortical Hormones and IL-6 Levels Following Long-Term Magnesium Supplementation in Male Students. Journal of Medical Biochemistry 2014, 33, 291-298, 10.2478/jomb-2014-0016.
- Etienne Pouteau; Marmar Kabir-Ahmadi; Lionel Noah; Andre Mazur; Louise Dye; Juliane Hellhammer; Gisele Pickering; Claude DuBray; Superiority of magnesium and vitamin B6 over magnesium alone on severe stress in healthy adults with low magnesemia: A randomized, single-blind clinical trial. PLoS ONE 2018, 13, e0208454, 10.1371/journal.pone.0208454.
- Nashat Abumaria; Bin Yin; Ling Zhang; Xiang-Yao Li; Tao Chen; Giannina Descalzi; Liangfang Zhao; Matae Ahn; Lin Luo; Chen Ran; et al.Min ZhuoGuosong Liu Effects of Elevation of Brain Magnesium on Fear Conditioning, Fear Extinction, and Synaptic Plasticity in the Infralimbic Prefrontal Cortex and Lateral Amygdala. The Journal of Neuroscience 2011, 31, 14871-14881, 10.1523/jneurosci.3782-11.2011.
- Bartlomiej Pochwat; Magdalena Sowa-Kućma; Katarzyna Kotarska; Paulina Misztakk; Gabriel Nowak; Bernadeta Szewczyk; Antidepressant-like activity of magnesium in the olfactory bulbectomy model is associated with the AMPA/BDNF pathway. Psychopharmacology 2014, 232, 355-367, 10.1007/s00213-014-3671-6.
- Adrienne K. Forsyth; Peter G. Williams; Frank P. Deane; Nutrition status of primary care patients with depression and anxiety. Australian Journal of Primary Health 2012, 18, 172-176, 10.1071/py11023.