Cerebrotendinous xanthomatosis (CTX) is an autosomal recessive disorder caused by pathogenic variants in CYP27A1, leading to a deficiency in sterol 27-hydroxylase. This defect results in the accumulation of cholestanol and bile alcohols in various tissues, including the brain, tendons, and peripheral nerves. Elevated levels of cholestanol are consistently observed. Most patients present normal or low serum cholesterol levels. The decrease in chenodeoxycholic acid (CDCA) leads to increased synthesis of cholesterol metabolites such as bile alcohols 23S-pentol and 25-tetrol 3-glucuronide, which may serve as surrogate follow-up markers in patients with CTX. Lipid abnormalities in CTX have clinical implications. Cholestanol deposition in tissues contributes to the clinical manifestations, including neurological symptoms and tendon xanthomas. Dyslipidemia and abnormal cholesterol metabolism may also contribute to the increased risk of atherosclerosis and cardiovascular complications observed in some CTX patients.
- cerebrotendinous xanthomatosis
- cholestanol
- cholesterol
- lipid
- chenodeoxycholic acid
1. Introduction
2. Cholesterol Metabolism in CTX
CTX originates from a deficiency in the activity of the sterol enzyme 27-hydroxylase. This disorder, therefore, compromises the alternative pathway’s function, altering the metabolism of cholesterol-derived sterols [6]. The alternative pathway has CDCA as its final product. With the impairment of this metabolic route already in the initial stages, there is a decrease in the production of this substance [2]. CDCA plays an important role in the metabolism of cholesterol, as it exercises control over the classical pathway through negative feedback, regulating the activity of cholesterol 7α-hydroxylase, which is responsible for the limiting step in the process of bile acid synthesis. Therefore, with CDCA deficiency, there is a stimulation of the classical pathway, leading to the accumulation of intermediates in the plasma and in various tissues (especially cholestanol), in addition to an increase in the excretion of bile alcohols [2,5,8][2][5][8]. Salen and Grundy (1973) used a radioactive cholestanol labeling method in hospitalized patients to observe the metabolism of cholesterol, cholestanol and bile acids in people affected by CTX. They observed that the plasma cholestanol concentration, miscible molecules and cholestanol synthesis rates were 2–5 times higher in CTX patients when compared with the controls [33][16]. Accumulation of lipid metabolites can lead to pathological repercussions throughout the organism [15]. Salen et al. (1991) [16][17] verified that the proportions of plasmatic cholestanol, which are normally 0.1–0.2% of total cholesterols, were 10–100 times higher in patients with CTX and could reach 2% levels. Furthermore, this proportion can reach up to 50% in the CNS and up to 10% in tendons and the bile. The loss of function of the enzyme CYP27A1 has been reported in certain types of cancer, such as bladder urothelial carcinoma, breast invasive ductal carcinoma, renal clear cell carcinoma, prostate adenocarcinoma and cutaneous melanoma [34][18]. Cholesterol availability promotes bladder cancer cell proliferation in vitro, and CYP27A1 activity leads to 27-hydroxycholesterol production and decreased cholesterol levels, thus inhibiting cancer cell proliferation [35][19]. Thus, CYP27A1 functions as a cellular cholesterol sensor in cancer cells. The relationship between CTX and cancer predisposition as well as a possible effect of CDCA in regulating this pathway in cancer warrant further studies. The mechanisms by which the accumulation of cholesterol metabolites in the CNS occurs are still not precisely known, as cholestanol has a limited ability to cross the blood–brain barrier (BBB). Among the main hypotheses are that the precursor 7α-hydroxy-4-cholesten-3-one crosses the BBB more easily and can be converted into cholestanol by neurons, microglia and astrocytes. In addition, high levels of cholestanol and apolipoprotein B were found in the cerebrospinal fluid (CSF) of patients with CTX, indicating a possible blood–brain barrier dysfunction in these patients [36][20]. Inoue et al. (1999) [37][21] conducted an experiment with rats on a hypercholestanolemic diet and concluded that cholestanol induces apoptosis of the cerebellar neuronal cells, especially for Purkinje cells, a factor that led the rats to present ataxia and tremor. Bogaert et al. (1969) [38][22]. described the autopsy of ataxic CTX patients, demonstrating the destruction of the dentate and fastigial nucleus, in addition to a reduction in Purkinje cells. Those histologic alterations were manifested in magnetic resonance neuroimaging studies as signal intensity changes in the deep cerebellar white matter and particularly in the dentate nucleus (Figure 1).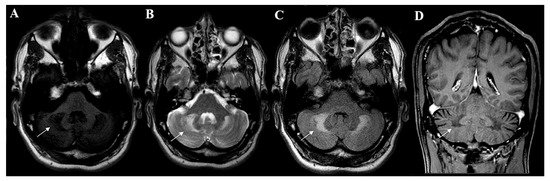
3. Metabolic Abnormalities and Laboratory Diagnosis of CTX
Cerebrotendinous xanthomatosis is a biochemical defect that comes with identifiable metabolic changes. The disruption of the classic pathway of cholesterol metabolism generates precursor accumulation, which is identified in the serum, CSF, urine, bile and traditionally affected CTX tissues. These biochemical markers are useful in both diagnosis and treatment follow-ups.4. CTX Treatment and Its Effect on Metabolism
Chenodeoxycholic acid (CDCA), an exogen bile acid, is considered the standard treatment for the disease and is the most efficient option for reverting the biochemical abnormalities of CTX and modifying the disease’s course [12,13,15,33,61,78,79,80,81,82][12][13][15][16][23][24][25][26][27][28]. The main objectives of CDCA therapy are to reduce the synthesis of cholesterol, the plasmatic concentrations of cholestanol and the accumulation of cholestanol [18][29], providing better outcomes for patients [83][30]. Many studies evaluated the metabolic effects of CDCA therapy in CTX patients. The main metabolic alteration provoked by the treatment was a reduction in serum cholestanol to normal levels in the majority of patients [1,7,12,14,15,33,40,44,53,54,68,69,70,79,84,85,86,87,88,89,90,91][1][7][12][14][15][16][25][31][32][33][34][35][36][37][38][39][40][41][42][43][44][45]. A reduction in cholestanol titers in the CSF and blood cell membranes was also reported [1,16,68,79,92][1][17][25][35][46]. It is possible that CDCA also lowers the BBB permeability to serum cholestanol, reducing the accumulation of this metabolite in the CNS [78,93][24][47]. However, the reduction in cholestanol levels in response to therapy is slow compared with other biomarkers [56,83][30][48]. Several studies reported that CDCA therapy also lowers the high bile alcohol titers in the serum, bile and urine [1,7,40,44,56,71,79,83,84,85,86,94,95,96][1][7][25][30][31][32][38][39][40][48][49][50][51][52]. The normalization of serum bile alcohol levels and urinary and biliary excretion of these metabolites demonstrates CDCA’s capability to inhibit abnormal bile acid synthesis [56,72,83,94][30][48][50][53]. The reduction in the serum levels of bile alcohols occurs before the normalization of serum cholestanol. The bile acid serum and urine titers also decrease with treatment [44,56][32][48], and CDCA represents the main bile compound with a parallel reduction in cholic and ursodeoxycholic acid. The titers of both the tetrols (represented by 5β-cholestane-3α, 7α, 12α and 25-tetrol) and pentols (represented by 5β-cholestane-3α, 7α, 12α, 23R and 25-pentol, 5β-cholestane-3α, 7α, 12α, 24ξ and 25-pentol and 5β-cholestane-3α, 7α, 12α, 22ξ and 25-pentol) in the urine and serum were reduced [56][48]. Different papers have observed different cholesterol responses to treatment with CDCA. In general, the serum cholesterol concentration remains stable with treatment [1,40][1][31]. Some studies have observed a reduction in cholesterol synthesis with CDCA, but no considerable changes were observed in the serum concentration of this molecule [44,97,98,99][32][54][55][56]. Despite this, older trials have evaluated cases of patients who had increased serum cholesterol levels after starting this therapy [56,97][48][54]. In addition, CDCA caused a reduction in serum HDL [100][57] and LDL catabolism [97][54]. It was also seen to reduce the susceptibility of LDL to oxidation [100][57], preventing the formation of oxidized LDL, an important component of xanthomas [100,101,102,103,104][57][58][59][60][61]. Decreases in 7α-hydroxycholesterol [1[1][55],98], 7a-hydroxy-4-cholesten-3-one (7α-HCO/7αC4) [1[1][7][30][31][34][40][41][43][44][45][56],7,40,54,83,86,87,89,90,91,99], lathosterol and lanosterol were also reported. The levels of other sterols, such as campesterol and sitosterol, were also lowered during treatment [1,40,44,54,83,89,99][1][30][31][32][34][43][56]. CDCA also induced a reduction in A1 apolipoprotein, B apolipoprotein and albumin in CSF, indicating the reestablishment of the selective permeability of the BBB [79][25]. The biochemical effects of CDCA therapy in CTX patients are achieved by inhibiting the classic pathway of cholesterol metabolism via negative feedback over the 7α-hydroxylase enzyme [78,83[24][30][50][62],94,105], reducing abnormal bile acid synthesis [3,40,83,97,99,106][3][30][31][54][56][63]. With the reduction in bile acid synthesis, the production of intermediate metabolites such as 7α-hydroxy-4-cholesten-3-one [49,54,89,90,99][34][43][44][56][64] and cholestanol [12,83,94,97,99][12][30][50][54][56] is lowered. Excretion of bile alcohols and cholesterol consumption, which stimulates de novo synthesis in a feedback loop, are also inhibited [40,44,83,107][30][31][32][65]. Aside from CDCA therapy, several studies reported different responses to alternative treatments. A well-studied therapy is the use of cholic acid, which showed clinical improvement or stability in some patients [105,108][62][66]. Some of the results obtained with the administration of cholic acid were a reduction in cholestanol blood and CSF levels [58[62][66][67],105,108], in bile acid synthesis, in urinary excretion of bile alcohol and in the abnormal bile acid tilter in urine [105][62]. Some efficacy was observed in the inhibition of 7α-hydroxylase enzyme activity [105,108][62][66]. In a 2019 study with CA, 53% of patients had reduced cholestanol levels, and none had adverse effects [108][66]. However, cholic acid is not as effective as CDCA, presenting a much smaller capacity for reversing biochemical abnormalities [109,110,111,112,113][68][69][70][71][72]. In general, there are contradictory results concerning the utility of cholic acid in CTX treatment and no consensus on its beneficial effects [13,106,114][13][63][73]. Despite this, cholic acid is often used when patients present side effects of CDCA [105,108,115][62][66][74]. Another possible treatment that has been considered is the use of HMG-CoA inhibitors. Controversial results have been observed regarding the clinical and metabolic response to this treatment, which vary among articles [2,5,11][2][5][11]. Several studies reported beneficial effects of statin use in reducing cholestanol [18[29][39][44][66][67][75][76][77],58,85,90,108,116,117,118], cholesterol and other plant sterol levels and improving lipoprotein and cholesterol metabolism [13,84,89,119][13][38][43][78]. In some studies, clinical improvement was observed with the association of statins with CDCA [81,84][27][38]. In a consensus statement, using the Delphi method, the association of statins to CDCA was suggested to improve or stabilize the prognoses of patients [13]. However, in other studies, statins failed to decrease abnormal bile acid production or stabilize symptoms [56,119][48][78]. Other previously tested treatments that did not achieve satisfactory results are ursodeoxycholic acid (UDCA), LDL apheresis, cholestyramine and clofibrate [13,33,71,83,84,96,109,110,111,120,121,122,123][13][16][30][38][49][52][68][69][70][79][80][81][82].5. Diet Effects in CTX
Currently, there is limited evidence on the association between cerebrotendinous xanthomatosis and dietary patterns, as very few studies investigated either the pathological or therapeutic potentials of one’s diet. In mice and rats, cholestanol ingestion can increase the cholestanol concentration in the plasma, liver and cerebellum of these animals compared with a control group with no such diet alteration [124,125][83][84]. In another study with CTX animal models fed cholestanol, the rats showed lipid accumulation in the Purkinje cells of the cerebellum, while the mice showed corneal opacifications without the presence of xanthomas [126][85]. A reduction in the plasmatic concentration of cholesterol was also noted in the rat models [124[83][84],125], suggesting there might be competition between cholestanol and cholesterol for intestinal absorption, even though cholestanol is known to be more poorly absorbed than cholesterol [125][84]. The prevalence of cardiovascular disease (CVD) can reach 10–20% in CTX, leading to coronary artery disease at an early age [4,15,127][4][15][86]. In this context, patients with CTX must be screened for CVD and receive dietary recommendations for atherosclerosis prevention [128][87]. A clinical trial reported clinical improvement in patients treated with a cholesterol-restricted diet in addition to conventional pharmacologic treatment with CDCA. However, a direct association was not established between dietary changes and the observed outcomes [129][88].References
- Höflinger, P.; Hauser, S.; Yutuc, E.; Hengel, H.; Griffiths, L.; Radelfahr, F.; Howell, O.W.; Wang, Y.; Connor, S.L.; Duell, P.B.; et al. Metabolic profiling in serum, cerebrospinal fluid, and brain of patients with cerebrotendinous xanthomatosis. J. Lipid Res. 2021, 62, 100078.
- Koyama, S.; Sekijima, Y.; Ogura, M.; Hori, M.; Matsuki, K.; Miida, T.; Harada-Shiba, M. Cerebrotendinous Xanthomatosis: Molecular Pathogenesis, Clinical Spectrum, Diagnosis, and Disease-Modifying Treatments. J. Atheroscler. Thromb. 2021, 28, 905–925.
- Nóbrega, P.R.; Bernardes, A.M.; Ribeiro, R.M.; Vasconcelos, S.C.; Araújo, D.A.B.S.; Gama, V.C.d.V. Cerebrotendinous Xanthomatosis: A practice review of pathophysiology, diagnosis, and treatment. Front. Neurol. 2022, 13, 1049850.
- Salen, G.; Steiner, R.D. Epidemiology, diagnosis, and treatment of cerebrotendinous xanthomatosis (CTX). J. Inherit. Metab. Dis. 2017, 40, 771–781.
- Nie, S.; Chen, G.; Cao, X.; Zhang, Y. Cerebrotendinous xanthomatosis: A comprehensive review of pathogenesis, clinical manifestations, diagnosis, and management. Orphanet J. Rare Dis. 2014, 9, 179.
- Gong, J.Y.; Setchell, K.D.R.; Zhao, J.; Zhang, W.; Wolfe, B.; Lu, Y.; Lackner, K.; Knisely, A.S.; Wang, N.L.; Hao, C.Z.; et al. Severe Neonatal Cholestasis in Cerebrotendinous Xanthomatosis: Genetics, Immunostaining, Mass Spectrometry. J. Pediatr. Gastroenterol. Nutr. 2017, 65, 561–568.
- Verrips, A.; Dotti, M.T.; Mignarri, A.; Stelten, B.M.L.; Verma, S.; Federico, A. The safety and effectiveness of chenodeoxycholic acid treatment in patients with cerebrotendinous xanthomatosis: Two retrospective cohort studies. Neurol. Sci. 2020, 41, 943–949.
- Russell, D.W. The enzymes, regulation, and genetics of bile acid synthesis. Annu. Rev. Biochem. 2003, 72, 137–174.
- Clayton, P.T.; Verrips, A.; Sistermans, E.; Mann, A.; Mieli-Vergani, G.; Wevers, R. Mutations in the sterol 27-hydroxylase gene (CYP27A) cause hepatitis of infancy as well as cerebrotendinous xanthomatosis. J. Inherit. Metab. Dis. 2002, 25, 501–513.
- Atallah, I.; San Millán, D.; Benoît, W.; Campos-Xavier, B.; Superti-Furga, A.; Tran, C. Spinal Cerebrotendinous Xanthomatosis: A case report and literature review. Mol. Genet. Metab. Rep. 2021, 26, 100719.
- Mignarri, A.; Gallus, G.N.; Dotti, M.T.; Federico, A. A suspicion index for early diagnosis and treatment of cerebrotendinous xanthomatosis. J. Inherit. Metab. Dis. 2014, 37, 421–429.
- Berginer, V.M.; Abeliovich, D. Genetics of cerebrotendinous xanthomatosis (CTX): An autosomal recessive trait with high gene frequency in Sephardim of Moroccan origin. Am. J. Med. Genet. 1981, 10, 151–157.
- Stelten, B.M.L.; Dotti, M.T.; Verrips, A.; Elibol, B.; Falik-Zaccai, T.C.; Hanman, K.; Mignarri, A.; Sithole, B.; Steiner, R.D.; Verma, S.; et al. Expert opinion on diagnosing, treating and managing patients with cerebrotendinous xanthomatosis (CTX): A modified Delphi study. Orphanet J. Rare Dis. 2021, 16, 353.
- Amador, M.D.M.; Masingue, M.; Debs, R.; Lamari, F.; Perlbarg, V.; Roze, E. Treatment with chenodeoxycholic acid in Cerebrotendinous Xanthomatosis: Clinical, neurophysiological, and quantitative brain structural outcomes. J. Inherit. Metab. Dis. 2018, 41, 799–807.
- Duell, P.B.; Salen, G.; Eichler, F.S.; DeBarber, A.E.; Connor, S.L.; Casaday, L. Diagnosis, treatment, and clinical outcomes in 43 cases with Cerebrotendinous Xanthomatosis. J. Clin. Lipidol. 2018, 12, 1169–1178.
- Salen, G.; Grundy, S.M. The metabolism of cholestanol, cholesterol, and bile acids in cerebrotendinous xanthomatosis. J. Clin. Investig. 1973, 52, 2822–2835.
- Salen, G.; Shefer, S.; Berginer, V. Biochemical abnormalities in cerebrotendinous xanthomatosis. Dev. Neurosci. 1991, 13, 363–370.
- Petar Brlek, P.; Bulić, L.; Weinberger, D.G.; Bošnjak, J.; Pavlović, T.; Tomić, S.; Dupan, Z.K.; Borić, I.; Primorac, D. Successful Treatment of a Rare Cholesterol Homeostasis Disorder Due to CYP27A1 Gene Mutation with Chenodeoxycholic Acid Therapy. Biomedicines 2023, 11, 1430.
- Liang, Z.; Chen, Y.; Wang, L.; Li, D.; Yang, X.; Ma, G.; Wang, Y.; Li, Y.; Zhao, H.; Liang, Y.; et al. CYP27A1 inhibits bladder cancer cells proliferation by regulating cholesterol homeostasis. Cell Cycle 2019, 18, 34–45.
- Menkes, J.H.; Schimschock, J.R.; Swanson, P.D. Cerebrotendinous Xanthomatosis: The Storage of Cholestanol Within the Nervous System. Arch. Neurol. 1968, 19, 47–53.
- Inoue, K.; Kubota, S.; Seyama, Y. Cholestanol induces apoptosis of cerebellar neuronal cells. Biochem. Biophys. Res. Commun. 1999, 256, 198–203.
- Van Bogaert, L.; Philippart, M.; De Barsy, T. Nouvelles recherches sur la xanthomatose cérébro-tendineuse . Rev. Neurol. 1969, 121, 98–100.
- Martini, G.; Mignarri, A.; Ruvio, M.; Valenti, R.; Franci, B.; Del Puppo, M.; Federico, A.; Nuti, R.; Dotti, M.T. Long-term bone density evaluation in cerebrotendinous xanthomatosis: Evidence of improvement after chenodeoxycholic acid treatment. Calcif. Tissue Int. 2013, 92, 282–286.
- Bonney, H.; de Silva, R.; Giunti, P.; Greenfeld, J.; Hunt, B.; Ataxia, U.K. Management of the Ataxias towards Best Clinical Practice. 2016. Available online: https://www.ataxia.org.uk/wp-content/uploads/2020/11/Ataxia_UK_Medical_Guidelines_Third_Edition._v3m_Dec_2016_-_updated_Sep_2019.pdf (accessed on 30 June 2021).
- Salen, G.; Berginer, V.; Shore, V.; Horak, I.; Horak, E.; Tint, G.S.; Shefer, S. Increased concentrations of cholestanol and apolipoprotein B in the cerebrospinal fluid of patients with cerebrotendinous xanthomatosis. Effect of chenodeoxycholic acid. N. Engl. J. Med. 1987, 316, 1233–1238.
- Samenuk, P.; Koffman, B.M. Chenodeoxycholic treatment of cerebrotendinous xanthomatosis. Neurology 2001, 56, 695–696.
- Mignarri, A.; Rossi, S.; Ballerini, M.; Gallus, G.N.; Del Puppo, M.; Galluzzi, P.; Federico, A.; Dotti, M.T. Clinical relevance and neurophysiological correlates of spasticity in cerebrotendinous xanthomatosis. J. Neurol. 2011, 258, 783–790.
- Ginanneschi, F.; Mignarri, A.; Mondelli, M.; Gallus, G.N.; Del Puppo, M.; Giorgi, S.; Federico, A.; Rossi, A.; Dotti, M.T. Polyneuropathy in cerebrotendinous xanthomatosis and response to treatment with chenodeoxycholic acid. J. Neurol. 2013, 260, 268–274.
- Burnett, J.R.; Moses, E.A.; Croft, K.D.; Brown, A.J.; Grainger, K.; Vasikaran, S.D.; Leitersdorf, E.; Watts, G.F. Clinical and biochemical features, molecular diagnosis and long-term management of a case of cerebrotendinous xanthomatosis. Clin. Chim. Acta 2001, 306, 63–69.
- Stelten, B.M.L.; Nijeholt, G.J.L.A.; Hendriks, E.; Kluijtmans, L.A.J.; Wevers, R.A.; Verrips, A. Long-term MRI findings in patients with Cerebrotendinous Xanthomatosis treated with chenodeoxycholic acid. Neurology 2022, 99, 559–566.
- Mignarri, A.; Magni, A.; Del Puppo, M.; Gallus, G.N.; Björkhem, I.; Federico, A.; Dotti, M.T. Evaluation of cholesterol metabolism in cerebrotendinous xanthomatosis. J. Inherit. Metab. Dis. 2016, 39, 75–83.
- De Sain-van der Velden, M.G.; Verrips, A.; Prinsen, B.H.; de Barse, M.; Berger, R.; Visser, G. Elevated cholesterol precursors other than cholestanol can also be a hallmark for CTX. J. Inherit. Metab. Dis. 2008, 31 (Suppl. S2), S387–S393.
- Panzenboeck, U.; Andersson, U.; Hansson, M.; Sattler, W.; Meaney, S.; Björkhem, I. On the mechanism of cerebral accumulation of cholestanol in patients with cerebrotendinous xanthomatosis. J. Lipid Res. 2007, 48, 1167–1174.
- DeBarber, A.E.; Connor, W.E.; Pappu, A.S.; Merkens, L.S.; Steiner, R.D. ESI-MS/MS quantification of 7α-hydroxy-4-cholesten-3-one facilitates rapid, convenient diagnostic testing for cerebrotendinous xanthomatosis. Clin. Chim. Acta. 2010, 411, 43–48.
- Di Taranto, M.D.; Gelzo, M.; Giacobbe, C.; Gentile, M.; Marotta, G.; Savastano, S.; Dello Russo, A.; Fortunato, G.; Corso, G. Cerebrotendinous xanthomatosis, a metabolic disease with different neurological signs: Two case reports. Metab. Brain Dis. 2016, 31, 1185–1188.
- Björkhem, I. Cerebrotendinous xanthomatosis. Curr. Opin. Lipidol. 2013, 24, 283–287.
- Haas, D.; Gan-Schreier, H.; Langhans, C.D.; Rohrer, T.; Engelmann, G.; Heverin, M.; Russell, D.W.; Clayton, P.T.; Hoffmann, G.F.; Okun, J.G. Differential diagnosis in patients with suspected bile acid synthesis defects. World J. Gastroenterol. 2012, 18, 1067–1076.
- Verrips, A.; Wevers, R.A.; Van Engelen, B.G.; Keyser, A.; Wolthers, B.G.; Barkhof, F.; Stalenhoef, A.; De Graaf, R.; Janssen-Zijlstra, F.; Van Spreeken, A.; et al. Effect of simvastatin in addition to chenodeoxycholic acid in patients with cerebrotendinous xanthomatosis. Metabolism 1999, 48, 233–238.
- Bel, S.; Garcia-Patos, V.; Rodriguez, L.; Selvan, A.; Diaz, P.; Wolthers, B.G.; Castells, A. Cerebrotendinous xanthomatosis. J. Am. Acad. Dermatol. 2001, 45, 292–295.
- Stelten, B.M.L.; Huidekoper, H.H.; van de Warrenburg, B.P.C.; Brilstra, E.H.; Hollak, C.E.M.; Haak, H.R.; Kluijtmans, L.A.J.; Wevers, R.A.; Verrips, A. Long-term treatment effect in cerebrotendinous xanthomatosis depends on age at treatment start. Neurology 2019, 92, e83–e95.
- Van Heijst, A.F.; Verrips, A.; Wevers, R.A.; Cruysberg, J.R.; Renier, W.O.; Tolboom, J.J. Treatment and follow-up of children with cerebrotendinous xanthomatosis. Eur. J. Pediatr. 1998, 157, 313–316.
- Salen, G.; Tint, G.S.; Eliav, B.; Deering, N.; Mosbach, E.H. Increased formation of ursodeoxycholic acid in patients treated with chenodeoxycholic acid. J. Clin. Investig. 1974, 53, 612.
- Kuriyama, M.; Tokimura, Y.; Fujiyama, J.; Utatsu, Y.; Osame, M. Treatment of cerebrotendinous xanthomatosis: Effects of chenodeoxycholic acid, pravastatin, and combined use. J. Neurol. Sci. 1994, 125, 22–28.
- Björkhem, I.; Skrede, S.; Buchmann, M.S.; East, C.; Grundy, S. Accumulation of 7α-hydroxy-4-cholesten-3-one and cholesta-4, 6-dien-3-one in patients with cerebrotendinous xanthomatosis: Effect of treatment with chenodeoxycholic acid. Hepatology 1987, 7, 266–271.
- Björkhem, K.; Muri-Boberg, E.; Leitersdorf. Inborn errors in bile acid biosynthesis and storage of sterols other than cholesterol. In The Metabolic Bases of Inherited Diseases; Scriver, C.R., Beaudet, A.L., Sly, W.S., Valle, D., Eds.; McGraw Hill Publishing Co.: New York, NY, USA, 2001; pp. 2961–2988.
- Salen, G.; Shefer, S.; Berginer, V.M. Familial diseases with storage of sterols other than cholesterol: Cerebrotendinous xanthomatosis and sitosterolemia with xanthomatosis. In The Metabolic Basis of Inherited Disease, 5th ed.; Stanbury, J.B., Wyngaarden, J., Fredrickson, D.S., Eds.; McGraw-Hill Book: New York, NY, USA, 1983; pp. 713–730.
- Oftebro, H.; Bjorkhem, I.; Skrede, S.; Schreiner, A.; Pederson, J.I. Cerebrotendinous xanthomatosis: A defect in mitochondrial 26-hydroxylation required for normal biosynthesis of cholic acid. J. Clin. Investig. 1980, 65, 1418–1430.
- Salen, G.; Batta, A.K.; Tint, G.S.; Shefer, S. Comparative effects of lovastatin and chenodeoxycholic acid on plasma cholestanol levels and abnormal bile acid metabolism in cerebrotendinous xanthomatosis. Metabolism. 1994, 43, 1018–1022.
- Wolthers, B.G.; Volmer, M.; van der Molen, J.; Koopman, B.J.; de Jager, A.E.; Waterreus, R.J. Diagnosis of cerebrotendinous xanthomatosis (CTX) and effect of chenodeoxycholic acid therapy by analysis of urine using capillary gas chromatography. Clin. Chim. Acta. 1983, 131, 53–65.
- Batta, A.K.; Shefer, S.; Batta, M.; Salen, G. Effect of chenodeoxycholic acid on biliary and urinary bile acids and bile alcohols in cercbrotendinous xanthomatosis: Monitoring by high performance liquid chromatography. J. Lipid Res. 1985, 26, 690–698.
- Batta, A.K.; Salen, G.; Shefer, S.; Tint, G.S.; Batta, M. Increased plasma bile alcohol glucuronides in patients with cerebrotendinous xanthomatosis: Effect of chenodeoxycholic acid. J. Lipid Res. 1987, 28, 1006–1012.
- Batta, A.K.; Salen, G.; Tint, G.S. Hydrophilic 7β-hydroxy bile acids, lovastatin, and cholestyramine are ineffective in the treatment of Cerebrotendinous Xanthomatosis. Metabolism 2004, 53, 556–562.
- Setoguchi, T.; Salen, G.; Tint, G.S.; Mosbach, E.H. A biochemical abnormality in cerebrotendinous xanthomatosis. Impairment of bile acid biosynthesis associated with incomplete degradation of the cholesterol side chain. J. Clin. Investig. 1974, 53, 1393–1401.
- Tint, G.S.; Ginsberg, H.; Salen, G.; Le, N.; Shefer, S. Chenodeoxycholic acid normalizes elevated lipoprotein secretion and catabolism in cerebrotendinous xanthomatosis. J. Lipid Res. 1989, 30, 633–640.
- Blaabjerg, M.; Marjanovic, D. Cerebrotendinøs xantomatose er en sjælden neurologisk sygdom med en specifik behandling . Ugeskr Laeger 2013, 175, 285–286. (In Danish)
- Salen, G.; Meriwether, T.W.; Nicolau, G. Chenodeoxycholic acid inhibits increased cholesterol and cholestanol synthesis in patients with cerebrotendinous xanthomatosis. Biochem. Med. 1975, 14, 57–74.
- Kinoshita, M.; Kawamura, M.; Fujita, M.; Hirota, D.; Suda, T.; Taki, M.; Kusano, J.; Takao, K.; Takenaka, H.; Kubota, S.; et al. Enhanced susceptibility of LDL to oxidative modification in a CTX patient:—role of chenodeoxycholic acid in xanthoma formation. J. Atheroscler. Thromb. 2004, 11, 167–172.
- Bjorkhem, I.; Skrede, S. Familial disease with storage of sterols other than cholesterol: Cerebrotendinous xanthomatosis and phytosterolemia. In The Metabolic Basis of Inherited Disease, 6th ed.; Scriver, C.R., Beaudet, A.L., Sly, W.S., Valle, D., Eds.; McGraw-Hill: New York, NY, USA, 1989; pp. 1283–1302.
- Goldstein, J.L.; Ho, Y.K.; Basu, S.K.; Brown, M.S. Binding site of macrophages that mediate uptake and degradation of acetylated low density lipoprotein, producing massive cholesterol deposition. Proc. Natl. Acad. Sci. USA 1979, 76, 333–337.
- Sparrow, C.P.; Parthasarathy, S.; Steinberg, D. A macrophage receptor that recognizes oxidized LDL but not acetylated LDL. J. Biol. Chem. 1989, 264, 2599–2604.
- Witztum, J.L.; Steinberg, D. Role of oxidized low density-lipoprotein in atherogenesis. J. Clin. Investig. 1991, 88, 1785–1792.
- Koopman, B.J.; Wolthers, B.G.; van der Molen, J.C.; Waterreus, R.J. Bile acid therapies applied to patients suffering from cerebrotendinous xanthomatosis. Clin. Chim. Acta 1985, 152, 115–122.
- Ellis, E.; Axelson, M.; Abrahamsson, A.; Eggertsen, G.; Thörne, A.; Nowak, G.; Ericzon, B.-G.; Björkhem, I.; Einarsson, C. Feedback regulation of bile acid synthesis in primary human hepatocytes: Evidence that CDCA is the strongest inhibitor. Hepatology 2003, 38, 930–938.
- Sekijima, Y.; Koyama, S.; Yoshinaga, T.; Koinuma, M.; Inaba, Y. Nationwide survey on cerebrotendinous xanthomatosis in Japan. J. Hum Genet. 2018, 63, 271–280.
- Berginer, V.M.; Berginer, J.; Korczyn, A.D.; Tadmor, R. Magnetic resonance imaging in cerebrotendinous xanthomatosis: A prospective clinical and neuroradiological study. J. Neurol. Sci. 1994, 122, 102–108.
- Mandia, D.; Besson, G.; Lamari, F.; Castelnovo, G.; Curot, J.; Duval, F.; Giral, P.; Lecerf, J.M.; Roland, D.; Pierdet, H.; et al. Cholic acid as a treatment for cerebrotendinous xanthomatosis in adults. J. Neurol. 2019, 266, 2043–2050.
- Pierre, G.; Setchell, K.; Blyth, J.; Preece, M.A.; Chakrapani, A.; McKiernan, P. Prospective treatment of cerebrotendinous xanthomatosis with cholic acid therapy. J. Inherit. Metab. Dis. 2008, 31, S241–S245.
- Makishima, M.; Okamoto, A.Y.; Repa, J.J.; Tu, H.; Learned, R.M.; Luk, A.; Hull, M.V.; Lustig, K.D.; Mangelsdorf, D.J.; Shan, B. Identification of a nuclear receptor for bile acids. Science 1999, 284, 1362–1365.
- Parks, D.J.; Blanchard, S.G.; Bledsoe, R.K.; Chandra, G.; Consler, T.G.; Kliewer, S.A.; Stimmel, J.B.; Willson, T.M.; Zavacki, A.M.; Moore, D.D.; et al. Bile acids: Natural ligands for an orphan nuclear receptor. Science 1999, 284, 1365–1368.
- Wang, H.B.; Chen, J.; Hollister, K.; Sowers, L.C.; Forman, B.M. Endogenous bile acids are ligands for the nuclear receptor FXR/BAR. Mol. Cell 1999, 3, 543–553.
- Einarsson, C.; Hillebrant, C.G.; Axelson, M. Effects of treatment with deoxycholic acid and chenodeoxycholic acid on the hepatic synthesis of cholesterol and bile acids in healthy subjects. Hepatology 2001, 33, 1189–1193.
- Huidekoper, H.H.; Vaz, F.M.; Verrips, A.; Bosch, A.M. Hepatotoxicity due to chenodeoxycholic acid supplementation in an infant with cerebrotendinous xanthomatosis: Implications for treatment. Eur. J. Pediatr. 2016, 175, 143–146.
- Medscape. Available online: https://emedicine.medscape.com/article/1418820-overview (accessed on 30 June 2021).
- Bartholdi, D.; Zumsteg, D.; Verrips, A.; Wevers, R.A.; Sistermans, E.; Hess, K.; Jung, H.H. Spinal phenotype of Cerebrotendinous Xanthomatosis—A pitfall in the diagnosis of multiple sclerosis. J. Neurol. 2004, 251, 105–107.
- Lewis, B.; Mitchell, W.D.; Marenah, C.B.; Cortese, C.; Reynolds, E.H.; Shakir, R. Cerebrotendinous xanthomatosis: Biochemical response to inhibition of cholesterol synthesis. Br. Med. J. 1983, 287, 21–22.
- Nakamura, T.; Matsuzawa, Y.; Takemura, K.; Kubo, M.; Miki, H.; Tarui, S. Combined treatment with chenodeoxycholic acid and pravastatin improves plasma cholestanol levels associated with marked regression of tendon xanthomas in cerebrotendinous xanthomatosis. Metabolism 1991, 40, 741–746.
- Black, M.M.; Gawkrodger, D.J.; Seymour, C.A.; Weismann, K. Metabolic and nutritional disorders. In Rook/Wilkinson/Ebling: Textbook of Dermatology, 6th ed.; Champion, R.H., Burton, J.L., Burns, T., Breathnach, S., Eds.; Blackwell Science: London, UK, 1998; pp. 2577–2677.
- Peynet, J.; Laurent, A.; De Liege, P.; Lecoz, P.; Gambert, P.; Legrand, A.; Mikol, J.; Warnet, A. Cerebrotendinous xanthomatosis: Treatments with simvastatin, lovastatin, and chenodeoxycholic acid in 3 siblings. Neurology 1991, 41, 434–436.
- Koopman, B.J.; Wolthers, B.G.; van der Moten, J.C.; Nagel, G.T.; Waterreus, R.J.; Oosterhuis, H.J.G.H. Capillary gas chromatographic determinations of urinary bile acids and bile alcohols in CTX-patients proving the ineffectivity of ursodeoxycholic acid treatment. Clin. Chim. Acta 1984, 142, 103–111.
- Koopman, B.J.; Wolthers, B.G.; van der Molen, J.C.; Nagel, G.T.; Kruizinga, W. Abnormal urinary bile acids in a patient suffering from cerebrotendinous xanthomatosis during oral administration of ursodeoxycholic acid. Biochim. Biophys. Acta 1987, 917, 238–246.
- Dotti, M.T.; Lütjohann, D.; von Bergmann, K.; Federico, A. Normalisation of serum cholestanol concentration in a patient with Cerebrotendinous Xanthomatosis by combined treatment with chenodeoxycholic acid, simvastatin and LDL apheresis. Neurol. Sci. 2004, 25, 185–191.
- Ito, S.; Kuwabara, S.; Sakakibara, R.; Oki, T.; Arai, H.; Oda, S.; Hattori, T. Combined treatment with LDL-apheresis, chenodeoxycholic acid and HMG-CoA. J. Neurol. Sci. 2003, 216, 179–182.
- Byun, D.S.; Kasama, T.; Shimizu, T.; Yorifuji, H.; Seyama, Y. Effect of cholestanol feeding on sterol concentrations in the serum, liver, and cerebellum of mice. J. Biochem. 1988, 103, 375–379.
- Shefer, S.; Hauser, S.; Salen, G.; Zaki, F.G.; Bullock, J.; Salgado, E.; Shevitz, J. Comparative effects of cholestanol and cholesterol on hepatic sterol and bile acid metabolism in the rat. J. Clin. Investig. 1984, 74, 1773–1781.
- Yousuke, S. Cholestanol metabolism, molecular pathology, and nutritional implications. J. Med. Food 2003, 6, 217–224.
- Valdivielso, P.; Calandra, S.; Duran, J.C.; Garuti, R.; Herrera, E.; Gonzalez, P. Coronary heart disease in a patient with cerebrotendinous xanthomatosis. J. Intern Med. 2004, 255, 680–683.
- Malco, R.; Nestor, W.; Marcelo, M. Cardiac involvement in movement disorders. Mov. Disord. Clin. Pract. 2021, 8, 651–668.
- Zhang, S.; Li, W.; Zheng, R.; Zhao, B.; Zhang, Y.; Zhao, D.; Zhao, C.; Yan, C.; Zhao, Y. Cerebrotendinous xanthomatosis with peripheral neuropathy: A clinical and neurophysiological study in Chinese population. Ann. Transl. Med. 2020, 8, 1372.
