Please note this is a comparison between Version 2 by Alfred Zheng and Version 1 by Kyoko Hoshino.
Development of the sleep–wake rhythm has a significant effect on the physical and mental development of children. The sleep–wake rhythm is controlled by aminergic neurons in the brainstem’s ascending reticular activating system, which is associated with synaptogenesis and the promotion of brain development. Before evaluating a sleep disorder in a child, it is of paramount importance to evaluate, as a prerequisite, whether ‘the parent or guardian has a stable sleep rhythm’ or whether ‘the parent or guardian pays attention to the adequate environment in which the child sleeps well at night’. The sleep rhythm of the child changes with that of his or her guardian.
- sleep hygiene
- sleep–wake rhythm
- children
- autism
- Rett syndrome
- aminergic neuron
- Neurodevelopmental Disorders
1. Introduction
The mammalian circadian clock is controlled by the oscillation of clock genes, located in the hypothalamic suprachiasmatic nucleus, and trained by light in the environment [1]. Most mammalian genes exhibit daily fluctuations, making circadian expression rhythms the largest known regulatory network in normal physiology [2]. Humans have lived on Earth as diurnal mammalians over many years. Insufficient sleep and/or sleep disorders in adults are tightly correlated to cardiovascular disease, diabetes, accidents and injuries, stress, and neurocognitive/psychiatric symptoms [3]. Development of the sleep–wake rhythm has significant influences on the physical and mental development of children. From birth, the sleep–wake rhythm changes on a daily basis. The baby grows day by day, with increasing waking time, feeding, and playing over the first year.
The development of sleep–wake rhythms probably has a critical period, and is related to neurodevelopment [4]. By one year of age, most children eat three meals a day, sleep long hours at night, develop walking and language skills, and establish a diurnal rhythm as ‘humans living’ on the Earth. The nervous system and internal organs (digestive and endocrine systems) develop significantly in accordance with the sleep–wake rhythm [5]. Waking is controlled, not only by the aminergic neurons of the brainstem ascending reticular activating system, but also by orexin, histamine, and other neurotransmitters that are associated with synaptogenesis and promoting brain development. Arousal activates the autonomic nervous system and promotes the physical development of the respiratory, circulatory, and digestive systems [6].
2. Normal Development of the Sleep–Wake Rhythm
2.1. Development of Sleep–Wake Rhythm
It is important to consider the question ‘over how many months in infancy does the baby establish the sleep–wake rhythm?’ However, it is difficult to answer this question because it is influenced by nutritional methods and weight gain. The development of sleep–wake rhythms has been investigated by several studies over the years [7]. Ref [8] shows the development of sleep rhythms in a normal boy from the time of birth, and is frequently cited in Japan. The first few months of life are characterised by an ultradian rhythm in which the periods in the first few hours range in multiple levels of biological organization and adaptive significance in humans [9]. Sleep rhythms around two months of age become temporarily disordered as a free-running circadian rhythm; however, at around four months, babies gradually wake up in the morning, remain awake during the day, and sleep longer at night [10]. Children begin to distinguish between day and night by 3–4 months of age [10,11][10][11]. The transition between night-time and daytime sleep does not occur until approximately four months of age [5]. By six weeks of age, the child may sleep five to six hours continuously at night. This length increases to eight to nine hours at night by four months of age. Daytime sleep can be called ‘napping’. From six months to one year of age, daytime and night-time are determined more clearly, which means that the amplitudes of wakefulness and sleep are higher. The late infant begins to stay awake longer during the day and decreases the number of naps and awakenings during the night. By the age of one year, afternoon naps decrease and night-time awakenings almost disappear [12]. The basic structure of an infant’s circadian rhythms as a diurnal animal is established by around one year of age. In a cohort study of 194 cases, Hayama [13] found that infants with nocturnal rhythms at 4 months of age had disturbed the establishment of sleep–wake rhythms at 10 months of age. The pathophysiological mechanism of ‘night-time crying’ is unknown. Fukumizu [14] focused on the prevalence of night-time crying in healthy Japanese children and reported that 60% of them experienced night-time crying. Most children fall asleep again, which means they are self-soothing. Sleep problems in childhood may be caused by a dysfunction of the self-soothing mechanism. At 3–4 years of age, a sleep–wake rhythm was firmly established with a nap in the afternoon. The nap disappears between the ages of five and six and the circadian rhythm develops into that of adults. In terms of sleep duration at night, sleep lengthens as development progresses. New-borns sleep 16–17 h, gradually decreasing to 14–16 h at four months of age and 13–14 h at six to eight months of age. Night feeding decreases and daytime meals increase, according to development. The normal number of night-time feedings recorded by actigraphy was shown to decrease to one by one year of age [12]. The diurnal rhythms of the autonomic nervous system, such as body temperature, heart rate, and urination, are established during the first five months [15]. The earliest rhythm begins at approximately two to three weeks of age. Taken together, the physical development of children responds to the development of sleep–wake rhythms. The hypothesis asserting the relationship between irregular sleep rhythms and developmental disorders was researched in ASD [16,17][16][17].2.2. Development of Rapid Eye Movement (REM) and Non-REM Sleep
There are two primary types of sleep: (1) active sleep or rapid eye movement (REM) sleep (dynamic REM sleep: eyes closed, eye movements, frequent movements of limbs and face, irregular breathing pattern) and (2) quiet sleep or non-REM sleep (static non-REM sleep: eyes closed without movements, little body movement, and regular breathing). Eye movements occur frequently at 24–26 weeks, with a period of no eye movement at 32 weeks, and regular breathing occurs at 32 weeks. Active sleep is primordial REM sleep, and is seen as a primitive, disorganized state during early embryonic development. It appears after 36 weeks of gestation and increases by three months [5]. In other words, the development of REM and non-REM sleep is the development of control mechanisms for excitation and inhibition and can be said to be the development of control systems for the brainstem and cortex. Thus, the development of REM and non-REM sleep is meaningful and reflects changes in brain maturation [18]. At one month of age, REM and non-REM sleep are frequently repeated, but by nine months of age, the sleep architecture approaches that of an adult. The twitching of the body during sleep may be due to muscle twitching associated with REM sleep. The development of REM and non-REM sleep is also linked to changes in the sleep–wake rhythm during infancy. The sleep–wake rhythm suggests alternating mechanisms of inhibition and excitation of the central nervous system during early development, which are closely related to the development of complex neural networks and neurotransmitters. Based on the above findings, we suggest that a well-regulated sleep rhythm is a well-developed control system for neurodevelopment in a well-developed child.3. The Importance of Sleep Hygiene for Children
Before evaluating a sleep disorder in a child, it is of paramount importance to evaluate, as a prerequisite, whether ‘the parent or guardian has a stable sleep rhythm’ or whether ‘the parent or guardian pays attention to the adequate environment in which the child sleeps well at night’. The sleep rhythm of the child changes with that of his or her guardian [48][19]. A child with inappropriate sleep hygiene cannot be diagnosed as a ‘child who cannot sleep at night’ or as having a sleep disorder. It goes without saying that ‘sleeplessness’ is a ‘sleep disorder’, despite the efforts of the parents to put the child to sleep. Many studies suggest that the mother’s life influences the infant’s sleep rhythm.
Shinkoda [49][20] proved that the sleep time at four months of age was later than that at one and a half and three years of age, and that this was due to the mother’s sleep behaviour. Adachi [50][21] also found that the sleep rhythm at four months affects the rhythm establishment of the later sleep–wake rhythm and can be improved through intervention. Neurologists and paediatricians help prevent sleep deprivation by carers.
Figure 1 shows the sleep record of a nine-month-old boy. He visited the hospital with complaints of moodiness and developmental delay, chiefly. His parents were instructed to decrease feedings during the night, to wake him up in the morning (he used to wake up at 9 a.m.), and to communicate with him as much as possible at baby salons during the day. After two weeks, improvements in sleep rhythm, mood swings, and developmental delays were observed.
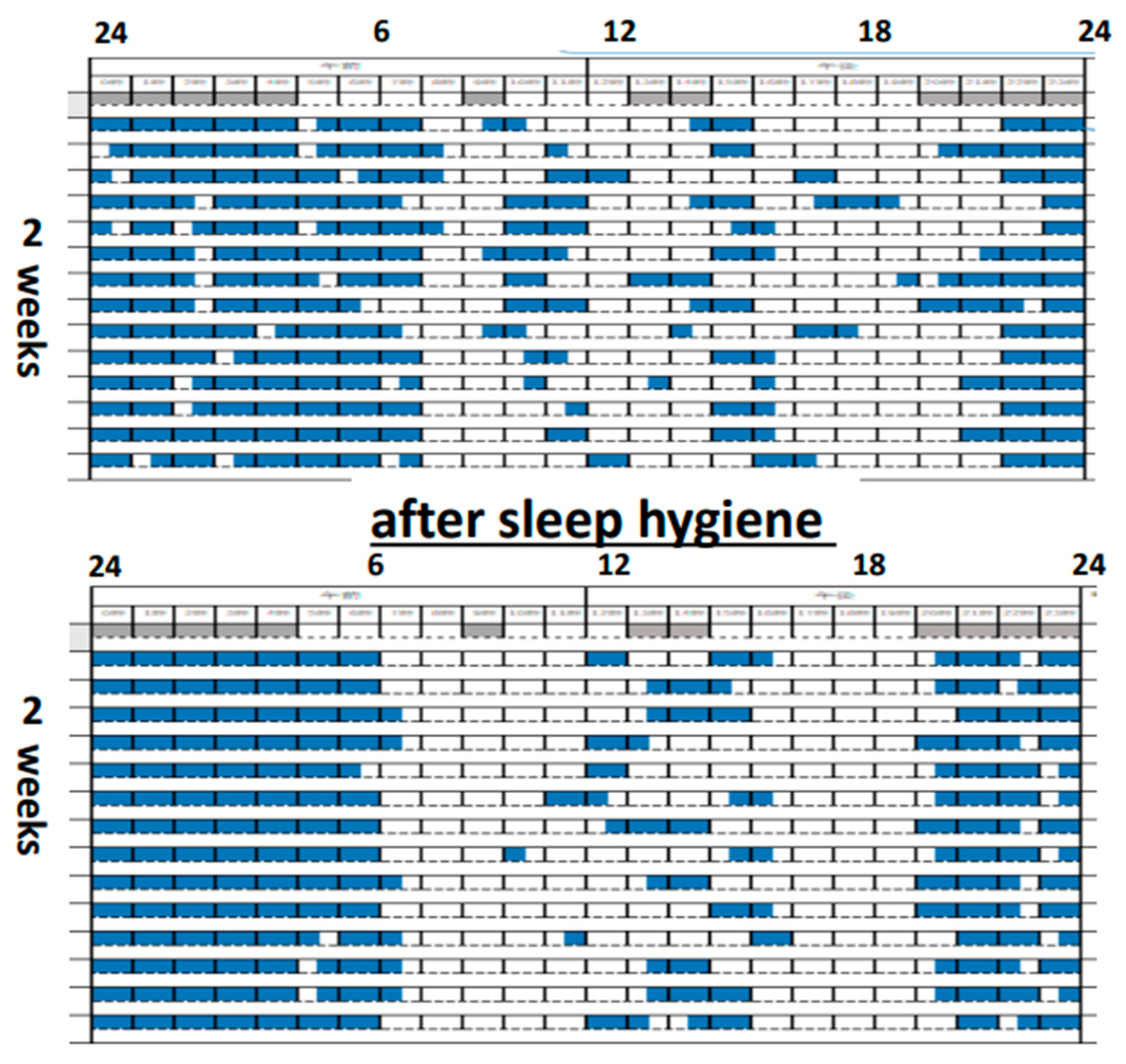
Figure 1. A 9-month-old boy improved not only his sleep rhythm, but his mood swings and developmental delays after two weeks of sleep hygiene education.
The disruption of sleep rhythms in early childhood can be a problem of inappropriate sleep hygiene and late sleep involving carers. Sleep problems in early childhood immediately affect children’s development. Suzuki [51][22] reported that irregular sleep rhythms in one-year-olds significantly correlated with poor finger-pointing, apathy, and emotional and behavioural problems. They also reported interesting findings on sleep and drawing triangles in five-year-old children. Late sleep time and the inability to draw triangles had a significantly higher odds ratio. The disintegration of higher cognitive function and sleep deprivation were also assessed. A five-year-old girl was presented to the hospital with the chief complaint of auditory hypersensitivity. Her bedtime was 11 p.m.; therefore, she was instructed to go to bed at 9 p.m. and her auditory hypersensitivity completely improved. This is the first case in which auditory sensitivity was improved by good sleep, and reminded people the importance of sleep in children.
It is no exaggeration to say that smartphones, the Internet, and the media have had the worst impact on children’s sleep in recent times. Children with ADHD are highly impulsive and game-dependent, whereas those with ASD are unable to leave the media due to interpersonal problems, such as developing social skills in the online world [52][23]. Night-time media use and light decrease melatonin levels, which further fails to improve sleep rhythms and contributes to abnormal sleep–wake rhythms. Media literacy is a major issue for children’s physical and mental development.
References
- Rosenwasser, A.M.; Turek, F.W. Neurobiology of Circadian Rhythm Regulation. Sleep Med. Clin. 2022, 17, 141–150.
- Panda, S. Circadian physiology of metabolism. Science 2016, 354, 1008–1015.
- Grandner, M.A. Sleep, Health, and Society. Sleep Med. Clin. 2022, 17, 117–139.
- Segawa, M.; Nomura, Y.; Hara, Y.; Hara, Y.; Shimajiri, T.; Miyagawa, F.; Hachimori, K.; Shinomiya, N. Pathogenesis of early in-fantile autism. Brain Dev. 1979, 3, 219.
- Clemente, C.D.; Purpura, D.P.; Mayer, F.E. Sleep and the Maturing Nervous System; Academic Press: New York, NY, USA; London, UK, 1972.
- Edward, F.; Schott, P.; Hobson, J.A. The Neurobiology of Sleep: Genetics, cellular physiology and subcortical networks. Nature Rev. Neurosci. 2020, 3, 591–605.
- Parmelee, A.H.; Wenner, W.H.; Schulz, H.R. Infant sleep patterns: From birth to 16 weeks of age. J. Pediatr. 1964, 65, 576–582.
- Matsuoka, M.; Segawa, M.; Higurashi, M. The Development of Sleep and Wakefulness Cycle in Early Infancy and Its Relationship to Feeding Habit. Tohoku J. Exp. Med. 1991, 165, 147–154.
- Prendergast, B.J.; Zucker, I. Ultradian rhythms in mammalian physiology and behavior. Curr. Opin. Neurobiol. 2016, 40, 150–154.
- Segawa, M.; Nomura, Y.; Katoh, J.; Uratake, K. Abnormal sleep-wakeful cycle in children. In New Trends in Pediatric Neurology; Fejeman, N., Chamoles, N.A., Eds.; Elseviere Science Publishers: Amsterdam, The Netherlands, 1993; pp. 207–212.
- Lopp, S.; Navidi, W.; Achermann, P.; LeBourgeois, M.; Behn, C.D. Developmental Changes in Ultradian Sleep Cycles across Early Childhood. J. Biol. Rhythm. 2017, 32, 64–74.
- So, K.; Adamson, T.M.; Horne, R.S.C. The use of actigraphy for assessment of the development of sleep/wake patterns in infants during the first 12 months of life. J. Sleep Res. 2007, 16, 181–187.
- Hayama, J.; Adachi, Y.; Nishino, N.; Oshiryouji, F. Sleep of 4-month-old infants: Bedtime, night waking and sleep problems. Nihon Koshu Eisei Zasshi 2007, 54, 440–446.
- Fukumizu, M.; Kaga, M.; Kohyama, J.; Hayes, M.J. Sleep-Related Nighttime Crying (Yonaki) in Japan: A Community-Based Study. Pediatrics 2005, 115 (Suppl. S1), 217–224.
- Hoppenbrouwers, T.; Hodgman, J.; Arakawa, K.; Geidel, S.A.; Sterman, M.B. Sleep and Waking States in Infancy: Normative Studies. Sleep 1988, 11, 387–401.
- Basile, C.; Gigliotti, F.; Cesario, S.; Bruni, O. The relation between sleep and neurocognitive development in infancy and early childhood: A neuroscience perspective. Adv. Child Dev. Behav. 2021, 60, 9–27.
- Segawa, M.; Katoh, M.; Nomura, Y. Early modulation of sleep parameters and its importance in later behavior. Brain Dysfunct. 1992, 5, 211–223.
- Knoop, M.S.; de Groot, E.R.; Dudink, J. Current ideas about the roles of rapid eye movement and non–rapid eye movement sleep in brain development. Acta Paediatr. 2021, 110, 36–44.
- Zhang, J.; Li, A.M.; Fok, T.F.; Wing, Y.K. Roles of Parental Sleep/Wake Patterns, Socioeconomic Status, and Daytime Activities in the Sleep/Wake Patterns of Children. J. Pediatr. 2010, 156, 606–612.
- Shinkoda, H.; Matsumoto, K.; Asami, E.; Suetsugu, Y.; Kato, N.; Uchimura, N.; Chishaki, A.; Kaku, T.; Kohyama, J.; Nanbu, Y.; et al. Analysis of late bedtime and influencing factors for it with respect to infants’ development age and sleep behavior of parents and children. Fukuoka Igaku Zasshi 2008, 99, 246–261.
- Adachi, Y.; Sato, C.; Nishino, N.; Ohryoji, F.; Hayama, J.; Yamagami, T. A Brief Parental Education for Shaping Sleep Habits in 4-Month-Old Infants. Clin. Med. Res. 2009, 7, 85–92.
- Suzuki, M.; Nakamura, T.; Kohyama, J.; Nomura, Y.; Segawa, M. Children’s ability to copy triangular figures is afeced by their sleep—wakefulness rhythms. Sleep Biol. Rhythm 2005, 3, 86–91.
- So, R.; Makino, K.; Fujiwara, M.; Hirota, T.; Ohcho, K.; Ikeda, S.; Tsubouchi, S.; Inagaki, M. The Prevalence of Internet Addiction Among a Japanese Adolescent Psychiatric Clinic Sample with Autism Spectrum Disorder and/or Attention-Deficit Hyperactivity Disorder: A Cross-Sectional Study. J. Autism Dev. Disord. 2017, 47, 2217–2224.
More
 Encyclopedia
Encyclopedia
