Your browser does not fully support modern features. Please upgrade for a smoother experience.
Please note this is a comparison between Version 1 by Maria Antoniadou and Version 2 by Alfred Zheng.
Bacteria populations can be spread during ongoing dental procedures when dentists are using high-speed handpieces and come into direct contact with the wounds of the patient undergoing treatment. There is a risk of water backflow into the dental unit waterline system from the handpieces known under the term of the suck-back phenomenon.
- water quality
- infection control
- handpieces
- dental unit
1. Introduction
Sustainable entrepreneurship in the field of health depends on the breathing space that managers and employees give to nature and its resources [1]. The recent COVID-19 pandemic made the need to protect and restore natural resources and integrate human activities more effectively even more imperative [2]. The pandemic has raised awareness of the interconnectedness of our own health and the health of ecosystems [3][4][5][3,4,5]. It is vital then that stakeholders of the field avoid becoming stuck in destructive habits of the past towards environmentalism and protect air, water, and natural resources [6][7][8][9][10][11][12][6,7,8,9,10,11,12].
Water pollution is a key driver of biodiversity loss [12][13][12,13] and has harmful effects on our health and environment [14]. Biodiversity is affected by the release of nutrients, chemical pesticides, pharmaceuticals, hazardous chemicals, municipal and industrial wastewater, and other wastes, including litter and plastics, into water resources [15]. Dental offices have long waterline networks. In the field of eco-friendly dental practices, the reduction of water waste and the quality of water in the waterline network of the office and the dental unit, but also the prevention of infections, are challenges that every dentist must face [16][17][16,17]. Increasingly, low water quality has been recognized as a possible cause of biohazards and the spread of infections in the dental office [18][19][18,19]. A biofilm that forms inside the pipes of a building could contaminate the entire water supply network of that building, including the dental office [20]. Furthermore, within the dental clinic, water spreads as an aerosol, increasing both bacterial spread and the risk of infection to all people in the premises [12][21][22][23][24][12,21,22,23,24]. Oral flora [25] and human pathogens (e.g., Pseudomonas aeruginosa [26], various Legionella species (Legionella pneumophila) [27][28][27,28], non-tuberculous Mycobacterium species (Mycobacterium) [29], Helicobacter pylori [30] and other microorganisms including unicellular algae, bacteria, fungi, and protozoa [16][31][16,31]) have already been isolated from dental unit water systems [32]. They can coat and colonize almost any material in the dental clinic [33][34][33,34], especially the suction tube [16], forming biofilms. Biofilms in dental clinics have been shown to form a hazardous bacterial deposit, which can become resistant to various disinfectants [23][35][36][37][23,35,36,37] and serves as a reservoir that can enhance the number of floating (planktonic) microorganisms in the water used for dental treatment [38][39][40][38,39,40].
The trend and attention to this important matter is growing, in part due to the increasing needs for workplace safety for both workers and patients [12][41][12,41]. Good water quality is an important factor in ensuring the quality and safe operation of the dental practice [31][42][31,42]. The water network participates in all clinical protocols, in the antisepsis and disinfection procedures, the operation of the dental unit as well as all other areas (doctor’s office, waiting room, toilets, laboratory, rest room or kitchen). Infections in dental practices can occur very easily [13][43][44][13,43,44]. Therefore, there is considerable (and justified) attention to the sterilization protocols of dental instruments and handpieces [45], but less attention is usually paid to the treatment of water in the practice’s network even though it participates in these protocols [46][47][46,47] and may even cause an erosion effect in oral metal prostheses [48].
Biofilms within the waterlines of dental clinics originate from one of two possible sources of contamination: from the internal piping system using a direct supply from the public network or from the patient’s mouth [31][48][31,48]. The public water supply is not entirely sterile. Water circulating in the system of the city contains a diverse microbial flora which, depending on its type and concentration, is generally harmless to humans. However, under certain conditions, pathogenic microorganisms or opportunistic pathogens can reach the dental unit through the water supply chain [49]. The microbiological quality of the water samples collected throughout the city system does not necessarily correspond to the microbiological quality that could be detected at points closer to the dental practice [17][33][50][51][52][17,33,50,51,52].
2. Procedures and Systems for Water Quality Control in the Handpieces and the Dental Unit
Bacteria populations can be spread during ongoing dental procedures when dentists are using high-speed handpieces [53][54][55][56][57,58,59,60] and come into direct contact with the wounds of the patient undergoing treatment [57][61]. There is a risk of water backflow into the dental unit waterline system from the handpieces known under the term of the suck-back phenomenon [58][62]. High-speed handpieces, in the deceleration phase of cutting, have a centrifugal suction effect that forces them to retract organic material especially from their head [27][59][27,63]. For this reason, many handpieces are equipped with special anti-retraction valves, which hold the suctioned material in the rotor [57][61]. These valves may not provide a perfect blockage (depending on how well the handpiece is maintained) and any leakage can lead to bacterial colonies inside the handpiece body [60][64]. This is an ideal environment for bacteria to grow, increasing the risk of cross-contamination. Consequently, all modern dental clinics need to have integrated disinfection systems [26][60][61][26,64,65].
There are various devices, materials, and filters within or in parallel connection with the dental unit, which make it possible to limit the risk of contamination of the water circulating within its piping: (1) Chlorine dioxide is a powerful and effective disinfecting agent capable of producing and maintaining safe drinking water through oxidation rather than a chlorination reaction [38]. (2) Reverse osmosis is the safest and most widespread water treatment system in the world and can guarantee absolute water purity for the dental unit [62][66]. The osmotic membrane can process water to the molecular size, making its characteristics optimal in terms of color, smell, and organoleptic purity. (3) Electrolysis apparatuses that use only the chlorine normally present in municipal water, such as the Poseidon-S system, an additive-free disinfectant system described in the study of Fujita et al. [63][67] can also control microbial contamination in contaminated dental unit waterlines [32]. (4) Positive relevant results can also be guaranteed with plasma devices [64][68] or (5) acoustic waves at high energy [65][69]. It was mentioned that the efficacy of acoustic waves in preventing Streptococcus mutans adhesion on dental unit waterlines can be important [12]. For surgical procedures, sterile saline or sterile water should be used as the coolant/irrigant. Conventional dental units cannot reliably provide sterile water even when equipped with independent water tanks containing sterile water because the water-carrying path cannot be reliably sterilized [61][66][65,70].
The guidelines on infection control in dental healthcare settings issued by the US Centers for Disease Control and Prevention [11] recommend that the level of the heterotrophic plate counts (HPCs) in dental unit water should not exceed 500 CFU/mL [67][71]. Moreover, the American Dental Association (ADA) has set a limit of ≤200 CFU/mL on the heterotrophic bacterial load in water from dental unit waterlines [68][72]. In the EU, however, there is no current guideline regarding a dental unit’s waterlines, though in some countries the drinking water standard is used as a reference (≤500 colony forming units (CFU)/mL of water heterotrophic bacteria) [59][63]. For this reason, dental units are designed to include (a) self-contained water systems (e.g., independent water tank) combined with chemical treatment (e.g., periodic or continuous chemical microbicide treatment protocols), (b) systems in parallel connection with one or more dental units within the same dental office that clean or treat incoming water to remove or inactivate microorganisms throughout the network and (c) combinations of these methods (Figure 1).
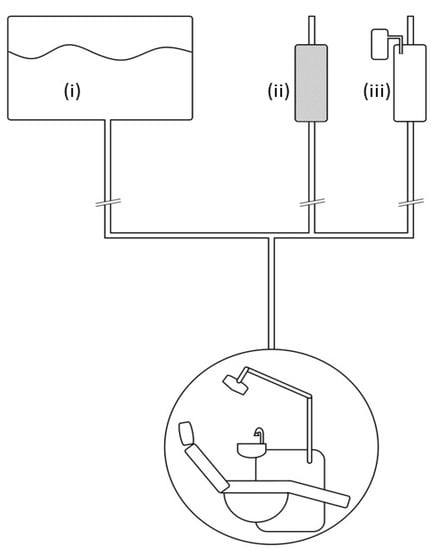
Figure 1. Graph showcasing various water treatment methods and arrangements within a dental practice: (i) Self-contained water systems (e.g., independent water tank) that supply the dental unit/s. (ii) Systems in line with one or more dental units within the same dental practice that filter incoming water. (iii) Systems in line with one or more dental units within the same dental practice that treat incoming water to remove or inactivate microorganisms throughout the network. These methods (i–iii) can also be used sequentially in line, e.g., tank combined with chemical treatment (periodic or continuous chemical microbicide treatment protocols) and filters.
When the treatment of patients is completed, specific protocols should be followed for flushing the suction network to reduce residual microbial contamination [12]. All incoming waterlines of the public water supply system within the dental practice (e.g., taps, dental unit water mains/waterlines and other dental equipment such as the suction mains) should be flushed [35][69][35,73]. There is no agreement on the optimal duration of flushing procedures, but the recommendations suggest that the procedures take from 1 to 5 min [70][74]. The time required may vary depending on the type and length of the network in the dental practice [11][60][70][11,64,74]. After flushing the incoming lines of the public water system, the dental facility waterlines should be disinfected according to manufacturer’s instructions [28][31][71][28,31,54].
