Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 2 by Fanny Huang and Version 1 by Claudio Manna.
Varicocele treatment is beneficial in improving semen parameters and pregnancy rate when an appropriate selection of patients is made. The purpose of treating varicocele in adults is mainly to improve current fertility status. On the other hand, the goal of treatment in adolescents is to prevent testicular injury and maintain testicular function for future fertility. Hence, the key to the success of varicocele treatment seems to be a correct indication.
- varicocele repair
- varicocelectomy
- infertility
- varicocele
1. Introduction
A varicocele is defined as an abnormal dilatation and/or tortuosity of the pampiniform venous plexus in the scrotum. It is a pathological condition caused by an alteration in the drainage of the testicle due to venous reflux in the internal spermatic vein (ISV). In fact, the left side is mainly affected due to anatomical reasons related to the ISV. In a previous study, using femoral and spermatic venographies, researchers observed the exclusive involvement of ISV in primary and recurrent varicoceles [1].
The condition occurs in 15% of the healthy general male population, in 35% of men with primary infertility, and in up to 80% of men with secondary infertility [2]. Several different clinical [3] and US sonographic classifications have been proposed for varicocele assessment, but unfortunately, there is no standardization, and a clear consensus has not yet been reached, which obviously also leads to difficulties in comparability [4]. According to the fourth edition of WHO classification [5], there are three grades of varicocele depending on the severity of it, from 1 to 3, with no reference to an absolute measure of the vein diameter or sonographic evidence of reflux with velocity measurement. On the other hand, Sarteschi describes a five-part classification, depending on the presence of dilated veins while supine and/or standing, the anatomical relationships of the dilated veins with the testis, the characteristics of reflux, and testicular size [6]. Cavallini et al. focused on varicocele grade and degree of reflux, showing that surgery to improve OAT and, thus, chances of successful ART should be reserved for Dubin and Amelar grade 2 and grade 3 varicoceles with continuous venous reflux at duplex Doppler assessment [7]. Furthermore, no global consensus has been established on the need for sonographic examination in the diagnosis of varicocele: on the first hand AUA/ASRM guidelines sustain that scrotal ultrasound should not be routinely performed in the initial evaluation of the infertile male; on the other hand, the EAU Guidelines, in accordance with the European Society of Urogenital Radiology Scrotal and Penile Imaging Working Group, consider scrotal Doppler necessary if physical examination is inconclusive or semen analysis remains unsatisfactory after varicocele repair to identify persistent and recurrent varicocele [8,9,10][8][9][10].
Varicocele may cause spermatogenetic damage resulting in altered seminal parameters, abnormalities in the development and growth of the affected testis, and, rarely, symptoms such as discomfort and pain [11]. Thus observational studies suggest that men with a varicocele tend to have a higher proportion of spermatozoa with fragmented DNA, lower total sperm counts, lower progressive sperm motility, lower sperm vitality, and higher abnormal forms when compared to control groups [12]. The exact pathophysiology and, especially, the cause–effect relationship between the presence of varicocele and abnormalities of the semen analysis has not been clearly established [13]. Conversely, a recent systematic review and meta-analysis provide a high level of evidence in favor of a positive effect of VR to improve conventional semen parameters in infertile men with clinical varicocele [14].
2. Surgical Treatment
Several therapeutic options are available for varicocele treatment and may involve an endovascular or surgical approach [13].
In Europe, endovascular techniques are popular due to their minimally invasive nature, despite their higher recurrence rates [15]. They include:
-
Retrograde sclero-embolization, trans-femoral or trans-brachial;
-
Retroperitoneal;
- .
Concerning surgical approach, this may be:
- Inguinal;
-
Sub-inguinal.
The retroperitoneal access involves an incision in the supra inguinal site and the ligation of the ISV immediately above the internal inguinal ring (Ivanissevich technique) or higher up at the level of the anterior iliac spine (Palomo technique).
A recent Palomo technique variant consists of sparing a few lymphatic vessels with the aid of an operating microscope, to avoid post-operative hydrocele which might occur after the standard Palomo procedure [17,18,19,20][17][18][19][20]. The approach is moved from the sub-inguinal to the pre-peritoneal level, just above the internal inguinal ring, as described by Jones for nonpalpable testes [21]. The internal spermatic veins are reached by splitting the muscle plane and thus preserving the integrity of the inguinal channel. The deferential vein can be evaluated but not necessarily ligated, considering that dilation is not synonymous with reflux [17] (Figure 1).
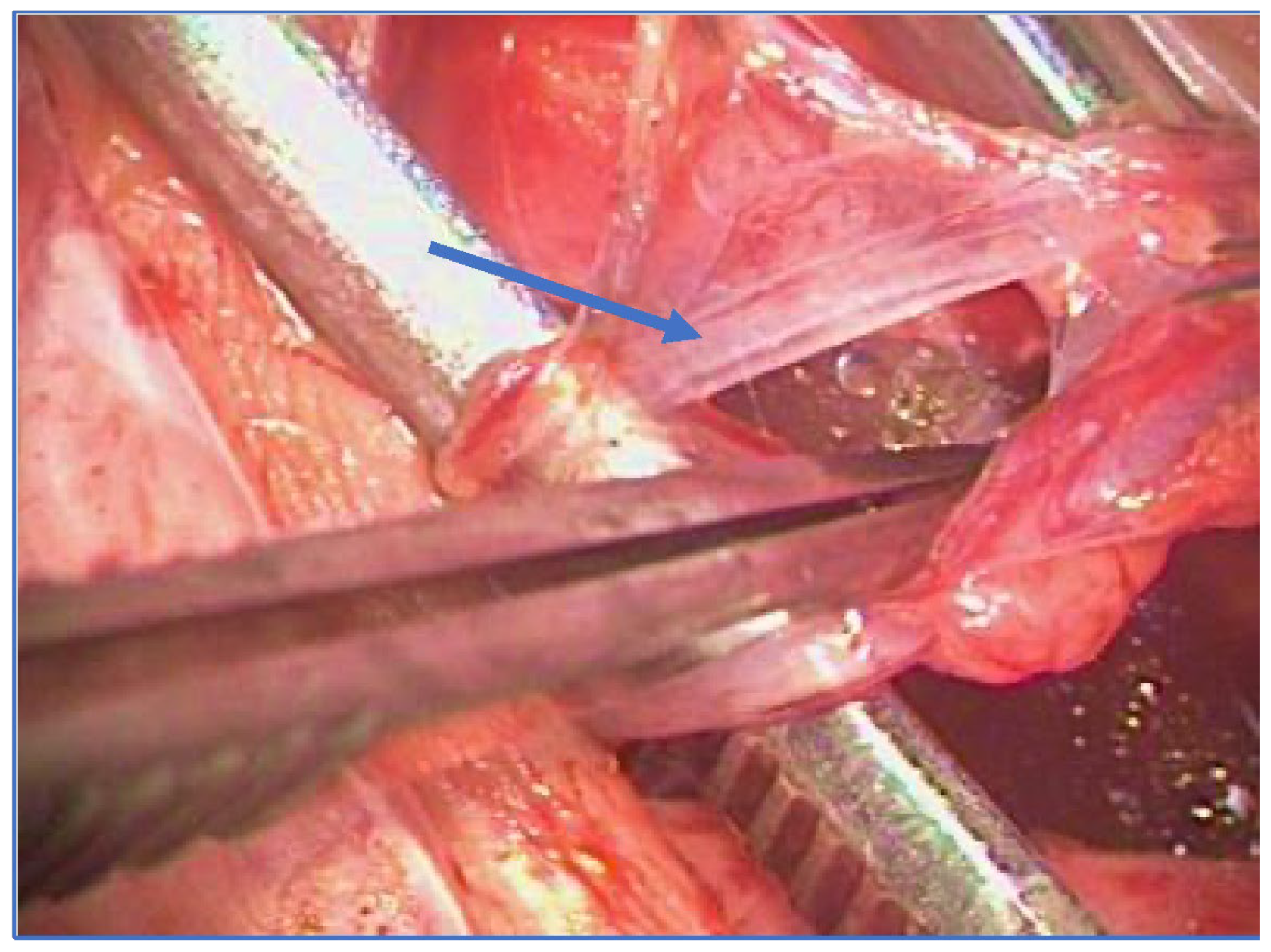
Figure 1. Microsurgical lymphatic sparing Palomo technique (arrow: spared lymphatics).
Retroperitoneal repair can also be performed using the laparoscopic technique, particularly in bilateral disease [22]. In researchers' view, laparoscopic repair appears to be more invasive and costly than the other techniques, due to general anesthesia, pneumoperitoneum issues and extremely rare but possible dreadful complications [23]; however, it has the advantage of excellent visibility of the posterior abdominal wall allowing a thorough search of sites known to be responsible for recurrent varicoceles, such as renal, caval and pelvic cross-over veins. Moreover, optical magnification optimizes the surgeon’s ability to preserve the testicular artery and lymphatic channels while ligating all veins to minimize the risk of hydrocele formation or varicocele recurrence. Finally, the laparoscopic approach allows a simultaneous correction of bilateral varicocele. Some evidence demonstrates lower recurrence rates (3–6%), especially when compared to sclero-embolization procedures, which were shown to reach 4–11% of varicocele recurrence [24]; furthermore, sclero-embolization procedures have their specific complications, such as inadvertent femoral artery perforation, radiation exposure, sclerosant agent local irritation or orchitis and coil migration that, despite being very uncommon, should be taken into account [25,26][25][26].
The sub-inguinal microsurgical technique, instead, is widely used in the United States with very low reported recurrence rates [27,28][27][28].
Different subinguinal microsurgical modified approaches have been subsequently proposed [27,29][27][29]. According to EAU guidelines and AUA/ASRM [30], the use of an operating microscope makes microsurgical subinguinal varicocelectomy the preferred method of treatment due to its lower incidence of complications and recurrence rates, as well as its potential for greater improvement in semen parameters [30,31][30][31]. However, it is technically demanding and needs access to an operating microscope [32].
Regarding the outcomes of the different techniques, there is still debate in the literature: a meta-analysis by Cayan et al. suggested that surgical intervention was better than embolization with regard to spontaneous pregnancy rates (41.97% for microsurgery versus 33.20% for embolization, p = 0.001) [23] and recurrence rates (1.05% for microsurgery versus 12.70% for embolization, p = 0.001) [23]. A randomized controlled trial (RCT) from Al-Kandari et al. demonstrated that, compared with open inguinal and laparoscopic varicocelectomy, subinguinal microsurgical varicocelectomy offers the best outcome only in terms of complications (hydrocele) and recurrence [33]. In researchers' experience, the modified lymphatic-sparing Palomo technique appears to offer excellent results in terms of outcomes and complication rates: one of the authors (F.F.), in the period January 2009–September 2020, treated 633 children and adolescents using this technique with a recurrence rate of 2.8% and postoperative hydrocele rate of 0.4% (unpublished data). Therefore, no technique has been proven to be certainly superior to the others. Each one of them has its own advantages and disadvantages (Table 1).
Table 1. Varicocele surgical techniques: pros and cons.
| Technique | Pros | Cons |
|---|---|---|
| Open retroperitoneal high ligation (Palomo) [23,33,48,83][23][33][34][35] | Complete ligation | General anesthesia, Higher hydrocele risk |
| Microsurgical lymphatic sparing Palomo [13,17,[18,17]19,20][13][18][19][20] |
Complete ligation Lower hydrocele risk |
General anesthesia Access to operating microscope |
| Microsurgical subinguinal or inguinal surgery [23,28,33][23][28][33] | Less invasive (local anesthesia) Lower recurrence rate Lower hydrocele risk |
Access to operating microscope Longer surgical time |
| Laparoscopic surgery [23,32,33][23][32][33] |
Bilateral varicocele Higher magnification Lower recurrence rate |
High costs More invasive (intraperitoneal) General anesthesia |
| Sclero-embolization [15,,48][16,15][23,1624,25,][23][24][25]26[26][34] |
Minimally invasive Short time Outpatient |
Limited applicability Higher recurrence rate Radiation exposure |
References
- Franco, G.; Iori, F.; De Dominicis, C.; Dal Forno, S.; Mander, A.; Laurenti, C. Challenging the Role of Cremasteric Reflux in the Pathogenesis of Varicocele Using a New Venographic Approach. J. Urol. 1999, 161, 117–121.
- Alsaikhan, B.; Alrabeeah, K.; Delouya, G.; Zini, A. Epidemiology of Varicocele. Asian J. Androl. 2016, 18, 179.
- Dubin, L.; Amelar, R.D. Varicocele Size and Results of Varicocelectomy in Selected Subfertile Men with Varicocele. Fertil. Steril. 1970, 21, 606–609.
- Freeman, S.; Bertolotto, M.; Richenberg, J.; Belfield, J.; Dogra, V.; Huang, D.Y.; Lotti, F.; Markiet, K.; Nikolic, O.; Ramanathan, S.; et al. Ultrasound Evaluation of Varicoceles: Guidelines and Recommendations of the European Society of Urogenital Radiology Scrotal and Penile Imaging Working Group (ESUR-SPIWG) for Detection, Classification, and Grading. Eur. Radiol. 2020, 30, 11–25.
- WHO Manual for the Standardized Investigation and Diagnosis of the Infertile Male. Available online: https://www.who.int/publications/i/item/9780521774741 (accessed on 15 May 2023).
- Sarteschi, L.; Paoli, R.; Bianchini, M.; Menchini Fabris, G. Lo Studio Del Varicocele Con Eco-Color-Doppler. G Ital. Ultrasonol. 1993, 4, 43–49.
- Cavallini, G.; Scroppo, F.I.; Colpi, G.M. The Clinical Usefulness of a Novel Grading System for Varicocoeles Using Duplex Doppler Ultrasound Examination Based on Postsurgical Modifications of Seminal Parameters. Andrology 2019, 7, 62–68.
- Schlegel, P.N.; Sigman, M.; Collura, B.; De Jonge, C.J.; Eisenberg, M.L.; Lamb, D.J.; Mulhall, J.P.; Niederberger, C.; Sandlow, J.I.; Sokol, R.Z.; et al. Diagnosis and Treatment of Infertility in Men: AUA/ASRM Guideline Part I. Fertil. Steril. 2021, 115, 54–61.
- Minhas, S.; Bettocchi, C.; Boeri, L.; Capogrosso, P.; Carvalho, J.; Cilesiz, N.C.; Cocci, A.; Corona, G.; Dimitropoulos, K.; Gül, M.; et al. European Association of Urology Guidelines on Male Sexual and Reproductive Health: 2021 Update on Male Infertility. Eur. Urol. 2021, 80, 603–620.
- Su, J.S.; Farber, N.J.; Vij, S.C. Pathophysiology and Treatment Options of Varicocele: An Overview. Andrologia 2021, 53, e13576.
- Dieamant, F.; Petersen, C.G.; Mauri, A.L.; Conmar, V.; Mattila, M.; Vagnini, L.D.; Renzi, A.; Costa, B.P.; Zamara, C.; Oliveira, J.B.A.; et al. Semen Parameters in Men with Varicocele: DNA Fragmentation, Chromatin Packaging, Mitochondrial Membrane Potential, and Apoptosis. JBRA Assist. Reprod. 2017, 21, 295–301.
- Franco, G.; Misuraca, L.; Ciletti, M.; Leonardo, C.; De Nunzio, C.; Palminteri, E.; De Dominicis, C. Surgery of Male Infertility: An Update. Urologia 2014, 81, 154–164.
- Agarwal, A.; Cannarella, R.; Saleh, R.; Boitrelle, F.; Gül, M.; Toprak, T.; Salvio, G.; Arafa, M.; Russo, G.I.; Harraz, A.M.; et al. Impact of Varicocele Repair on Semen Parameters in Infertile Men: A Systematic Review and Meta-Analysis. World J. Men’s Health 2023, 41, 220142.
- Crestani, A.; Giannarini, G.; Calandriello, M.; Rossanese, M.; Mancini, M.; Novara, G.; Ficarra, V. Antegrade Scrotal Sclerotherapy of Internal Spermatic Veins for Varicocele Treatment: Technique, Complications, and Results. Asian J. Androl. 2016, 18, 292–295.
- Matsuda, T.; Horii, Y.; Yoshida, O. Should the Testicular Artery Be Preserved at Varicocelectomy? J. Urol. 1993, 149, 1357–1360.
- Ferro, F.; Gentile, V. Il Varicocele in Età Pediatrica Ed Adolescenziale. In Varicocele e Infertilità Maschile; Flati, G., Gentile, V., Lenzi, A., Eds.; SEU: Rome, Italy, 2006.
- Riccabona, M.; Oswald, J.; Koen, M.; Lusuardi, L.; Radmayr, C.; Bartsch, G. Optimizing the Operative Treatment of Boys with Varicocele: Sequential Comparison of 4 Techniques. J. Urol. 2003, 169, 666–668.
- Silveri, M.; Bassani, F.; Adorisio, O. Changing Concepts in Microsurgical Pediatric Varicocelectomy: Is Retroperitoneal Approach Better than Subinguinal One? Urol. J. 2015, 12, 2032–2035.
- Zhang, H.; Li, H.; Hou, Y.; Jin, J.; Gu, X.; Zhang, M.; Huo, W.; Li, H. Microscopic Retroperitoneal Varicocelectomy with Artery and Lymphatic Sparing: An Alternative Treatment for Varicocele in Infertile Men. Urology 2015, 86, 511–515.
- Jones, P.F.; Bagley, F.H. An Abdominal Extraperitoneal Approach for the Difficult Orchidopexy. Br. J. Surg. 1979, 66, 14–18.
- Kroese, A.C.; de Lange, N.M.; Collins, J.; Evers, J.L. Surgery or Embolization for Varicoceles in Subfertile Men. Cochrane Database Syst. Rev. 2012, 10, 67.
- Çayan, S.; Shavakhabov, S.; Kadioǧlu, A. Treatment of Palpable Varicocele in Infertile Men: A Meta-Analysis to Define the Best Technique. J. Androl. 2009, 30, 33–40.
- Makris, G.C.; Efthymiou, E.; Little, M.; Boardman, P.; Anthony, S.; Uberoi, R.; Tapping, C. Safety and Effectiveness of the Different Types of Embolic Materials for the Treatment of Testicular Varicoceles: A Systematic Review. Br. J. Radiol. 2018, 91, 20170445.
- Halpern, J.; Mittal, S.; Pereira, K.; Bhatia, S.; Ramasamy, R. Percutaneous Embolization of Varicocele: Technique, Indications, Relative Contraindications, and Complications. Asian J. Androl. 2016, 18, 234–238.
- Bebi, C.; Bilato, M.; Minoli, D.G.; De Marco, E.A.; Gnech, M.; Paraboschi, I.; Boeri, L.; Fulgheri, I.; Brambilla, R.; Campoleoni, M.; et al. Radiation Exposure and Surgical Outcomes after Antegrade Sclerotherapy for the Treatment of Varicocele in the Paediatric Population: A Single Centre Experience. J. Clin. Med. 2023, 12, 755.
- Goldstein, M.; Gilbert, B.R.; Dicker, A.P.; Dwosh, J.; Gnecco, C. Microsurgical Inguinal Varicocelectomy with Delivery of the Testis: An Artery and Lymphatic Sparing Technique. J. Urol. 1992, 148, 1808–1811.
- Marmar, J.L.; DeBenedictis, T.J.; Praiss, D. The Management of Varicoceles by Microdissection of the Spermatic Cord at the External Inguinal Ring. Fertil. Steril. 1985, 43, 583–588.
- Colpi, G.M.; Carmignani, L.; Nerva, F.; Piediferro, G.; Castiglioni, F.; Grugnetti, C.; Galasso, G. Surgical Treatment of Varicocele by a Subinguinal Approach Combined with Antegrade Intraoperative Sclerotherapy of Venous Vessels. BJU Int. 2006, 97, 142–145.
- Practice Committee of the American Society for Reproductive Medicine. Report on Varicocele and Infertility. Fertil. Steril. 2008, 90, S247–S249.
- Mehta, A.; Goldstein, M. Microsurgical Varicocelectomy: A Review. Asian J. Androl. 2013, 15, 56–60.
- Wang, H.; Ji, Z.G. Microsurgery Versus Laparoscopic Surgery for Varicocele: A Meta-Analysis and Systematic Review of Randomized Controlled Trials. J. Investig. Surg. 2020, 33, 40–48.
- Al-Kandari, A.M.; Shabaan, H.; Ibrahim, H.M.; Elshebiny, Y.H.; Shokeir, A.A. Comparison of Outcomes of Different Varicocelectomy Techniques: Open Inguinal, Laparoscopic, and Subinguinal Microscopic Varicocelectomy: A Randomized Clinical Trial. Urology 2007, 69, 417–420.
- Evers, J.L.H.; Collins, J.; Clarke, J. Surgery or Embolisation for Varicoceles in Subfertile Men. Cochrane Database Syst. Rev. 2009, 10, CD000479, Update in: Cochrane Database Syst. Rev. 2012, 10, CD000479.
- Lara-Cerrillo, S.; Gual-Frau, J.; Benet, J.; Abad, C.; Prats, J.; Amengual, M.J.; Ribas-Maynou, J.; García-Peiró, A. Microsurgical Varicocelectomy Effect on Sperm Telomere Length, DNA Fragmentation and Seminal Parameters. Hum. Fertil. 2022, 25, 135–141.
- Palomo, A. Radical Cure of Varicocele by a New Technique; Preliminary Report. J. Urol. 1949, 61, 604–607.
More
