Oxidative stress (OxS) is a physiologically significant alteration in redox status resulting from the overproduction of reactive species and or the reduction in antioxidant defenses. Oxidative stress (OxS) has emerged as a likely initiating factor in T2D. Antioxidant supplements may act to slow or prevent T2D by multiple mechanisms, i.e., (1) reducing mitochondrial oxidative stress, (2) preventing the damaging effects of lipid peroxidation, and (3) acting as essential cofactors for antioxidant enzymes.
- antioxidants
- type 2 diabetes
- vitamin E
- vitamin C
- selenium
- manganese
- beta-carotene
- oxidative stress
1. Introduction
The worldwide prevalence of diabetes mellitus (DM) over the last three decades has at least tripled, making this disease a critical public health and economic issue for most nations (1, 2)[1][2]. About 90–95% of those with DM have type 2 DM (T2D) which is rapidly increasing in children, adolescents, and young adults along with an increasing rate of prediabetes, a major risk factor for T2D (3)[3]. About one in three USA adults have prediabetes, which is undiagnosed in eight out of ten people (4),(5)[4][5]. The total USA cost of DM in 2017 was USD 327 billion with each diagnosed individual incurring about USD 16,000 in annual medical expenses (4)[4]. Minimizing physiological factors that induce damaging OxS and maximizing natural antioxidant products (i.e., the OptRedox strategy) may provide a means of preventing or slowing T2D progression. Both adults and the pediatric population could potentially benefit from this OptRedox strategy.
2. The Role of Oxidative Stress and T2D Pathogenesis
As shown in Figure 1, there are four stages to T2D progression, i.e., insulin resistance, prediabetes, T2D, and T2D with vascular damage (8, 9)[6][7][8][9]. Fasting blood glucose levels (and/or HbA1c) levels are the main criteria for distinguishing these stages. T2D pathogenesis is multifactorial with very complex alterations in carbohydrate, lipid, and protein metabolism (10)[10].

Figure 1. The four stages of type 2 diabetes (T2D) progression and oxidative stress. The roles of reactive oxygen species (ROS) and advanced glycation end products (AGEs) in T2D progression are explained in the text below.
3. Insulin Resistance in Skeletal Muscle Is Considered the Initiating Defect Leading to T2D
Damaging OxS plays a central role in both initiating and accelerating the progression of T2D (7, 11, 12)[7][11][12]. Insulin resistance in skeletal muscle is considered the initiating, or primary, defect leading to T2D (13)[13]. GLUT4 is the primary glucose transporter for skeletal muscle. Under normal circumstances, insulin binding to the insulin receptor on skeletal muscle cells activates AKT (serine/threonine-specific protein kinases) phosphorylation, eventually resulting in the translocation of GLUT4 to the plasma membrane, thereby promoting glucose transport from plasma into skeletal muscle cells. Skeletal muscle insulin resistance occurs when the normal amount of insulin is inadequate for promoting the expected uptake of glucose. Over time, insulin resistance may result in prediabetes with an increased level of blood glucose. Skeletal muscle accounts for about 80% of insulin-stimulated glucose uptake (13)[13]. Decreased insulin-stimulated translocation of GLUT4 to the skeletal muscle surface, and/or decreased expression of GLUT4, are well-accepted causes of insulin resistance (14-16)[14][15][16].
4. Skeletal Muscle Mitochondrial Hydrogen Peroxide (H
2
O
2
) Emission Results in Insulin Resistance
The pioneering work of Anderson et al. (17)[17] in normal rodents and humans shows that excess dietary calories promote skeletal muscle mitochondrial hydrogen peroxide (H2O2) emission resulting in transient insulin resistance. While excess dietary carbohydrates and fat both promote this effect, it is markedly more pronounced with a high-fat diet. In obese but otherwise healthy human subjects, skeletal muscle mitochondrial H2O2 emission was twice the level observed in lean human subjects (17)[17]. Mechanistically, a high-fat diet prevented the AKT-mediated translocation of GLUT4 to the skeletal muscle surface as detailed above (other mechanisms could also be involved) (17)[17]. Increased mitochondrial H2O2 emission was accompanied by a reduction in the skeletal muscle ratio of reduced glutathione (GSH) to oxidized glutathione (GSSG) which would be expected by the glutathione peroxidase (GPX) reduction of H2O2 to H2O (see Figure 2).

Figure 2. Glutathione peroxidase decomposition of hydrogen peroxide. Mitochondrial electrons from the respiratory chain are donated to oxygen forming the superoxide radical (O2*−.). Superoxide dismutase (SOD) generates hydrogen peroxide (H2O2) from O2*−. In the mitochondrial matrix, the only isoform of SOD present is manganese SOD (see text in Section 12). H2O2 (or lipid hydroperoxide) is reduced to H2O (or lipid alcohols) by glutathione peroxidase (GPX) utilizing reduced glutathione (GSH) and generating oxidized glutathione (GSSG). GSSG is recycled back to GSH by glutathione reductase (GR) with the consumption of NADPH. Mitochondrial GPX is a selenium (Se)-requiring enzyme.
5. Avoiding High-Fat, High-Calorie Meals Could Be an Effective OptRedox Strategy
The Anderson et al. research strongly suggests that avoiding high-fat, high-calorie meals (and the attendant OxS) could be an effective OptRedox strategy for inhibiting early T2D initiation (17)[17]. Encouragingly, there is evidence showing that a low-calorie diet combined with long-term weight-loss support has the potential to reverse T2D in adults (19, 20)[18][19][20].
6. Hyperglycemia, Oxidative Stress, and T2D Progression
In susceptible individuals, skeletal muscle insulin resistance can be a contributing factor to increased postprandial glycemia (PPG) (21, 22)[21][22]. Postprandial glucose can eventually exceed 140 mg/dL (2 h after a carbohydrate-containing meal) and become postprandial hyperglycemia (PPH), which is one of the earliest abnormalities associated with T2D (21)[21].
High levels of PPG are problematic for multiple reasons. PPG, 2 h after lunch, is a better predictor of cardiovascular events and all-cause mortality in T2D than fasting blood glucose levels (23, 24)[23][24]. In an excellent and extensive review, Sottero (22)[22] et al. concluded that chronic postprandial OxS resulting from PPH is a key factor driving T2D progression. The mechanisms connecting hyperglycemia and OxS are detailed below.
7. Hyperglycemia, AGE Formation, the Polyol Pathway, and Oxidative Stress
Glucose can covalently react with lysine, arginine, and N-terminal residues on proteins to form glycation adducts which can further react to form advanced glycation end products (AGEs) (25)[25]. Fasting hyperglycemia or PPH increases AGE formation in plasma proteins as well as proteins on the outer plasma-membrane surface of most cells (26-28)[26][27][28]. Covalent modification of proteins by glucose can alter their structure and, potentially, their functions. For cells relying on insulin-independent GLUT transporters (e.g., GLUT1) intracellular glucose concentration will increase in response to hyperglycemia, thereby promoting AGE-modification of cytosolic proteins. Both red blood cells and vascular endothelial cells rely on GLUT1, and glucose in these cell types will equilibrate with plasma glucose. Under PPH or fasting hyperglycemia, cells primarily relying on GLUT1 will utilize the polyol pathway and thereby lower intracellular glucose by converting it to fructose. The polyol pathway consumes NADPH which is needed to keep GSH in the reduced form (see Figure 2) required by the GPX system to detoxify H2O2 (and lipid hydroperoxides). Under hyperglycemic conditions, it has been estimated that about 30% of blood glucose goes through the polyol pathway (29)[29].
As indicated in Figure 3, mitochondrial OxS induces insulin resistance leading to increased plasma glucose, increased plasma AGEs, and increased polyol-induced NADPH consumption, all of which contribute to systemic OxS and inflammation. Moreover, both in vitro and in vivo evidence indicate that plasma-protein AGEs can induce insulin resistance by repression of GLUT4 expression in skeletal muscle (30)[30]. This AGE-induced insulin resistance is an example of an amplifying OxS feedback loop, i.e., plasma AGEs further increase insulin resistance by amplifying glycemia and OxS. OxS can also contribute to beta-cell dysfunction and reduced glucose-induced insulin secretion, thereby further increasing the risk of hyperglycemia and T2D progression (31)[31]. Both AGE formation and systemic OxS give rise to an increased risk of both macrovascular and microvascular damage (32, 33)[32][33].
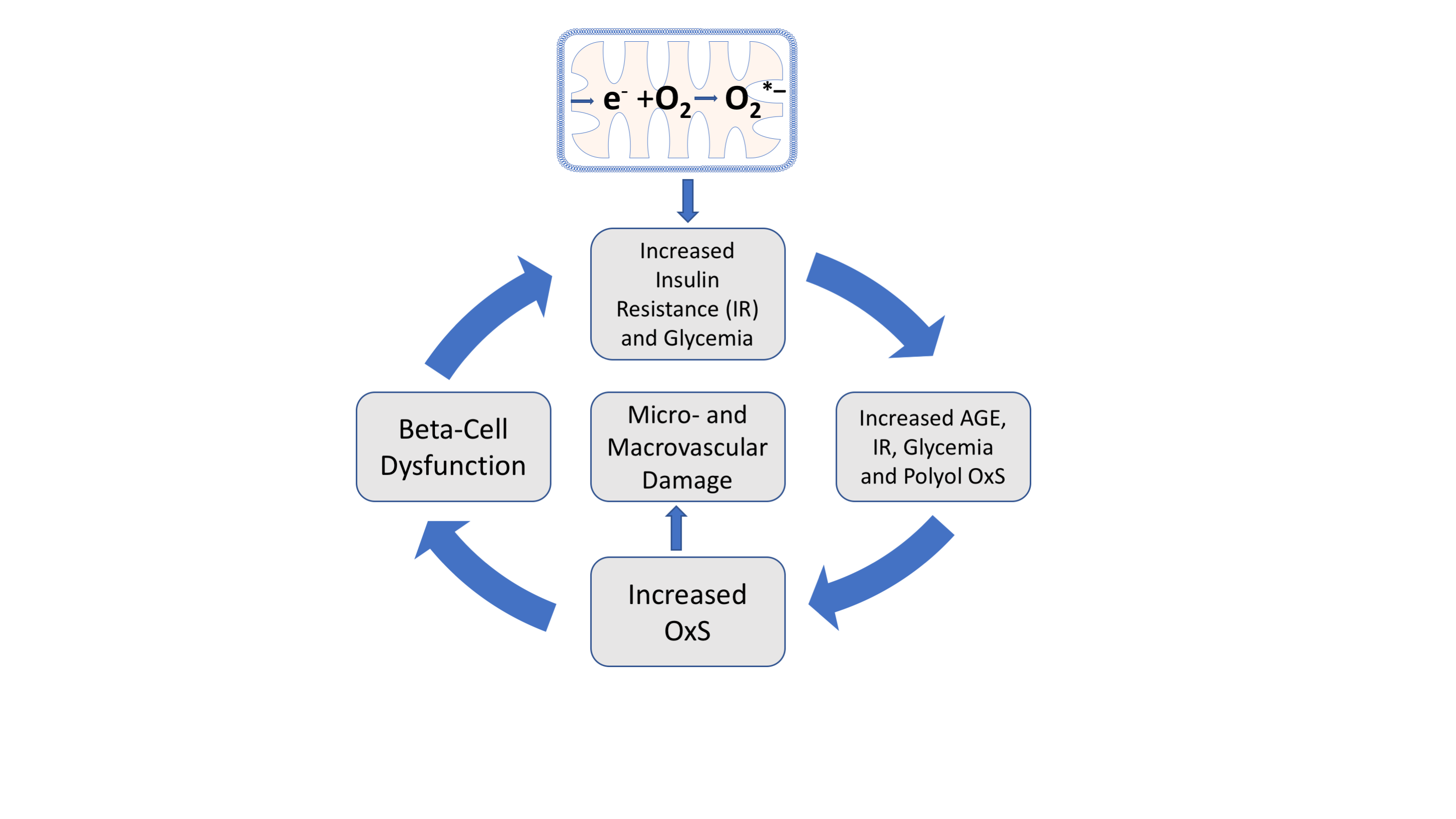
Figure 3. Amplifying oxidative stress (OxS) feedback loops and T2D initiation and progression. Mitochondrial generation of O2*− (top) and the subsequent production of H2O2 (see Figure 2) are proposed initiating factors for T2D and give rise to transient insulin resistance (IR) and increased glycemia. Chronic increases in glycemia promote increased AGE formation which can also promote hyperglycemia and polyol-induced OxS.
8. The OptRedox Strategy for Preventing or Slowing the Progression of T2D
Most publications on the roles of natural antioxidants in T2D progression tend to focus on individual antioxidant molecules such as vitamin E and their roles in blocking OxS. There are, however, benefits that arise from reframing this focus to also include OptRedox strategies for preventing or slowing the progression of T2D. An OptRedox approach is more nuanced by also embracing dynamic physiological processes such as glycemic control and physical activity. As outlined in Figure 3, processes that increase insulin resistance and glycemia can also promote damaging OxS and T2D progression. In contrast, processes that decrease insulin resistance and glycemia can be considered as promoting an OptRedox strategy. Both glycemic control and exercise can be viewed as natural processes promoting an OptRedox status (11)[11]. Exercise, despite causing a transient oxidative OxS, subsequently induces skeletal muscle antioxidant enzymes that are beneficial for preventing T2D progression (34, 35)[34][35].
8.1. Glycemic Control as a Natural OptRedox Process
In those with T2D, glycemic control is clinically defined as maintaining an HbA1C level of less than 7.0%, or 6.5% for more strict control (36)[36]. Both fasting and PPG impact HbA1C levels. Woerle et al. have found that lowering PPG is essential for optimizing glycemic control. In contrast to good glycemic control, poor glycemic control in subjects with T2D or prediabetes results in decreased plasma total antioxidant capacity and increased lipid peroxidation (a marker of OxS) (37)[37]. Physical activity/exercise is well a recognized critical factor for promoting glycemic control in individuals with T2D or prediabetes (38, 39)[38][39].
8.2. Physical Activity/Exercise as an OptRedox Lifestyle Factor
As emphasized by the American Diabetes Association (ADA), physical activity in T2D and prediabetes improves glycemic control while also reducing cardiovascular risk and promoting weight loss (38)[38]. Moreover, the ADA suggests that “regular exercise may prevent or delay T2D development”. Light exercise provides an excellent example of an OptRedox lifestyle factor with an untapped potential to reduce OxS and slow T2D progression and, could potentially be cost-effectively implemented in a school setting (40)[40].
8.3. Light-Intensity Walking as an OptRedox Lifestyle Factor That Reduces Postprandial Glycemia (PPG)
A recent meta-analysis in predominantly adults with overweight or obesity showed that as little as two to five minutes of light-intensity walking significantly reduced PPG levels compared to prolonged sitting (41)[41]. This meta-analysis also found that the light-exercise-induced lowering of PPG was more effective in overweight individuals compared to individuals with obesity, suggesting that obesity imposes additional metabolic dysfunction (41, 42)[41][42]. Given the acknowledged importance of early intervention, it is critically important that this research be repeated in a pediatric population, perhaps, in a school setting. The potential near-future availability of real-time noninvasive blood glucose sensors on consumer smartwatches will rapidly accelerate research efforts focused on PPG as well as fasting hyperglycemia (43, 44)[43][44]. Twenty-four-hour glycemic profiles have shown a significant reduction in PPG in T2D subjects performing 15 min of strolling during each postprandial period compared to sedentary T2D subjects (39, 45)[39][45].
Short-duration light-intensity walking can lower PPG simply by promoting skeletal muscle consumption of glucose. Exercise can, however, also increase skeletal muscle uptake of glucose by promoting GLUT4 translocation to the plasma membrane as well as GLUT4 expression (46)[46]. Both low- and high-intensity exercise can equally and immediately induce GLUT4 expression in human skeletal muscle (47, 48)[47][48]. The signaling pathway for exercise-induced translocation of GLUT4 is distinct from that of insulin (see above) and likely involves AMP-activated protein kinase (AMPK) and increased sarcoplasmic calcium (46)[46].
9. Exercise, Reactive Oxygen Species (ROS), and OptRedox Status
As reviewed by Kawamura (49)[49] there is a “consensus that exercise increases the production of free radicals”. It is recognized, however, that exercise duration and intensity are key determinants of measurable OxS (49, 50)[49][50]. Moreover, transient exercise-induced OxS can evoke both beneficial and adverse physiological processes depending on the intensity/duration of the OxS and body conditioning (34)[34]. High levels of exercise-induced OxS can result in adverse damage to skeletal muscle, particularly in untrained individuals (51)[51]. It has long been recognized that physiological levels of ROS play essential roles in cell signaling pathways (52, 53)[52][53]. This raises the possibility that high levels of exogenous chemical antioxidant supplements could interfere with cell signaling pathways (see below) (54)[54].
9.1. Exercise-Induced ROS Production Has a Biphasic Impact on Skeletal Muscle Force Production
Powers et al. (51) have reviewed the evidence showing that exercise-induced ROS production has a biphasic impact on skeletal muscle force production, i.e., low levels of ROS production increase contractile force, but high ROS levels decrease force production. There is, therefore, an optimal level of exercise-induced ROS production (and redox status) required for maximal skeletal muscle contraction force. The molecular mechanism(s) for this biphasic effect is/are not fully understood, but this illustrates the need to consider complex physiological processes in determining an OptRedox status (51, 55)[51][55].
The relationship between exercise intensity and ROS production has been and continues to be, the subject of intensive research (49, 56)[49][56]. During low and moderate exercise, the lactate released from muscle tissue into blood can be absorbed without build-up. During vigorous exercise, however, the released lactate is released faster than it can be absorbed, i.e., this is termed the lactate threshold. Quindry, et al. (50)[50] have shown that ROS production in humans primarily results from exercise intensities above the lactate threshold. Subsequent research has shown that exercise duration can also impact the rate of ROS production in humans (49)[49]. Although beyond the scope of this review, the overall consensus is that the ROS produced during vigorous exercise can have both positive and negative effects. In addition to the potentially positive effect ROS can have on skeletal muscle function, ROS can also increase the expression of some enzymatic antioxidants. As will be discussed below, this effect may be blunted by natural exogenous chemical antioxidants such as vitamin E.
9.2. Exercise-Induced Oxidative Stress and Induction of Enzymatic Antioxidants
As mentioned above, exercise has long been associated with an increased activity level of some endogenous antioxidant enzyme, e.g., skeletal muscle GPX (57)[57]. It has also been hypothesized that the ROS generated during exercise could be essential for this induction of antioxidant enzymes by modulating signal transduction pathways (35, 57)[35][57]. If this hypothesis is correct, it raises the concern that antioxidant supplements could interfere with this induction. The research of Ristow et al. (35)[35] shows that supplementation for four weeks with ascorbate (1000 mg/day) plus vitamin E (400 IU/day) blocked the exercise-induced expression of GPX1 in skeletal muscle biopsies from healthy young men. These investigators also found that four weeks of exercise increased insulin sensitivity, but this effect was blocked by daily supplementation with ascorbate plus vitamin E. The form of vitamin E used in these experiments was RRR-alpha-tocopherol (more on this below). Ristow et al. concluded that exercise-induced ROS are essential for promoting insulin sensitivity and the induction of GPX1 (35)[35]. Although discussed as being relevant to T2D, the subjects in this study were healthy adult males. In the context of T2D, the lifelong implementation of regular exercise and physical activity, in general, is overwhelmingly viewed as an essential factor for preventing or slowing T2D progression (58)[58].
10. Sleep and Psychological Stress as Lifestyle Factors Affecting T2D and Oxidative Stress
In addition to exercise, dealing with other lifestyle factors that promote or cause sleep disorders/disturbances and/or psychological stress may also play important roles in T2D prevention and therapy (59, 60)[59][60]. Moreover, both sleep disorders (61,[61][62] 62) and psychological stress (63)[63] have been linked to increased OxS. T2D is associated with a higher incidence of sleep disorders and emerging evidence supports a positive role of sleep quality in T2D glycemic control (59)[59]. As detailed in Sections 5 and 6, and Figure 3, poor glycemic control contributes to OxS. In an animal model, Everson et al. found that sleep deprivation was associated with a decreased level of liver catalase activity (an antioxidant enzyme) and GSH content (see Figure 2). Moreover, these authors found that sleep recovery could restore both liver catalase and GSH content to normal levels. The relationship between OxS and sleep disorders is attracting increased research interest (64)[64]. Future research may help define the molecular mechanisms connecting sleep, antioxidants, and T2D. Due to preexisting OxS, individuals with T2D may have an enhance adverse susceptibility to any additional OxS driven by sleep disturbances and/or stress.
11. The Distinct Forms of Vitamin E and Their Effects on T2D Progression
Natural chemical antioxidants that prevent or inhibit skeletal muscle mitochondrial oxidative stress would be excellent candidates for potentially slowing or blocking the progression of insulin resistance. Vitamin E is considered the primary lipid-soluble antioxidant and is present in all biomembranes including those of mitochondria where vitamin E levels can be increased by dietary supplementation (65)[65].
11.1. Natural Vitamin E and the Importance of Stereochemistry
According to the International Union of Pure and Applied Chemistry the term “vitamin E” refers to “all tocol and tocotrienol derivatives exhibiting qualitatively the biological activity of α-tocopherol”. Natural vitamin E from dietary sources consists of (1) four tocopherol monophenol vitamers (TOH), i.e., alpha-TOH, beta-TOH, gamma-TOH, and delta-TOH) and; (2) four tocotrienol (T3) monophenol vitamers, i.e., alpha-T3OH, beta-T3OH, gamma-T3OH, and delta-T3OH. T3s are forms of vitamin E in which the hydrophobic “tails” have three trans double bonds (66)[66].
The stereochemistry of natural vitamin E vitamers is very specific. For example, natural alpha-tocopherol has three asymmetric carbons, and each has the R stereochemical designation, i.e., 2R,4′R,8′R-alpha-tocopherol (or RRR-alpha-TOH). In contrast, synthetic alpha-tocopherol has both R and S configurations at each of the three asymmetric carbons and is, therefore, an equimolar mixture of eight compounds with only one eighth being the natural RRR-alpha-TOH: the other seven forms being xenobiotics with mostly unknown physiochemical properties. The synthetic form of alpha-TOH is most often termed all-racemic-alpha-tocopherol (or all-rac-alpha-TOH). Since vitamin E compounds have signal-transduction properties that are independent of their antioxidant oxidant abilities, it is important to detail the form used in any experiment/trial (67, 68)[67][68]. Unfortunately, this is often not the case, which makes reproducibility difficult, obscures potential physiological effects unique to specific vitamin E vitamers, and confounds meta-analyses which often lump all forms of vitamin E together.
11.2. Supplementation with “Vitamin E” May Be a Valuable Strategy for Controlling Diabetes Complications
A meta-analysis of the effects of antioxidant vitamins on T2D concluded that supplementation with vitamin E “may be a valuable strategy for controlling diabetes complications” (69)[69]. In this meta-analysis, the different forms of vitamin E were lumped together making it difficult to determine if positive or negative effects were unique to a form of vitamin E. In addition, the primary papers sometimes fail to distinguish all-rac-alpha-TOH from RRR-alpha-TOH. Nevertheless, all vitamin E vitamers are free radical quenchers and inhibit lipid peroxidation. It is possible, therefore, that the antioxidant properties shared by all members of the vitamin E family contribute to their positive effects on controlling T2D complications. Interestingly, increased lipid peroxidation is associated with poor glycemic control in T2D patients (37)[37].
11.3. All-Racemic-Alpha-Tocopherol (All-Rac-Alpha-TOH) and Rice Bran Tocopherol Concentrate Inhibit Skeletal Muscle Generation of Hydrogen Peroxide
Given the central importance of mitochondrial oxidative stress in T2D (see Figure 3), vitamin E has been advanced as an antioxidant with great therapeutic potential for T2D treatment. As detailed above, skeletal mitochondrial hydrogen peroxide emission may be an initiating event for the development of insulin resistance. In a rat model, Chow et al. have quite remarkedly demonstrated that dietary supplementation with either all-rac-alpha-TOH or a rice bran tocopherol concentrate (8.6% RRR-alpha-TOH, 5.5% RRR-beta-TOH, and 15.4% gamma-T3OH) markedly decreases skeletal muscle hydrogen peroxide generation in a dose-dependent manner (70)[70]. The mechanism for this important effect is not well understood and has not been studied in human skeletal muscle, but this implies that early supplementation with vitamin E could slow the progression of T2D. Future mechanistic research on the role of vitamin E on mitochondrial hydrogen peroxide emission is a high priority.
11.4. Vitamin E and/or Ascorbate Supplementation Improves Glycemic Control in T2D
In contrast to the work of Ristow et al. (35)[35] (see Section 9.2) in n which the subjects were adult healthy males, El-Aal et al. (71)[71] conducted a clinical trial looking at the effects of vitamin E and/or ascorbate on adult T2D males who were all under metformin treatment. The results clearly show beneficial effects on glycemic control in those supplementing (for 90 days) with vitamin E alone (400 mg twice daily), ascorbate (500 mg twice daily) alone, or the combination of both. Unfortunately, it is not clear if RRR-alpha-TOH or all-rac-alpha-TOH was the form of vitamin E used in this trial. Nevertheless, this study strongly suggests that future studies should look at the potential beneficial effects of vitamin E supplementation on pediatric subjects with prediabetes or with T2D. Subjects with T2D or prediabetes with antioxidant deficiencies due to enhanced OxS may respond differently to antioxidant supplementation (or exercise) than healthy subjects with adequate antioxidant levels.
11.5. The Tocotrienol-Rich Fraction (TRF) from Palm Oil May Be Beneficial in Both Prediabetes and T2D and in Preventing Early Diabetic Retinopathy
Evidence from a randomized double-blind placebo-controlled clinical trial (the Vafa study) in T2D subjects with poor glycemic control shows that the tocotrienol-rich fraction (TRF) from palm oil (200 mg daily) for eight weeks lowered fasting blood glucose levels by 15% and improved indices of OxS (72)[72]. An earlier study (the Baliarsingh study) in adult T2D subjects did not show any benefit of tocotrienols (60 days, 3 mg/kg body weight, twice daily) on fasting blood glucose, but these subjects had well-medication-controlled blood glucose levels at the start of the trial (73)[73]. This earlier study did, however, show a marked decrease in atherogenic low-density lipoprotein cholesterol levels in the subjects taking the tocotrienol supplement. In both the Baliarsingh et al. study and the Vafa et al. study, the palm oil TRF was predominantly alpha-T3OH, beta-T3OH, gamma-T3OH, and RRR-alpha-TOH with only a small content (about 4–8%) of delta-T3OH. The low content of delta-T3OH in the TRF is noteworthy since delta-T3OH may be uniquely important in preventing T2D progression, as detailed below.
A recent study by Ho, et al. (74)[74] showed that TRF (200 mg twice daily for 12 months) was effective in preventing early diabetic retinopathy compared to a placebo. Diabetic retinopathy is a very common microvascular complication of T2D and makes a major contribution to blindness and vision loss in adults (74)[74].
11.6. Delta-Tocotrienol Shows Promise in Treating Prediabetes
Treatment options for prediabetes are limited, especially in the pediatric population (75)[75]. Encouragingly, a recent randomized controlled pilot study looked at the effects of T3 purified from annatto seeds: this preparation was primarily delta-T3OH (90%) and 10% gamma-T3OH (76)[76]. The prediabetic adult study population was not being treated with any medications for glucose control or taking any dietary supplements. After 12 weeks of 300 mg/day of T3s, there were significant improvements in glycemic control compared to the controls taking a placebo (76)[76]. T3s are thought to improve glycemic control by upregulating the skeletal muscle expression of GLUT4, insulin receptor substrate 1, AKT signaling, and by activation of peroxisome proliferator-activated receptor-gamma (PPAR-gamma) (76, 77)[76][77].
12. Vitamin C (L-Ascorbate or AA) and Its Role in T2D Progression and Management
Vitamin C is a water-soluble antioxidant present in plasma and tissues. As detailed below, vitamin C status and vitamin C supplementation play potential roles in T2D progression and management (78-85)[78][79][80][81][82][83][84][85]. The molecular mechanisms for the protective effects of vitamin C on T2D are not fully understood but inhibition of mitochondrial OxS is a probable candidate (see Figure 4). As discussed further below, Vitamin C may also reduce the chronic low-grade inflammation associated with promoting T2D progression (86)[86].

Figure 4. Vitamin C protects mitochondria from reactive oxygen species (ROS). Oxidized vitamin C (DHA, as shown in Figure 5) is transported from the cytoplasm into the mitochondrial matrix by GLUT1, where it is reduced to ascorbate (AA, as shown in Figure 5) where it blocks mitochondrial OxS by reducing the levels of ROS such as superoxide, hydrogen peroxide, and hydroxyl radicals. Reduced mitochondrial OxS may be an important mechanism for combating insulin resistance.
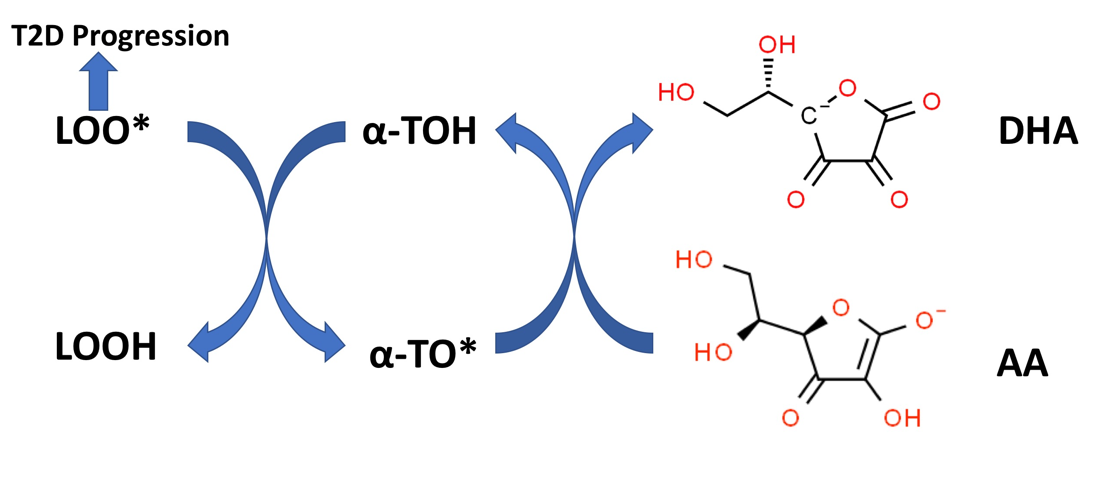
Figure 5. Vitamin E recycling by Vitamin C. Alpha-tocopherol (alpha-TOH) quenches lipid peroxidation by converting lipid peroxyl radicals (LOO*) to lipid hydroperoxides (LOOH) with the formation of alpha-tocopheroxyl radicals (alpha-TO*). The reduced form of vitamin C (AA), can recycle alpha-TO* back to alpha-TOH with the formation of oxidized vitamin C (DHA). Increased lipid peroxidation is associated with T2D progression (see text).
12.1. Vitamin C Protects Mitochondria from Oxidative Stress
Figure 4 illustrates a possible mechanism whereby L-ascorbate (AA) supplementation could promote glycemic control. At pH 7.4, vitamin C is primarily present as the mono-anion as indicated in FigureFigure 5 5 (87)[87]. Outstanding in vitro work by Sagun et al. (88)[88] has shown that DHA enters mitochondria, via the facilitative D-glucose transporter GLUT1, where it is reduced to AA and protects mitochondria from OxS damage. In oxidatively stressed purified mitochondria, AA was found to reduce the levels of H2O2, O2*− , and *OH (the hydroxyl radical) (88)[88]. As discussed above (see Section 4), mitochondrial OxS is a key factor promoting reduced glycemic control and T2D progression (also see Figure 3). In vitro and ex vivo studies have demonstrated that mitochondrial OxS causes insulin resistance by impairing insulin-regulated GLUT4 translocation to the surface of myotubes (fused skeletal muscle cells) and adipocytes (see Sections 3 and 4 above) (18)[18].
12.2. Vitamin C and Oxidative Stress in T2D
Excess OxS in T2D would be expected to increase the metabolic consumption of AA, thereby lowering its plasma, tissue, and mitochondrial concentrations. Published data consistently shows lower plasma AA levels in patients with T2D (compared to healthy controls), but a lower dietary intake of AA might also be a contributing factor (85, 89-91)[85][89][90][91]. This issue has been addressed by both Bansal et al. (89)[89] and Sinclair et al. (90)[90] with the conclusion that the lower plasma levels of AA observed in patients with T2D are due to increased “demand” rather than inadequate dietary intake. Data provided by Bansal et al. indicates that, even with the daily recommended dietary intake (RDI) of AA, patients with T2D have about half the plasma AA levels found in healthy controls (consuming the RDI) (89)[89].
An important caveat here is, however, the discovery that renal leakage can also contribute to low T2D plasma ascorbate levels and that poor glycemic control, microvascular complications, and obesity correlate with this renal leakage (81)[81]. Chronic kidney disease is very common in patients with T2D and therefore urinary loss of AA can be of real clinical concern (92)[92].
12.3. Vitamin C Supplementation Plays a Positive Role in Adult T2D Management and Progression
An increasing body of literature suggests that AA supplementation plays a potential role in the management of T2D (78-84)[78][79][80][81][82][83][84]. A 2021 meta-analysis by Mason et al. (78) shows that supplementation with AA decreases HbA1c, fasting glucose, and PPG. A noted limitation in this meta-analysis is, however, the lack of randomized controlled trials (RCTs) with sufficient power, as well as short-term study durations (less than six months) (83)[83]. Moreover, the dose of AA used in intervention studies may be an important variable. An RCT in 2007 found that a daily 1000 mg dose, but not a 500 mg dose (for six weeks), was effective in reducing fasting blood glucose and HbA1c in adult patients with T2D (93)[93].
Importantly, all the studies referenced in the above paragraph were conducted with adult populations. Unfortunately, very limited information is available on the potential role of AA in either the progression or management of children with T2D. An epidemiological study of 2025 UK children found that lower plasma AA concentrations were associated with insulin resistance and higher fasting glucose (94)[94]. Future studies are urgently needed to test the hypothesis that increasing plasma AA could help prevent or slow T2D progression in children (94, 95)[94][95].
12.4. Do Synergistic Interactions between Vitamin C and Vitamin E Play a Role in Preventing T2D Pathophysiology?
Compelling in vitro evidence in model systems supports a synergism between alpha-TOH and AA in preventing lipid peroxidation (87, 96-98)[87][96][97][98]. The molecular basis for this in vitro synergy is outlined in Figure 5. AA, despite being water-soluble, can regenerate alpha-TOH (lipid-soluble) from the alpha-tocopheroxyl radical (alpha-TO*) present at the surface of biomembranes (99)[99]. Alpha-TO* radicals are formed by quenching the lipid peroxyl radicals (LOO*) formed during lipid peroxidation with the concurrent formation of lipid hydroperoxides (LOOH). As shown in Figure 2, LOOH can be detoxified by the glutathione peroxidase system. LOO* radicals, if not quenched by alpha-TOH (or other forms of vitamin E), can promote rapid lipid peroxidation propagation reactions in biomembranes or other lipid–protein complexes (e.g., lipoproteins) with polyunsaturated fatty acid (PUFA)-containing lipids (100)[100]. Lipid peroxidation and the chemical products of this process, such as malondialdehyde (MDA) and 4-hydroxy-2-nonenal (4-HNE), can cause functional damage to lipid–protein complexes and alter many physiological processes (100). Biomarkers of lipid peroxidation in T2D patients have been associated with systemic inflammation (101)[101], nephropathy, retinopathy (102)[102], poor glycemic control, and T2D progression (37)[37].
Sato et al. (103)[103] recently presented data from an animal model showing that vitamin C can spare alpha-tocopherol (stereochemistry not specified) in liver and heart tissue but not in other organs that were examined (or plasma). These data show that any sparing in vivo effect of ascorbate on alpha-TOH levels is likely to be tissue/organ-specific. The potential physiological significance of any in vivo vitamin E/C synergy has yet to be firmly established. Most in vivo evidence suggests that such a synergism may be relatively unimportant (96)[96]. A long-term RCT study (12 months) in healthy men found that vitamin E alone (182 mg/day of RRR-alpha-TOH) or in combination with slow-release vitamin C (500 mg/day) reduced in vivo serum-lipid-peroxidation markers (compared to placebo) but vitamin C alone did not (104)[104]. A subsequent in vivo RCT study by Huang et al. (105)[105] in healthy adults looked at daily supplementation (for two months) with vitamin C (500 mg), vitamin E alone (400 IU of RRR-alpha-tocopheryl acetate), or the combination of both. This study found that supplementation with vitamin C alone or vitamin E alone reduced in vivo lipid peroxidation but there was no synergistic effect of supplementing with both vitamins.
It should be kept in mind that most studies attempting to look at the potential in vivo vitamin E/C synergism focus on systemic markers of lipid peroxidation in plasma/serum or urine and not at OxS markers in subcellular organelles, e.g., skeletal muscle mitochondria. In vivo vitamin E/C antioxidant synergy (short and/or long-term) could potentially be important in improving T2D pathogenesis biomarkers other than fasting serum/plasma systemic OxS markers. This possibility has not been adequately tested. Encouragingly, a small RCT study with vitamin C supplementation (1000 mg/day for six weeks) alone found that postprandial OxS (see Section 6) was reduced compared to placebo (106)[106]. Neri et al. found that a daily antioxidant supplement mixture with N-acetylcysteine (600 mg), alpha-TOH (300 mg), and vitamin C (250 mg) reduced postprandial OxS after a moderate-fat meal in healthy adults and patients with T2D: individual antioxidants were not studied (107)[107].
Both in vitro and in vivo studies tend to focus on vitamin E in the form RRR-alpha-TOH and not the tocotrienol forms, which (see Sections 11.5 and 11.6) may be particularly important in T2D pathophysiology. Moreover, plasma/tissue levels of tocotrienols are much lower than those of tocopherols after supplementation and therefore may be more sensitive to OxS depletion and any potential for tocotrienol/vitamin C synergy.
13. Dietary and Supplemental Manganese and T2D
Manganese (Mn) is an essential trace element and a cofactor for the antioxidant enzyme Mn-superoxide dismutase (MnSOD) which is the sole isoform of SOD located in the mitochondrial matrix (see Figure 2). Since mitochondria are a major subcellular site of ROS production, MnSOD is thought to play an important role in preventing ROS-induced cellular damage (108)[108]. As covered above in Section 4, this strongly suggests that MnSOD could play a role in preventing or reversing T2D progression.
The potential roles of Mn status, MnSOD levels, and OxS in T2D have been the subject of both animal and human studies (109-113)[109][110][111][112][113]. These studies reveal a complex pattern that will require further research. In wild-type mice, Lee et al. (109)[109] have demonstrated that Mn supplementation (by injection for 8 weeks) resulted in increased liver MnSOD activity (by 73%) and protection against high-fat-diet-induced diabetes. These authors provide evidence showing that the Mn injection increased insulin secretion and suggest that this effect, along with reduced mitochondrial OxS, could explain the in vivo protection against high-fat-diet-induced diabetes.
Utilizing Zucker diabetic fatty (ZDF) rats as a T2D model, Burlet et al. (110)[110] explored the hypothesis that supplemental Mn (by gavage for 7 weeks) could help prevent vascular inflammation and endothelial dysfunction. In this ZDF model, Mn supplementation reduced glucose-induced monocyte adhesion to endothelial cells as well as endothelial dysfunction. Complementary in vitro experiments showed, however, that this effect was not dependent upon MnSOD expression (110)[110]. This unexpected finding does not rule out other beneficial roles of MnSOD in T2D but does suggest that supplemental Mn has pleiotropic physiological effects.
Although very informative, the role of Mn in human T2D progression has primarily been limited to association/prospective-cohort studies rather than RCTs. Wang et al. (112)[111][112] looked at the association between serum Mn levels and prediabetes in Chinese adults. This study found an inverse association between serum Mn levels and prediabetes suggesting that some populations (particularly women) could potentially benefit from a Mn-rich diet (112)[112].
In prospective cohort studies, Du et al. (111)[111] found that the incidence of T2D was inversely associated with dietary Mn levels. These investigators also utilized a food-frequency questionnaire to calculate the total dietary antioxidant capacity (TAC) for each subject. Dietary TAC provides an overall measure of the total antioxidant capacity arising from complex mixtures of dietary antioxidants (e.g., polyphenols and flavonoids) (114)[113][114]. As reported in the Rotterdam study, dietary TAC is related to a lower risk of T2D and is inversely associated with insulin resistance (114)[114]. Du et al. (111)[111] found that the inverse association of dietary Mn with T2D incidence was independent of TAC suggesting that a high TAC does not “mask” the beneficial effect of dietary Mn. A recent cross-sectional study by Chen et al. (113)[113] looked at the association between serum Mn levels and T2D in a Chinese population with hypertension. These authors found a U-shaped association between serum Mn levels and the T2D odds ratio suggesting that there could be an optimal moderate level of serum Mn for prevention of T2D (113)[113].
The human and animal Mn data reviewed here looks promising for preventing or treating T2D. A strong molecular argument can be made that dietary/supplemental Mn reduces mitochondrial OxS. Nevertheless, there is a notable lack of supporting RCTs. Hopefully, this gap will be the focus of future research.
14. Selenium Supplementation and T2D
Selenium (Se) is an essential trace element and is required for the activity of GPX1–4 and 6, with GPX1 being the most abundant form of the GPXs (115)[115]. Rats deficient in Se exhibit in vivo evidence of OxS, particularly in the retina (116)[116]. A small longitudinal study in 2019 suggests that Se supplementation (200 microgram/daily for six months) in patients with T2D showed improvement in glycemic control and decreased low-density lipoprotein cholesterol levels. A comprehensive review of the role of Se in T2D by Wong et al. (117)[117] provides, however, a critical caution on the blanket use of supplemental Se for individuals with T2D who already have a diet with adequate Se intake. The basis for this caution lies in the U-shaped curve for the dose of Se versus health benefit (117)[117]. This caution should be emphasized for pediatric patients where evidence for the potential role of Se supplementation in T2D progression is minimal.
15. The Role of Beta-Carotene in T2D Prevention
Beta-carotene is the most abundant carotenoid in humans and food and has long been recognized for its antioxidant and anti-inflammatory properties (118)[118]. A comprehensive review suggests that beta-carotene, either in food or as a dietary supplement, may have “a vital influence” in the prevention of T2D (118)[118]. A 2021 meta-analysis of prospective observational studies strongly supports the role of dietary and circulating carotenoids in reducing the risk of T2D (119)[119]. Nevertheless, a very large and long-term RCT indicates that beta-carotene supplementation (50 mg on alternate days for 12 years) in healthy men did not affect the risk of subsequent T2D. While a diet rich in carotenoids looks very promising for reducing T2D risk, the lack of confirming RCT studies with a beta-carotene supplement remains unresolved (119)[119]. Foodstuffs rich in beta-carotene may likely contain other complex mixtures of bioactive nutrients that act synergistically to reduce T2D risk.
16. Conclusions
The evidence reviewed here strongly supports the role of OxS and ROS in both the initiation and progression of T2D. The role of natural antioxidant products in combating T2D is best evaluated in the context of the complex physiological processes associated with its initiation and progression. The consumption of high-calorie, high-fat diets gives rise to transient insulin resistance resulting from mitochondrial OxS. In susceptible individuals, gradual increases in PPG and fasting blood glucose promote systemic OxS with amplifying feedback loops that eventually can cause OxS-induced beta-cell dysfunction and T2D with micro-and macro-vascular damage (see Figure 3). Avoiding high-calorie, high-fat diets, engaging in exercise, and avoiding sleep disturbances are, in effect, key frontline antioxidant strategies. The role of natural antioxidant compounds in combating T2D must likewise be considered beyond their simple roles as inhibitors of in vitro or ex vivo OxS. Vitamin E illustrates this point. While all members of the vitamin E family have powerful in vitro antioxidant properties, they can also exhibit distinct abilities to regulate cellular signal transduction pathways important to T2D progression. While most literature on the role of vitamin E vitamers in T2D or prediabetes has been limited to RRR-alpha-TOH or all-rac-alpha-TOH, emerging trials with tocotrienols show promise. As detailed in Section 11.6, a delta-T3-rich supplement improved glycemic control in adults with prediabetes [120][121][122][123].
The evidence reviewed here supports the very positive role of vitamin C supplementation in T2D prevention and management. Moreover, decades of research attest to the nontoxicity of vitamin C supplementation. In contrast, both Mn and Se supplementation data exhibit U-shaped risk versus dose–response curves, suggesting the importance of careful quality control issues and the need to establish clinical criteria for safe dosing. For beta-carotene, the lack of confirming RCT data limits any suggestion for its use as a supplementation in T2D prevention/management.
References
- Diabetes. Available online: https://www.who.int/news-room/fact-sheets/detail/diabetes (accessed on 12 July 2022).
- Chen, L.; Magliano, D.J.; Zimmet, P.Z. The worldwide epidemiology of type 2 diabetes mellitus—Present and future perspectives. Nat. Rev. Endocrinol. 2011, 8, 228–236. https://doi.org/10.1038/nrendo.2011.183.
- Liu, J.; Li, Y.; Zhang, D.; Yi, S.S. Trends in Prediabetes Among Youths in the US From 1999 Through 2018. JAMA Pediatr. 2022, 176, 608–611. https://doi.org/10.1001/jamapediatrics.2022.0077.
- How Type 2 Diabetes Affects Your Workforce. Available online: https://www.cdc.gov/diabetes/prevention/how-type2-affects-workforce.htm#:~:text=Diabetes%20Is%20Costly,over%20a%205%2Dyear%20period (accessed on 13 July 2022).
- Davidson, K.W.; Barry, M.J.; Mangione, C.M.; Cabana, M.; Caughey, A.B.; Davis, E.M.; Donahue, K.E.; Doubeni, C.A.; Krist, A.H.; Kubik, M.; et al. Screening for Prediabetes and Type 2 Diabetes: US Preventive Services Task Force Recommendation Statement. JAMA 2021, 326, 736–743. https://doi.org/10.1001/jama.2021.12531.
- Prevalence of Both Diagnosed and Undiagnosed Diabetes. Available online: https://www.cdc.gov/diabetes/data/statistics-report/diagnosed-undiagnosed-diabetes.html (accessed on 22 May 2023).
- Reinehr, T. Type 2 diabetes mellitus in children and adolescents. World J. Diabetes 2013, 4, 270–281. https://doi.org/10.4239/wjd.v4.i6.270.
- Pansier, B.; Schulz, P.J. School-based diabetes interventions and their outcomes: A systematic literature review. J. Public Health Res. 2015, 4, 467. https://doi.org/10.4081/jphr.2015.467.
- Alu, S.N.; Los, E.A.; Ford, G.A.; Stone, W.L. Oxidative Stress in Type 2 Diabetes: The Case for Future Pediatric Redoxomics Studies. Antioxidants 2022, 11, 1336.
- Garber, A.J.; Abrahamson, M.J.; Barzilay, J.I.; Blonde, L.; Bloomgarden, Z.T.; Bush, M.A.; Dagogo-Jack, S.; DeFronzo, R.A.; Einhorn, D.; Fonseca, V.A.; et al. Consensus statement by the american association of clinical endocrinologists and american college of endocrinology on the comprehensive type 2 diabetes management algorithm-2018 executive summary. Endocr. Pract. 2018, 24, 91–120. https://doi.org/10.4158/CS-2017-0153.
- Mechanick, J.I.; Garber, A.J.; Grunberger, G.; Handelsman, Y.; Garvey, W.T. Dysglycemia-based chronic disease: An american association of clinical endocrinologists position statement. Endocr Pract. 2018, 24, 995–1011. https://doi.org/10.4158/PS-2018-0139.
- Hansen, T. Type 2 diabetes mellitus--a multifactorial disease. Ann. Univ. Mariae Curie Sklodowska Med. 2002, 57, 544–549.
- Wright, E.; Scism-Bacon, J.L.; Glass, L.C. Oxidative stress in type 2 diabetes: The role of fasting and postprandial glycaemia. Int J. Clin. Pract. 2006, 60, 308–314. https://doi.org/10.1111/j.1368-5031.2006.00825.x.
- Chikezie, P.C.; Ojiako, O.A.; Ogbuji, A.C. Oxidative Stress in Diabetes Mellitus. Int. J. Biol. Chem. 2015, 9, 92–109. https://doi.org/10.3923/ijbc.2015.92.109.
- DeFronzo, R.A.; Tripathy, D. Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care 2009, 32 (Suppl 2), S157–S163. https://doi.org/10.2337/dc09-S302.
- Mueckler, M. Insulin resistance and the disruption of Glut4 trafficking in skeletal muscle. J. Clin. Investig. 2001, 107, 1211–1213. https://doi.org/10.1172/JCI13020.
- Maier, V.H.; Gould, G.W. Long-term insulin treatment of 3T3-L1 adipocytes results in mis-targeting of GLUT4: Implications for insulin-stimulated glucose transport. Diabetologia 2000, 43, 1273–1281. https://doi.org/10.1007/s001250051523.
- Kampmann, U.; Christensen, B.; Nielsen, T.S.; Pedersen, S.B.; Ørskov, L.; Lund, S.; Møller, N.; Jessen, N. GLUT4 and UBC9 protein expression is reduced in muscle from type 2 diabetic patients with severe insulin resistance. PLoS ONE 2011, 6, e27854. https://doi.org/10.1371/journal.pone.0027854.
- Anderson, E.J.; Lustig, M.E.; Boyle, K.E.; Woodlief, T.L.; Kane, D.A.; Lin, C.T.; Price, J.W.; Kang, L.; Rabinovitch, P.S.; Szeto, H.H.; et al. Mitochondrial H2O2 emission and cellular redox state link excess fat intake to insulin resistance in both rodents and humans. J. Clin. Investig. 2009, 119, 573–581. https://doi.org/10.1172/JCI37048.
- Fazakerley, D.J.; Minard, A.Y.; Krycer, J.R.; Thomas, K.C.; Stöckli, J.; Harney, D.J.; Burchfield, J.G.; Maghzal, G.J.; Caldwell, S.T.; Hartley, R.C.; et al. Mitochondrial oxidative stress causes insulin resistance without disrupting oxidative phosphorylation. J. Biol. Chem. 2018, 293, 7315–7328. https://doi.org/10.1074/jbc.RA117.001254.
- Lean, M.E.; Leslie, W.S.; Barnes, A.C.; Brosnahan, N.; Thom, G.; McCombie, L.; Peters, C.; Zhyzhneuskaya, S.; Al-Mrabeh, A.; Hollingsworth, K.G.; et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): An open-label, cluster-randomised trial. Lancet 2018, 391, 541–551. https://doi.org/10.1016/S0140-6736(17)33102-1.
- Juray, S.; Axen, K.V.; Trasino, S.E. Remission of Type 2 Diabetes with Very Low-Calorie Diets-A Narrative Review. Nutrients 2021, 13, 2086. https://doi.org/10.3390/nu13062086.
- Maffettone, A.; Rinaldi, M.; Fontanella, A. Postprandial hyperglycemia: A new frontier in diabetes management? Ital. J. Med. 2018, 12, 108–115. https://doi.org/10.4081/itjm.2018.961.
- Sottero, B.; Gargiulo, S.; Russo, I.; Barale, C.; Poli, G.; Cavalot, F. Postprandial Dysmetabolism and Oxidative Stress in Type 2 Diabetes: Pathogenetic Mechanisms and Therapeutic Strategies. Med. Res. Rev. 2015, 35, 968–1031. https://doi.org/10.1002/med.21349.
- Cavalot, F.; Petrelli, A.; Traversa, M.; Bonomo, K.; Fiora, E.; Conti, M.; Anfossi, G.; Costa, G.; Trovati, M. Postprandial blood glucose is a stronger predictor of cardiovascular events than fasting blood glucose in type 2 diabetes mellitus, particularly in women: Lessons from the San Luigi Gonzaga Diabetes Study. J. Clin. Endocrinol. Metab. 2006, 91, 813–819. https://doi.org/10.1210/jc.2005-1005.
- Cavalot, F.; Pagliarino, A.; Valle, M.; Di Martino, L.; Bonomo, K.; Massucco, P.; Anfossi, G.; Trovati, M. Postprandial blood glucose predicts cardiovascular events and all-cause mortality in type 2 diabetes in a 14-year follow-up: Lessons from the San Luigi Gonzaga Diabetes Study. Diabetes Care 2011, 34, 2237–2243. https://doi.org/10.2337/dc10-2414.
- Singh, R.; Barden, A.; Mori, T.; Beilin, L. Advanced glycation end-products: A review. Diabetologia 2001, 44, 129–146. https://doi.org/10.1007/s001250051591.
- Vlassara, H.; Uribarri, J. Advanced glycation end products (AGE) and diabetes: Cause, effect, or both? Curr. Diab. Rep. 2014, 14, 453. https://doi.org/10.1007/s11892-013-0453-1.
- Greifenhagen, U.; Frolov, A.; Blüher, M.; Hoffmann, R. Plasma Proteins Modified by Advanced Glycation End Products (AGEs) Reveal Site-specific Susceptibilities to Glycemic Control in Patients with Type 2 Diabetes. J. Biol. Chem. 2016, 291, 9610–9616. https://doi.org/10.1074/jbc.M115.702860.
- Ando, K.; Beppu, M.; Kikugawa, K.; Nagai, R.; Horiuchi, S. Membrane proteins of human erythrocytes are modified by advanced glycation end products during aging in the circulation. Biochem. Biophys. Res. Commun. 1999, 258, 123–127. https://doi.org/10.1006/bbrc.1999.0606.
- Yan, L.J. Redox imbalance stress in diabetes mellitus: Role of the polyol pathway. Anim. Model Exp. Med. 2018, 1, 7–13. https://doi.org/10.1002/ame2.12001.
- Pinto-Junior, D.C.; Silva, K.S.; Michalani, M.L.; Yonamine, C.Y.; Esteves, J.V.; Fabre, N.T.; Thieme, K.; Catanozi, S.; Okamoto, M.M.; Seraphim, P.M.; et al. Advanced glycation end products-induced insulin resistance involves repression of skeletal muscle GLUT4 expression. Sci. Rep. 2018, 8, 8109. https://doi.org/10.1038/s41598-018-26482-6.
- Drews, G.; Krippeit-Drews, P.; Düfer, M. Oxidative stress and beta-cell dysfunction. Pflug. Arch. 2010, 460, 703–718. https://doi.org/10.1007/s00424-010-0862-9.
- Stirban, A.; Gawlowski, T.; Roden, M. Vascular effects of advanced glycation endproducts: Clinical effects and molecular mechanisms. Mol. Metab. 2014, 3, 94–108. https://doi.org/10.1016/j.molmet.2013.11.006.
- Schleicher, E.; Friess, U. Oxidative stress, AGE, and atherosclerosis. Kidney Int. Suppl. 2007, 72, S17–S26. https://doi.org/10.1038/sj.ki.5002382.
- Powers, S.K.; Radak, Z.; Ji, L.L. Exercise-induced oxidative stress: Past, present and future. J. Physiol. 2016, 594, 5081–5092. https://doi.org/10.1113/JP270646.
- Ristow, M.; Zarse, K.; Oberbach, A.; Klöting, N.; Birringer, M.; Kiehntopf, M.; Stumvoll, M.; Kahn, C.R.; Blüher, M. Antioxidants prevent health-promoting effects of physical exercise in humans. Proc. Natl. Acad. Sci. USA 2009, 106, 8665–8670. https://doi.org/10.1073/pnas.0903485106.
- Woerle, H.J.; Neumann, C.; Zschau, S.; Tenner, S.; Irsigler, A.; Schirra, J.; Gerich, J.E.; Göke, B. Impact of fasting and postprandial glycemia on overall glycemic control in type 2 diabetes Importance of postprandial glycemia to achieve target HbA1c levels. Diabetes Res. Clin. Pract. 2007, 77, 280–285. https://doi.org/10.1016/j.diabres.2006.11.011.
- Gunawardena, H.P.; Silva, R.; Sivakanesan, R.; Ranasinghe, P.; Katulanda, P. Poor Glycaemic Control Is Associated with Increased Lipid Peroxidation and Glutathione Peroxidase Activity in Type 2 Diabetes Patients. Oxid. Med. Cell Longev. 2019, 2019, 9471697. https://doi.org/10.1155/2019/9471697.
- Colberg, S.R.; Sigal, R.J.; Yardley, J.E.; Riddell, M.C.; Dunstan, D.W.; Dempsey, P.C.; Horton, E.S.; Castorino, K.; Tate, D.F. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care 2016, 39, 2065–2079. https://doi.org/10.2337/dc16-1728.
- van Dijk, J.W.; van Loon, L.J. Exercise strategies to optimize glycemic control in type 2 diabetes: A continuing glucose monitoring perspective. Diabetes Spectr. 2015, 28, 24–31. https://doi.org/10.2337/diaspect.28.1.24.
- Velicer, C. Available online: https://thrivingschools.kaiserpermanente.org/kids-and-type-2-diabetes-how-parents-and-teachers-can-help-curb-the-tide/ (accessed on 13 September 2022).
- Buffey, A.J.; Herring, M.P.; Langley, C.K.; Donnelly, A.E.; Carson, B.P. The Acute Effects of Interrupting Prolonged Sitting Time in Adults with Standing and Light-Intensity Walking on Biomarkers of Cardiometabolic Health in Adults: A Systematic Review and Meta-analysis. Sport. Med. 2022, 52, 1765–1787. https://doi.org/10.1007/s40279-022-01649-4.
- Singla, P.; Bardoloi, A.; Parkash, A.A. Metabolic effects of obesity: A review. World J. Diabetes 2010, 1, 76–88. https://doi.org/10.4239/wjd.v1.i3.76.
- Chang, T.; Li, H.; Zhang, N.; Jiang, X.; Yu, X.; Yang, Q.; Jin, Z.; Meng, H.; Chang, L. Highly integrated watch for noninvasive continual glucose monitoring. Microsyst. Nanoeng. 2022, 8, 25. https://doi.org/10.1038/s41378-022-00355-5.
- Rodriguez-León, C.; Villalonga, C.; Munoz-Torres, M.; Ruiz, J.R.; Banos, O. Mobile and Wearable Technology for the Monitoring of Diabetes-Related Parameters: Systematic Review. JMIR Mhealth Uhealth 2021, 9, e25138. https://doi.org/10.2196/25138.
- Van Dijk, J.W.; Venema, M.; van Mechelen, W.; Stehouwer, C.D.; Hartgens, F.; van Loon, L.J. Effect of moderate-intensity exercise versus activities of daily living on 24-hour blood glucose homeostasis in male patients with type 2 diabetes. Diabetes Care 2013, 36, 3448–3453. https://doi.org/10.2337/dc12-2620.
- Flores-Opazo, M.; McGee, S.L.; Hargreaves, M. Exercise and GLUT4. Exerc. Sport Sci. Rev. 2020, 48, 110–118. https://doi.org/10.1249/JES.0000000000000224.
- Richter, E.A.; Hargreaves, M. Exercise, GLUT4, and skeletal muscle glucose uptake. Physiol. Rev. 2013, 93, 993–1017. https://doi.org/10.1152/physrev.00038.2012.
- Kraniou, G.N.; Cameron-Smith, D.; Hargreaves, M. Acute exercise and GLUT4 expression in human skeletal muscle: Influence of exercise intensity. J. Appl. Physiol. 2006, 101, 934–937. https://doi.org/10.1152/japplphysiol.01489.2005.
- Kawamura, T.; Muraoka, I. Exercise-Induced Oxidative Stress and the Effects of Antioxidant Intake from a Physiological Viewpoint. Antioxidants 2018, 7, 119. https://doi.org/10.3390/antiox7090119.
- Quindry, J.; Stone, W.; King, J.; Broeder, C. The effects of acute exercise on neutrophils and plasma oxidative stress. Med. Sci. Sport. Exerc. 2003, 35, 1139–1145.
- Powers, S.K.; Deminice, R.; Ozdemir, M.; Yoshihara, T.; Bomkamp, M.P.; Hyatt, H. Exercise-induced oxidative stress: Friend or foe? J. Sport Health Sci. 2020, 9, 415–425. https://doi.org/10.1016/j.jshs.2020.04.001.
- Thannickal, V.J.; Fanburg, B.L. Reactive oxygen species in cell signaling. Am. J. Physiol. Lung Cell Mol. Physiol. 2000, 279,
L1005–L1028. https://doi.org/10.1152/ajplung.2000.279.6.L1005. - Hancock, J.T.; Desikan, R.; Neill, S.J. Role of reactive oxygen species in cell signalling pathways. Biochem. Soc. Trans. 2001, 29, 345–350. https://doi.org/10.1042/0300-5127:0290345.
- Cobley, J.N.; McHardy, H.; Morton, J.P.; Nikolaidis, M.G.; Close, G.L. Influence of vitamin C and vitamin E on redox signaling: Implications for exercise adaptations. Free Radic. Biol. Med. 2015, 84, 65–76. https://doi.org/10.1016/j.freeradbiomed.2015.03.018.
- Reid, M.B. Nitric oxide, reactive oxygen species, and skeletal muscle contraction. Med. Sci. Sport. Exerc. 2001, 33, 371–376. https://doi.org/10.1097/00005768-200103000-00006.
- He, F.; Li, J.; Liu, Z.; Chuang, C.C.; Yang, W.; Zuo, L. Redox Mechanism of Reactive Oxygen Species in Exercise. Front. Physiol. 2016, 7, 486. https://doi.org/10.3389/fphys.2016.00486.
- Ji, L.L. Antioxidant enzyme response to exercise and aging. Med. Sci. Sport. Exerc. 1993, 25, 225–231.
- Lipska, K.J. Patient education: Exercise and medical care for people with type 2 diabetes (Beyond the Basics). Available online: www.uptodate.com/contents/exercise-and-medical-care-for-people-with-type-2-diabetes-beyond-the-basics (accessed on 22 May 2023).
- Khandelwal, D.; Dutta, D.; Chittawar, S.; Kalra, S. Sleep Disorders in Type 2 Diabetes. Indian J. Endocrinol. Metab. 2017, 21,
758–761. https://doi.org/10.4103/ijem.IJEM_156_17. - Kelly, S.J.; Ismail, M. Stress and type 2 diabetes: A review of how stress contributes to the development of type 2 diabetes. Annu. Rev. Public Health 2015, 36, 441–462. https://doi.org/10.1146/annurev-publhealth-031914-122921.
- Atrooz, F.; Salim, S. Sleep deprivation, oxidative stress and inflammation. Adv. Protein Chem. Struct. Biol. 2020, 119, 309–336. https://doi.org/10.1016/bs.apcsb.2019.03.001.
- Hill, V.M.; O’Connor, R.M.; Sissoko, G.B.; Irobunda, I.S.; Leong, S.; Canman, J.C.; Stavropoulos, N.; Shirasu-Hiza, M. A bidirectional relationship between sleep and oxidative stress in Drosophila. PLoS Biol. 2018, 16, e2005206. https://doi.org/10.1371/journal.pbio.2005206.
- Moller, P.; Wallin, H.; Knudsen, L.E. Oxidative stress associated with exercise, psychological stress and life-style factors. Chem. Biol. Interact. 1996, 102, 17–36. Available online: http://biomednet.com/db/medline/96424598 (accessed on).
- Belaïdi, E. Oxidative Stress and Sleep Disorders. Available online: https://www.mdpi.com/journal/antioxidants/special_issues/Oxidative_Stress_and_Sleep_Disorders (accessed on 26 April 2023).
- Lauridsen, C.; Jensen, S.K. α-Tocopherol incorporation in mitochondria and microsomes upon supranutritional vitamin E supplementation. Genes Nutr. 2012, 7, 475–482. https://doi.org/10.1007/s12263-012-0286-6.
- Sen, C.K.; Khanna, S.; Roy, S. Tocotrienols in health and disease: The other half of the natural vitamin E family. Mol. Asp. Med. 2007, 28, 692–728. https://doi.org/10.1016/j.mam.2007.03.001.
- Azzi, A.; Gysin, R.; Kempna, P.; Munteanu, A.; Negis, Y.; Villacorta, L.; Visarius, T.; Zingg, J.M. Vitamin E mediates cell signaling and regulation of gene expression. Ann. N. Y. Acad. Sci. 2004, 1031, 86–95.
- Zingg, J.M. Vitamin E: A Role in Signal Transduction. Annu. Rev. Nutr. 2015, 35, 135–173. https://doi.org/10.1146/annurev-nutr-071714-034347.
- Balbi, M.E.; Tonin, F.S.; Mendes, A.M.; Borba, H.H.; Wiens, A.; Fernandez-Llimos, F.; Pontarolo, R. Antioxidant effects of vitamins in type 2 diabetes: A meta-analysis of randomized controlled trials. Diabetol. Metab. Syndr. 2018, 10, 18. https://doi.org/10.1186/s13098-018-0318-5.
- Chow, C.K.; Ibrahim, W.; Wei, Z.; Chan, A.C. Vitamin E regulates mitochondrial hydrogen peroxide generation. Free Radic. Biol. Med. 1999, 27, 580–587. https://doi.org/10.1016/s0891-5849(99)00121-5.
- El-Aal, A.A.; El-Ghffar, E.A.A.; Ghali, A.A.; Zughbur, M.R.; Sirdah, M.M. The effect of vitamin C and/or E supplementations on type 2 diabetic adult males under metformin treatment: A single-blinded randomized controlled clinical trial. Diabetes Metab. Syndr. 2018, 12, 483–489. https://doi.org/10.1016/j.dsx.2018.03.013.
- Vafa, M.; Haghighat, N.; Moslehi, N.; Eghtesadi, S.; Heydari, I. Effect of Tocotrienols enriched canola oil on glycemic control and oxidative status in patients with type 2 diabetes mellitus: A randomized double-blind placebo-controlled clinical trial. J. Res. Med. Sci. 2015, 20, 540–547. https://doi.org/10.4103/1735-1995.165945.
- Baliarsingh, S.; Beg, Z.H.; Ahmad, J. The therapeutic impacts of tocotrienols in type 2 diabetic patients with hyperlipidemia. Atherosclerosis 2005, 182, 367–374. https://doi.org/10.1016/j.atherosclerosis.2005.02.020.
- Ho, J.I.; Ng, E.Y.; Chiew, Y.; Koay, Y.Y.; Chuar, P.F.; Phang, S.C.W.; Ahmad, B.; Kadir, K.A. The effects of vitamin E on non-proliferative diabetic retinopathy in type 2 diabetes mellitus: Are they sustainable with 12 months of therapy. SAGE Open Med. 2022, 10, https://doi.org/10.1177/20503121221095324.
- Kalvaitus, K.; Portnoy, S.A. Available online: https://www.healio.com/news/endocrinology/20120325/experts-recommend-two-pronged-approach-to-treating-prediabetes (accessed on 11 January 2023).
- Suleman, F.; Khan, D.A.; Pervez, M.A.; Aamir, M. Effects of delta-tocotrienol supplementation on glycaemic control in individuals with prediabetes: A randomized controlled study. J. Pak. Med. Assoc. 2022, 72, 4–7. https://doi.org/10.47391/JPMA.966.
- Fang, F.; Kang, Z.; Wong, C. Vitamin E tocotrienols improve insulin sensitivity through activating peroxisome proliferator-activated receptors. Mol. Nutr. Food Res. 2010, 54, 345–352. https://doi.org/10.1002/mnfr.200900119.
- Mason, S.A.; Parker, L.; van der Pligt, P.; Wadley, G.D. Vitamin C supplementation for diabetes management: A comprehensive narrative review. Free Radic. Biol. Med. 2023, 194, 255–283. https://doi.org/10.1016/j.freeradbiomed.2022.12.003.
- Sun, H.; Karp, J.; Sun, K.M.; Weaver, C.M. Decreasing Vitamin C Intake, Low Serum Vitamin C Level and Risk for US Adults with Diabetes. Nutrients 2022, 14, 3902. https://doi.org/10.3390/nu14193902.
- Liu, M.; Park, S. A Causal Relationship between Vitamin C Intake with Hyperglycemia and Metabolic Syndrome Risk: A Two-Sample Mendelian Randomization Study. Antioxidants 2022, 11, 857. https://doi.org/10.3390/antiox11050857.
- Ebenuwa, I.; Violet, P.C.; Padayatty, S.; Wang, Y.; Sun, H.; Adhikari, P.; Smith, S.; Tu, H.; Niyyati, M.; Wilkins, K.; et al. Abnormal urinary loss of vitamin C in diabetes: Prevalence and clinical characteristics of a vitamin C renal leak. Am. J. Clin. Nutr. 2022, 116, 274–284. https://doi.org/10.1093/ajcn/nqac063.
- Shi, L.; Du, X.; Guo, P.; Huang, L.; Qi, P.; Gong, Q. Ascorbic acid supplementation in type 2 diabetes mellitus: A protocol for systematic review and meta-analysis. Medicine 2020, 99, e23125. https://doi.org/10.1097/MD.0000000000023125.
- Mason, S.A.; Keske, M.A.; Wadley, G.D. Effects of Vitamin C Supplementation on Glycemic Control and Cardiovascular Risk Factors in People With Type 2 Diabetes: A GRADE-Assessed Systematic Review and Meta-analysis of Randomized Controlled Trials. Diabetes Care 2021, 44, 618–630. https://doi.org/10.2337/dc20-1893.
- Jiang, C.L.; Tsao, C.Y.; Lee, Y.C. Vitamin C attenuates predisposition to high-fat diet-induced metabolic dysregulation in GLUT10-deficient mouse model. Genes Nutr. 2022, 17, 10. https://doi.org/10.1186/s12263-022-00713-y.
- Wilson, R.; Willis, J.; Gearry, R.; Skidmore, P.; Fleming, E.; Frampton, C.; Carr, A. Inadequate Vitamin C Status in Prediabetes and Type 2 Diabetes Mellitus: Associations with Glycaemic Control, Obesity, and Smoking. Nutrients 2017, 9, 997. https://doi.org/10.3390/nu9090997.
- Stanimirovic, J.; Radovanovic, J.; Banjac, K.; Obradovic, M.; Essack, M.; Zafirovic, S.; Gluvic, Z.; Gojobori, T.; Isenovic, E.R. Role of C-Reactive Protein in Diabetic Inflammation. Mediat. Inflamm 2022, 2022, 3706508. https://doi.org/10.1155/2022/3706508.
- Valko, M.; Izakovic, M.; Mazur, M.; Rhodes, C.J.; Telser, J. Role of oxygen radicals in DNA damage and cancer incidence. Mol. Cell Biochem. 2004, 266, 37–56. https://doi.org/10.1023/b:mcbi.0000049134.69131.89.
- Sagun, K.C.; Cárcamo, J.M.; Golde, D.W. Vitamin C enters mitochondria via facilitative glucose transporter 1 (Glut1) and confers mitochondrial protection against oxidative injury. FASEB J. 2005, 19, 1657–1667. https://doi.org/10.1096/fj.05-4107com.
- Bansal, A.; Hadimani, C.P. Low Plasma Ascorbate Levels in Type 2 Diabetic Patients With Adequate Dietary Vitamin C. J. Lab. Physicians 2021, 13, 139–143. https://doi.org/10.1055/s-0041-1730751.
- Sinclair, A.J.; Taylor, P.B.; Lunec, J.; Girling, A.J.; Barnett, A.H. Low plasma ascorbate levels in patients with type 2 diabetes mellitus consuming adequate dietary vitamin C. Diabet. Med. 1994, 11, 893–898. https://doi.org/10.1111/j.1464-5491.1994.tb00375.x.
- Chen, H.; Karne, R.J.; Hall, G.; Campia, U.; Panza, J.A.; Cannon, R.O.; Wang, Y.; Katz, A.; Levine, M.; Quon, M.J. High-dose oral vitamin C partially replenishes vitamin C levels in patients with Type 2 diabetes and low vitamin C levels but does not improve endothelial dysfunction or insulin resistance. Am. J. Physiol. Heart Circ. Physiol. 2006, 290, H137–145. https://doi.org/10.1152/ajpheart.00768.2005.
- Bonner, R.; Albajrami, O.; Hudspeth, J.; Upadhyay, A. Diabetic Kidney Disease. Prim. Care 2020, 47, 645–659. https://doi.org/10.1016/j.pop.2020.08.004.
- Afkhami-Ardekani, M.; Shojaoddiny-Ardekani, A. Effect of vitamin C on blood glucose, serum lipids & serum insulin in type 2 diabetes patients. Indian J. Med. Res. 2007, 126, 471–474.
- Donin, A.S.; Dent, J.E.; Nightingale, C.M.; Sattar, N.; Owen, C.G.; Rudnicka, A.R.; Perkin, M.R.; Stephen, A.M.; Jebb, S.A.; Cook, D.G.; et al. Fruit, vegetable and vitamin C intakes and plasma vitamin C: Cross-sectional associations with insulin resistance and glycaemia in 9–10 year-old children. Diabet. Med. 2016, 33, 307–315. https://doi.org/10.1111/dme.13006.
- Parajuli, S.; Jasmin, G.; Sirak, H.; Lee, A.F.; Nwosu, B.U. Prediabetes: Adherence to Nutrition Visits Decreases HbA1c in Children and Adolescents. Front. Endocrinol. 2022, 13, 916785. https://doi.org/10.3389/fendo.2022.916785.
- Strain, J.J.; Mulholland, C.W. Vitamin C and vitamin E--synergistic interactions in vivo? EXS 1992, 62, 419–422. https://doi.org/10.1007/978-3-0348-7460-1_40.
- Azzi, A. Tocopherols, tocotrienols and tocomonoenols: Many similar molecules but only one vitamin E. Redox Biol. 2019, 26, 101259. https://doi.org/10.1016/j.redox.2019.101259.
- Pangrazzi, L.; Balasco, L.; Bozzi, Y. Natural Antioxidants: A Novel Therapeutic Approach to Autism Spectrum Disorders? Antioxidants 2020, 9, 1186. https://doi.org/10.3390/antiox9121186.
- Buettner, G.R. The pecking order of free radicals and antioxidants: Lipid peroxidation, alpha-tocopherol, and ascorbate. Arch. Biochem. Biophys. 1993, 300, 535–543. https://doi.org/10.1006/abbi.1993.1074.
- Ayala, A.; Muñoz, M.F.; Argüelles, S. Lipid peroxidation: Production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxid. Med. Cell Longev. 2014, 2014, 360438. https://doi.org/10.1155/2014/360438.
- de Souza Bastos, A.; Graves, D.T.; de Melo Loureiro, A.P.; Júnior, C.R.; Corbi, S.C.T.; Frizzera, F.; Scarel-Caminaga, R.M.; Câmara, N.O.; Andriankaja, O.M.; Hiyane, M.I.; et al. Diabetes and increased lipid peroxidation are associated with systemic inflammation even in well-controlled patients. J. Diabetes Complicat. 2016, 30, 1593–1599. https://doi.org/10.1016/j.jdiacomp.2016.07.011.
- Augustine, J.; Troendle, E.P.; Barabas, P.; McAleese, C.A.; Friedel, T.; Stitt, A.W.; Curtis, T.M. The Role of Lipoxidation in the Pathogenesis of Diabetic Retinopathy. Front. Endocrinol. 2020, 11, 621938. https://doi.org/10.3389/fendo.2020.621938.
- Sato, A.; Takino, Y.; Yano, T.; Fukui, K.; Ishigami, A. Determination of tissue-specific interaction between vitamin C and vitamin E. Br. J. Nutr. 2022, 128, 993–1003. https://doi.org/10.1017/S0007114521004384.
- Porkkala-Sarataho, E.; Salonen, J.T.; Nyyssönen, K.; Kaikkonen, J.; Salonen, R.; Ristonmaa, U.; Diczfalusy, U.; Brigelius-Flohe, R.; Loft, S.; Poulsen, H.E. Long-term effects of vitamin E, vitamin C, and combined supplementation on urinary 7-hydro-8-oxo-2’-deoxyguanosine, serum cholesterol oxidation products, and oxidation resistance of lipids in nondepleted men. Arter. Thromb. Vasc. Biol. 2000, 20, 2087–2093. https://doi.org/10.1161/01.atv.20.9.2087.
- Huang, H.Y.; Appel, L.J.; Croft, K.D.; Miller, E.R.; Mori, T.A.; Puddey, I.B. Effects of vitamin C and vitamin E on in vivo lipid peroxidation: Results of a randomized controlled trial. Am. J. Clin. Nutr. 2002, 76, 549–555. https://doi.org/10.1093/ajcn/76.3.549.
- Mazloom, Z.; Hejazi, N.; Dabbaghmanesh, M.H.; Tabatabaei, H.R.; Ahmadi, A.; Ansar, H. Effect of vitamin C supplementation on postprandial oxidative stress and lipid profile in type 2 diabetic patients. Pak. J. Biol. Sci. 2011, 14, 900–904. https://doi.org/10.3923/pjbs.2011.900.904.
- Neri, S.; Calvagno, S.; Mauceri, B.; Misseri, M.; Tsami, A.; Vecchio, C.; Mastrosimone, G.; Di Pino, A.; Maiorca, D.; Judica, A.; et al. Effects of antioxidants on postprandial oxidative stress and endothelial dysfunction in subjects with impaired glucose tolerance and type 2 diabetes. Eur. J. Nutr. 2010, 49, 409–416. https://doi.org/10.1007/s00394-010-0099-6.
- Holley, A.K.; Bakthavatchalu, V.; Velez-Roman, J.M.; St Clair, D.K. Manganese superoxide dismutase: Guardian of the powerhouse. Int. J. Mol. Sci. 2011, 12, 7114–7162. https://doi.org/10.3390/ijms12107114.
- Lee, S.H.; Jouihan, H.A.; Cooksey, R.C.; Jones, D.; Kim, H.J.; Winge, D.R.; McClain, D.A. Manganese supplementation protects against diet-induced diabetes in wild type mice by enhancing insulin secretion. Endocrinology 2013, 154, 1029–1038. https://doi.org/10.1210/en.2012-1445.
- Burlet, E.; Jain, S.K. Manganese supplementation reduces high glucose-induced monocyte adhesion to endothelial cells and endothelial dysfunction in Zucker diabetic fatty rats. J. Biol. Chem. 2013, 288, 6409–6416. https://doi.org/10.1074/jbc.M112.447805.
- Du, S.; Wu, X.; Han, T.; Duan, W.; Liu, L.; Qi, J.; Niu, Y.; Na, L.; Sun, C. Dietary manganese and type 2 diabetes mellitus: Two prospective cohort studies in China. Diabetologia 2018, 61, 1985–1995. https://doi.org/10.1007/s00125-018-4674-3.
- Wang, X.; Zhang, M.; Lui, G.; Chang, H.; Liu, W.; Li, Z.; Liu, Y.; Huang, G. Associations of Serum Manganese Levels with Prediabetes and Diabetes among ≥60-Year-Old Chinese Adults: A Population-Based Cross-Sectional Analysis. Nutrients 2016, 8, 497. https://doi.org/10.3390/nu8080497.
- Chen, H.; Cui, Z.; Lu, W.; Wang, P.; Wang, J.; Zhou, Z.; Zhang, N.; Wang, Z.; Lin, T.; Song, Y.; et al. Association between serum manganese levels and diabetes in Chinese adults with hypertension. J. Clin. Hypertens 2022, 24, 918–927. https://doi.org/10.1111/jch.14520.
- van der Schaft, N.; Schoufour, J.D.; Nano, J.; Kiefte-de Jong, J.C.; Muka, T.; Sijbrands, E.J.G.; Ikram, M.A.; Franco, O.H.; Voortman, T. Dietary antioxidant capacity and risk of type 2 diabetes mellitus, prediabetes and insulin resistance: The Rotterdam Study. Eur. J. Epidemiol. 2019, 34, 853–861. https://doi.org/10.1007/s10654-019-00548-9.
- Brigelius-Flohé, R.; Flohé, L. Regulatory Phenomena in the Glutathione Peroxidase Superfamily. Antioxid. Redox Signal. 2020, 33, 498–516. https://doi.org/10.1089/ars.2019.7905.
- Katz, M.L.; Stone, W.L.; Dratz, E.A. Fluorescent pigment accumulation in retinal pigment epithelium of antioxidant-deficient rats. Investig. Ophthalmol. Vis. Sci. 1978, 17, 1049–1058.
- Ogawa-Wong, A.N.; Berry, M.J.; Seale, L.A. Selenium and Metabolic Disorders: An Emphasis on Type 2 Diabetes Risk. Nutrients 2016, 8, 80. https://doi.org/10.3390/nu8020080.
- Marcelino, G.; Machate, D.J.; Freitas, K.C.; Hiane, P.A.; Maldonade, I.R.; Pott, A.; Asato, M.A.; Candido, C.J.; Guimarães, R.C.A. β-Carotene: Preventive Role for Type 2 Diabetes Mellitus and Obesity: A Review. Molecules 2020, 25, 5803. https://doi.org/10.3390/molecules25245803.
- Jiang, Y.W.; Sun, Z.H.; Tong, W.W.; Yang, K.; Guo, K.Q.; Liu, G.; Pan, A. Dietary Intake and Circulating Concentrations of Carotenoids and Risk of Type 2 Diabetes: A Dose-Response Meta-Analysis of Prospective Observational Studies. Adv. Nutr. 2021, 12, 1723–1733. https://doi.org/10.1093/advances/nmab048.
- Available online: https://www.aap.org/en/practice-management/bright-futures/bright-futures-materials-and-tools/bright-futures-guidelines-and-pocket-guide/ (accessed on 11 January 2023).
- Eddolls, W.T.B.; McNarry, M.A.; Stratton, G.; Winn, C.O.N.; Mackintosh, K.A. High-Intensity Interval Training Interventions in Children and Adolescents: A Systematic Review. Sport. Med. 2017, 47, 2363–2374. https://doi.org/10.1007/s40279-017-0753-8.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content.
1. W. diabetes: Diabetes https://www.who.int/news-room/fact-sheets/detail/diabetes. In: Ed W. H. Organization. (2021)
2. L. Chen, D. J. Magliano and P. Z. Zimmet: The worldwide epidemiology of type 2 diabetes mellitus--present and future perspectives. Nat Rev Endocrinol, 8(4), 228-36 (2011) doi:10.1038/nrendo.2011.183
3. J. Liu, Y. Li, D. Zhang and S. S. Yi: Trends in Prediabetes Among Youths in the US From 1999 Through 2018. JAMA Pediatr, 176(6), 608-611 (2022) doi:10.1001/jamapediatrics.2022.0077
4. C. workforce: How Type 2 Diabetes Affects Your Workforce, https://www.cdc.gov/diabetes/prevention/how-type2-affects-workforce.htm#:~:text=Diabetes%20Is%20Costly,over%20a%205%2Dyear%20period. In: Ed C. f. D. Control. (2021)
5. K. W. Davidson, M. J. Barry, C. M. Mangione, M. Cabana, A. B. Caughey, E. M. Davis, K. E. Donahue, C. A. Doubeni, A. H. Krist, M. Kubik, L. Li, G. Ogedegbe, D. K. Owens, L. Pbert, M. Silverstein, J. Stevermer, C. W. Tseng, J. B. Wong and U. P. S. T. Force: Screening for Prediabetes and Type 2 Diabetes: US Preventive Services Task Force Recommendation Statement. JAMA, 326(8), 736-743 (2021) doi:10.1001/jama.2021.12531
6. B. Pansier and P. J. Schulz: School-based diabetes interventions and their outcomes: a systematic literature review. J Public Health Res, 4(1), 467 (2015) doi:10.4081/jphr.2015.467
7. S. N. Alu, E. A. Los, G. A. Ford and W. L. Stone: Oxidative Stress in Type 2 Diabetes: The Case for Future Pediatric Redoxomics Studies. Antioxidants, 11(7), 1336 (2022)
8. A. J. Garber, M. J. Abrahamson, J. I. Barzilay, L. Blonde, Z. T. Bloomgarden, M. A. Bush, S. Dagogo-Jack, R. A. DeFronzo, D. Einhorn, V. A. Fonseca, J. R. Garber, W. T. Garvey, G. Grunberger, Y. Handelsman, I. B. Hirsch, P. S. Jellinger, J. B. McGill, J. I. Mechanick, P. D. Rosenblit and G. E. Umpierrez: CONSENSUS STATEMENT BY THE AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS AND AMERICAN COLLEGE OF ENDOCRINOLOGY ON THE COMPREHENSIVE TYPE 2 DIABETES MANAGEMENT ALGORITHM - 2018 EXECUTIVE SUMMARY. Endocr Pract, 24(1), 91-120 (2018) doi:10.4158/CS-2017-0153
9. J. I. Mechanick, A. J. Garber, G. Grunberger, Y. Handelsman and W. T. Garvey: DYSGLYCEMIA-BASED CHRONIC DISEASE: AN AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS POSITION STATEMENT. Endocr Pract, 24(11), 995-1011 (2018) doi:10.4158/PS-2018-0139
10. T. Hansen: Type 2 diabetes mellitus--a multifactorial disease. Ann Univ Mariae Curie Sklodowska Med, 57(1), 544-9 (2002)
11. E. Wright, J. L. Scism-Bacon and L. C. Glass: Oxidative stress in type 2 diabetes: the role of fasting and postprandial glycaemia. Int J Clin Pract, 60(3), 308-14 (2006) doi:10.1111/j.1368-5031.2006.00825.x
12. P. C. Chikezie, O. A. Ojiako and A. C. Ogbuji: Oxidative Stress in Diabetes Mellitus. International Journal of Biological Chemistry, 9(3), 92-109 (2015) doi:10.3923/ijbc.2015.92.109
13. R. A. DeFronzo and D. Tripathy: Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care, 32 Suppl 2, S157-63 (2009) doi:10.2337/dc09-S302
14. M. Mueckler: Insulin resistance and the disruption of Glut4 trafficking in skeletal muscle. J Clin Invest, 107(10), 1211-3 (2001) doi:10.1172/JCI13020
15. V. H. Maier and G. W. Gould: Long-term insulin treatment of 3T3-L1 adipocytes results in mis-targeting of GLUT4: implications for insulin-stimulated glucose transport. Diabetologia, 43(10), 1273-81 (2000) doi:10.1007/s001250051523
16. U. Kampmann, B. Christensen, T. S. Nielsen, S. B. Pedersen, L. Ørskov, S. Lund, N. Møller and N. Jessen: GLUT4 and UBC9 protein expression is reduced in muscle from type 2 diabetic patients with severe insulin resistance. PLoS One, 6(11), e27854 (2011) doi:10.1371/journal.pone.0027854
17. E. J. Anderson, M. E. Lustig, K. E. Boyle, T. L. Woodlief, D. A. Kane, C. T. Lin, J. W. Price, L. Kang, P. S. Rabinovitch, H. H. Szeto, J. A. Houmard, R. N. Cortright, D. H. Wasserman and P. D. Neufer: Mitochondrial H2O2 emission and cellular redox state link excess fat intake to insulin resistance in both rodents and humans. J Clin Invest, 119(3), 573-81 (2009) doi:10.1172/JCI37048
18. D. J. Fazakerley, A. Y. Minard, J. R. Krycer, K. C. Thomas, J. Stöckli, D. J. Harney, J. G. Burchfield, G. J. Maghzal, S. T. Caldwell, R. C. Hartley, R. Stocker, M. P. Murphy and D. E. James: Mitochondrial oxidative stress causes insulin resistance without disrupting oxidative phosphorylation. J Biol Chem, 293(19), 7315-7328 (2018) doi:10.1074/jbc.RA117.001254
19. M. E. Lean, W. S. Leslie, A. C. Barnes, N. Brosnahan, G. Thom, L. McCombie, C. Peters, S. Zhyzhneuskaya, A. Al-Mrabeh, K. G. Hollingsworth, A. M. Rodrigues, L. Rehackova, A. J. Adamson, F. F. Sniehotta, J. C. Mathers, H. M. Ross, Y. McIlvenna, R. Stefanetti, M. Trenell, P. Welsh, S. Kean, I. Ford, A. McConnachie, N. Sattar and R. Taylor: Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet, 391(10120), 541-551 (2018) doi:10.1016/S0140-6736(17)33102-1
20. S. Juray, K. V. Axen and S. E. Trasino: Remission of Type 2 Diabetes with Very Low-Calorie Diets-A Narrative Review. Nutrients, 13(6) (2021) doi:10.3390/nu13062086
21. A. Maffettone, M. Rinaldi and A. Fontanella: Postprandial hyperglycemia: a new frontier in diabetes management? Italian Journal of Medicine, 12(2), 108-115 (2018) doi:10.4081/itjm.2018.961
22. B. Sottero, S. Gargiulo, I. Russo, C. Barale, G. Poli and F. Cavalot: Postprandial Dysmetabolism and Oxidative Stress in Type 2 Diabetes: Pathogenetic Mechanisms and Therapeutic Strategies. Med Res Rev, 35(5), 968-1031 (2015) doi:10.1002/med.21349
23. F. Cavalot, A. Petrelli, M. Traversa, K. Bonomo, E. Fiora, M. Conti, G. Anfossi, G. Costa and M. Trovati: Postprandial blood glucose is a stronger predictor of cardiovascular events than fasting blood glucose in type 2 diabetes mellitus, particularly in women: lessons from the San Luigi Gonzaga Diabetes Study. J Clin Endocrinol Metab, 91(3), 813-9 (2006) doi:10.1210/jc.2005-1005
24. F. Cavalot, A. Pagliarino, M. Valle, L. Di Martino, K. Bonomo, P. Massucco, G. Anfossi and M. Trovati: Postprandial blood glucose predicts cardiovascular events and all-cause mortality in type 2 diabetes in a 14-year follow-up: lessons from the San Luigi Gonzaga Diabetes Study. Diabetes Care, 34(10), 2237-43 (2011) doi:10.2337/dc10-2414
25. R. Singh, A. Barden, T. Mori and L. Beilin: Advanced glycation end-products: a review. Diabetologia, 44(2), 129-46 (2001) doi:10.1007/s001250051591
26. H. Vlassara and J. Uribarri: Advanced glycation end products (AGE) and diabetes: cause, effect, or both? Curr Diab Rep, 14(1), 453 (2014) doi:10.1007/s11892-013-0453-1
27. U. Greifenhagen, A. Frolov, M. Blüher and R. Hoffmann: Plasma Proteins Modified by Advanced Glycation End Products (AGEs) Reveal Site-specific Susceptibilities to Glycemic Control in Patients with Type 2 Diabetes. J Biol Chem, 291(18), 9610-6 (2016) doi:10.1074/jbc.M115.702860
28. K. Ando, M. Beppu, K. Kikugawa, R. Nagai and S. Horiuchi: Membrane proteins of human erythrocytes are modified by advanced glycation end products during aging in the circulation. Biochem Biophys Res Commun, 258(1), 123-7 (1999) doi:10.1006/bbrc.1999.0606
29. L. J. Yan: Redox imbalance stress in diabetes mellitus: Role of the polyol pathway. Animal Model Exp Med, 1(1), 7-13 (2018) doi:10.1002/ame2.12001
30. D. C. Pinto-Junior, K. S. Silva, M. L. Michalani, C. Y. Yonamine, J. V. Esteves, N. T. Fabre, K. Thieme, S. Catanozi, M. M. Okamoto, P. M. Seraphim, M. L. Corrêa-Giannella, M. Passarelli and U. F. Machado: Advanced glycation end products-induced insulin resistance involves repression of skeletal muscle GLUT4 expression. Sci Rep, 8(1), 8109 (2018) doi:10.1038/s41598-018-26482-6
31. G. Drews, P. Krippeit-Drews and M. Düfer: Oxidative stress and beta-cell dysfunction. Pflugers Arch, 460(4), 703-18 (2010) doi:10.1007/s00424-010-0862-9
32. A. Stirban, T. Gawlowski and M. Roden: Vascular effects of advanced glycation endproducts: Clinical effects and molecular mechanisms. Mol Metab, 3(2), 94-108 (2014) doi:10.1016/j.molmet.2013.11.006
33. E. Schleicher and U. Friess: Oxidative stress, AGE, and atherosclerosis. Kidney Int Suppl(106), S17-26 (2007) doi:10.1038/sj.ki.5002382
34. S. K. Powers, Z. Radak and L. L. Ji: Exercise-induced oxidative stress: past, present and future. J Physiol, 594(18), 5081-92 (2016) doi:10.1113/JP270646
35. M. Ristow, K. Zarse, A. Oberbach, N. Klöting, M. Birringer, M. Kiehntopf, M. Stumvoll, C. R. Kahn and M. Blüher: Antioxidants prevent health-promoting effects of physical exercise in humans. Proc Natl Acad Sci U S A, 106(21), 8665-70 (2009) doi:10.1073/pnas.0903485106
36. H. J. Woerle, C. Neumann, S. Zschau, S. Tenner, A. Irsigler, J. Schirra, J. E. Gerich and B. Göke: Impact of fasting and postprandial glycemia on overall glycemic control in type 2 diabetes Importance of postprandial glycemia to achieve target HbA1c levels. Diabetes Res Clin Pract, 77(2), 280-5 (2007) doi:10.1016/j.diabres.2006.11.011
37. H. P. Gunawardena, R. Silva, R. Sivakanesan, P. Ranasinghe and P. Katulanda: Poor Glycaemic Control Is Associated with Increased Lipid Peroxidation and Glutathione Peroxidase Activity in Type 2 Diabetes Patients. Oxid Med Cell Longev, 2019, 9471697 (2019) doi:10.1155/2019/9471697
38. S. R. Colberg, R. J. Sigal, J. E. Yardley, M. C. Riddell, D. W. Dunstan, P. C. Dempsey, E. S. Horton, K. Castorino and D. F. Tate: Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care, 39(11), 2065-2079 (2016) doi:10.2337/dc16-1728
39. J. W. van Dijk and L. J. van Loon: Exercise strategies to optimize glycemic control in type 2 diabetes: a continuing glucose monitoring perspective. Diabetes Spectr, 28(1), 24-31 (2015) doi:10.2337/diaspect.28.1.24
40. C. Velicer: https://thrivingschools.kaiserpermanente.org/kids-and-type-2-diabetes-how-parents-and-teachers-can-help-curb-the-tide/. In: Ed K. Permanente. (2016)
41. A. J. Buffey, M. P. Herring, C. K. Langley, A. E. Donnelly and B. P. Carson: The Acute Effects of Interrupting Prolonged Sitting Time in Adults with Standing and Light-Intensity Walking on Biomarkers of Cardiometabolic Health in Adults: A Systematic Review and Meta-analysis. Sports Med, 52(8), 1765-1787 (2022) doi:10.1007/s40279-022-01649-4
42. P. Singla, A. Bardoloi and A. A. Parkash: Metabolic effects of obesity: A review. World J Diabetes, 1(3), 76-88 (2010) doi:10.4239/wjd.v1.i3.76
43. T. Chang, H. Li, N. Zhang, X. Jiang, X. Yu, Q. Yang, Z. Jin, H. Meng and L. Chang: Highly integrated watch for noninvasive continual glucose monitoring. Microsyst Nanoeng, 8, 25 (2022) doi:10.1038/s41378-022-00355-5
44. C. Rodriguez-León, C. Villalonga, M. Munoz-Torres, J. R. Ruiz and O. Banos: Mobile and Wearable Technology for the Monitoring of Diabetes-Related Parameters: Systematic Review. JMIR Mhealth Uhealth, 9(6), e25138 (2021) doi:10.2196/25138
45. J. W. van Dijk, M. Venema, W. van Mechelen, C. D. Stehouwer, F. Hartgens and L. J. van Loon: Effect of moderate-intensity exercise versus activities of daily living on 24-hour blood glucose homeostasis in male patients with type 2 diabetes. Diabetes Care, 36(11), 3448-53 (2013) doi:10.2337/dc12-2620
46. M. Flores-Opazo, S. L. McGee and M. Hargreaves: Exercise and GLUT4. Exerc Sport Sci Rev, 48(3), 110-118 (2020) doi:10.1249/JES.0000000000000224
47. E. A. Richter and M. Hargreaves: Exercise, GLUT4, and skeletal muscle glucose uptake. Physiol Rev, 93(3), 993-1017 (2013) doi:10.1152/physrev.00038.2012
48. G. N. Kraniou, D. Cameron-Smith and M. Hargreaves: Acute exercise and GLUT4 expression in human skeletal muscle: influence of exercise intensity. J Appl Physiol (1985), 101(3), 934-7 (2006) doi:10.1152/japplphysiol.01489.2005
49. T. Kawamura and I. Muraoka: Exercise-Induced Oxidative Stress and the Effects of Antioxidant Intake from a Physiological Viewpoint. Antioxidants (Basel), 7(9) (2018) doi:10.3390/antiox7090119
50. J. Quindry, W. Stone, J. King and C. Broeder: The effects of acute exercise on neutrophils and plasma oxidative stress. Med Sci Sports Exerc, 35(7), 1139-45 (2003)
51. S. K. Powers, R. Deminice, M. Ozdemir, T. Yoshihara, M. P. Bomkamp and H. Hyatt: Exercise-induced oxidative stress: Friend or foe? J Sport Health Sci, 9(5), 415-425 (2020) doi:10.1016/j.jshs.2020.04.001
52. V. J. Thannickal and B. L. Fanburg: Reactive oxygen species in cell signaling. Am J Physiol Lung Cell Mol Physiol, 279(6), L1005-28 (2000) doi:10.1152/ajplung.2000.279.6.L1005
53. J. T. Hancock, R. Desikan and S. J. Neill: Role of reactive oxygen species in cell signalling pathways. Biochem Soc Trans, 29(Pt 2), 345-50 (2001) doi:10.1042/0300-5127:0290345
54. J. N. Cobley, H. McHardy, J. P. Morton, M. G. Nikolaidis and G. L. Close: Influence of vitamin C and vitamin E on redox signaling: Implications for exercise adaptations. Free Radic Biol Med, 84, 65-76 (2015) doi:10.1016/j.freeradbiomed.2015.03.018
55. M. B. Reid: Nitric oxide, reactive oxygen species, and skeletal muscle contraction. Med Sci Sports Exerc, 33(3), 371-6 (2001) doi:10.1097/00005768-200103000-00006
56. F. He, J. Li, Z. Liu, C. C. Chuang, W. Yang and L. Zuo: Redox Mechanism of Reactive Oxygen Species in Exercise. Front Physiol, 7, 486 (2016) doi:10.3389/fphys.2016.00486
57. L. L. Ji: Antioxidant enzyme response to exercise and aging. Med Sci Sports Exerc, 25(2), 225-31 (1993)
58. K. J. Lipska: Patient education: Exercise and medical care for people with type 2 diabetes (Beyond the Basics), www.uptodate.com/contents/exercise-and-medical-care-for-people-with-type-2-diabetes-beyond-the-basics. In: UpToDate. UptoDate, (2023)
59. D. Khandelwal, D. Dutta, S. Chittawar and S. Kalra: Sleep Disorders in Type 2 Diabetes. Indian J Endocrinol Metab, 21(5), 758-761 (2017) doi:10.4103/ijem.IJEM_156_17
60. S. J. Kelly and M. Ismail: Stress and type 2 diabetes: a review of how stress contributes to the development of type 2 diabetes. Annu Rev Public Health, 36, 441-62 (2015) doi:10.1146/annurev-publhealth-031914-122921
61. F. Atrooz and S. Salim: Sleep deprivation, oxidative stress and inflammation. Adv Protein Chem Struct Biol, 119, 309-336 (2020) doi:10.1016/bs.apcsb.2019.03.001
62. V. M. Hill, R. M. O'Connor, G. B. Sissoko, I. S. Irobunda, S. Leong, J. C. Canman, N. Stavropoulos and M. Shirasu-Hiza: A bidirectional relationship between sleep and oxidative stress in Drosophila. PLoS Biol, 16(7), e2005206 (2018) doi:10.1371/journal.pbio.2005206
63. P. Moller, H. Wallin and L. E. Knudsen: Oxidative stress associated with exercise, psychological stress and life-style factors. Chem Biol Interact, 102 http://biomednet.com/db/medline/96424598(1), 17-36 (1996)
64. E. Belaïdi: Oxidative Stress and Sleep Disorders, https://www.mdpi.com/journal/antioxidants/special_issues/Oxidative_Stress_and_Sleep_Disorders. In: Health Outcomes of Antioxidants and Oxidative Stress. Antioxidants, (2022)
65. C. Lauridsen and S. K. Jensen: α-Tocopherol incorporation in mitochondria and microsomes upon supranutritional vitamin E supplementation. Genes Nutr, 7(4), 475-82 (2012) doi:10.1007/s12263-012-0286-6
66. C. K. Sen, S. Khanna and S. Roy: Tocotrienols in health and disease: the other half of the natural vitamin E family. Mol Aspects Med, 28(5-6), 692-728 (2007) doi:10.1016/j.mam.2007.03.001
67. A. Azzi, R. Gysin, P. Kempna, A. Munteanu, Y. Negis, L. Villacorta, T. Visarius and J. M. Zingg: Vitamin E mediates cell signaling and regulation of gene expression. Ann N Y Acad Sci, 1031, 86-95 (2004)
68. J. M. Zingg: Vitamin E: A Role in Signal Transduction. Annu Rev Nutr, 35, 135-73 (2015) doi:10.1146/annurev-nutr-071714-034347
69. M. E. Balbi, F. S. Tonin, A. M. Mendes, H. H. Borba, A. Wiens, F. Fernandez-Llimos and R. Pontarolo: Antioxidant effects of vitamins in type 2 diabetes: a meta-analysis of randomized controlled trials. Diabetol Metab Syndr, 10, 18 (2018) doi:10.1186/s13098-018-0318-5
70. C. K. Chow, W. Ibrahim, Z. Wei and A. C. Chan: Vitamin E regulates mitochondrial hydrogen peroxide generation. Free Radic Biol Med, 27(5-6), 580-7 (1999) doi:10.1016/s0891-5849(99)00121-5
71. A. A. El-Aal, E. A. A. El-Ghffar, A. A. Ghali, M. R. Zughbur and M. M. Sirdah: The effect of vitamin C and/or E supplementations on type 2 diabetic adult males under metformin treatment: A single-blinded randomized controlled clinical trial. Diabetes Metab Syndr, 12(4), 483-489 (2018) doi:10.1016/j.dsx.2018.03.013
72. M. Vafa, N. Haghighat, N. Moslehi, S. Eghtesadi and I. Heydari: Effect of Tocotrienols enriched canola oil on glycemic control and oxidative status in patients with type 2 diabetes mellitus: A randomized double-blind placebo-controlled clinical trial. J Res Med Sci, 20(6), 540-7 (2015) doi:10.4103/1735-1995.165945
73. S. Baliarsingh, Z. H. Beg and J. Ahmad: The therapeutic impacts of tocotrienols in type 2 diabetic patients with hyperlipidemia. Atherosclerosis, 182(2), 367-374 (2005) doi:10.1016/j.atherosclerosis.2005.02.020
74. J. I. Ho, E. Y. Ng, Y. Chiew, Y. Y. Koay, P. F. Chuar, S. C. W. Phang, B. Ahmad and K. A. Kadir: The effects of vitamin E on non-proliferative diabetic retinopathy in type 2 diabetes mellitus: Are they sustainable with 12 months of therapy. SAGE Open Med, 10, 20503121221095324 (2022) doi:10.1177/20503121221095324
75. K. Kalvaitus and S. A. Portnoy: https://www.healio.com/news/endocrinology/20120325/experts-recommend-two-pronged-approach-to-treating-prediabetes. In: Endrocrine Today. (2010)
76. F. Suleman, D. A. Khan, M. A. Pervez and M. Aamir: Effects of delta-tocotrienol supplementation on glycaemic control in individuals with prediabetes: A randomized controlled study. J Pak Med Assoc, 72(1), 4-7 (2022) doi:10.47391/JPMA.966
77. F. Fang, Z. Kang and C. Wong: Vitamin E tocotrienols improve insulin sensitivity through activating peroxisome proliferator-activated receptors. Molecular nutrition & food research, 54(3), 345-352 (2010) doi:10.1002/mnfr.200900119
78. S. A. Mason, L. Parker, P. van der Pligt and G. D. Wadley: Vitamin C supplementation for diabetes management: A comprehensive narrative review. Free Radic Biol Med, 194, 255-283 (2023) doi:10.1016/j.freeradbiomed.2022.12.003
79. H. Sun, J. Karp, K. M. Sun and C. M. Weaver: Decreasing Vitamin C Intake, Low Serum Vitamin C Level and Risk for US Adults with Diabetes. Nutrients, 14(19) (2022) doi:10.3390/nu14193902
80. M. Liu and S. Park: A Causal Relationship between Vitamin C Intake with Hyperglycemia and Metabolic Syndrome Risk: A Two-Sample Mendelian Randomization Study. Antioxidants (Basel), 11(5) (2022) doi:10.3390/antiox11050857
81. I. Ebenuwa, P. C. Violet, S. Padayatty, Y. Wang, H. Sun, P. Adhikari, S. Smith, H. Tu, M. Niyyati, K. Wilkins and M. Levine: Abnormal urinary loss of vitamin C in diabetes: prevalence and clinical characteristics of a vitamin C renal leak. Am J Clin Nutr, 116(1), 274-284 (2022) doi:10.1093/ajcn/nqac063
82. L. Shi, X. Du, P. Guo, L. Huang, P. Qi and Q. Gong: Ascorbic acid supplementation in type 2 diabetes mellitus: A protocol for systematic review and meta-analysis. Medicine (Baltimore), 99(45), e23125 (2020) doi:10.1097/MD.0000000000023125
83. S. A. Mason, M. A. Keske and G. D. Wadley: Effects of Vitamin C Supplementation on Glycemic Control and Cardiovascular Risk Factors in People With Type 2 Diabetes: A GRADE-Assessed Systematic Review and Meta-analysis of Randomized Controlled Trials. Diabetes Care, 44(2), 618-630 (2021) doi:10.2337/dc20-1893
84. C. L. Jiang, C. Y. Tsao and Y. C. Lee: Vitamin C attenuates predisposition to high-fat diet-induced metabolic dysregulation in GLUT10-deficient mouse model. Genes Nutr, 17(1), 10 (2022) doi:10.1186/s12263-022-00713-y
85. R. Wilson, J. Willis, R. Gearry, P. Skidmore, E. Fleming, C. Frampton and A. Carr: Inadequate Vitamin C Status in Prediabetes and Type 2 Diabetes Mellitus: Associations with Glycaemic Control, Obesity, and Smoking. Nutrients, 9(9) (2017) doi:10.3390/nu9090997
86. J. Stanimirovic, J. Radovanovic, K. Banjac, M. Obradovic, M. Essack, S. Zafirovic, Z. Gluvic, T. Gojobori and E. R. Isenovic: Role of C-Reactive Protein in Diabetic Inflammation. Mediators Inflamm, 2022, 3706508 (2022) doi:10.1155/2022/3706508
87. M. Valko, M. Izakovic, M. Mazur, C. J. Rhodes and J. Telser: Role of oxygen radicals in DNA damage and cancer incidence. Mol Cell Biochem, 266(1-2), 37-56 (2004) doi:10.1023/b:mcbi.0000049134.69131.89
88. K. C. Sagun, J. M. Cárcamo and D. W. Golde: Vitamin C enters mitochondria via facilitative glucose transporter 1 (Glut1) and confers mitochondrial protection against oxidative injury. FASEB J, 19(12), 1657-67 (2005) doi:10.1096/fj.05-4107com
89. A. Bansal and C. P. Hadimani: Low Plasma Ascorbate Levels in Type 2 Diabetic Patients With Adequate Dietary Vitamin C. J Lab Physicians, 13(2), 139-143 (2021) doi:10.1055/s-0041-1730751
90. A. J. Sinclair, P. B. Taylor, J. Lunec, A. J. Girling and A. H. Barnett: Low plasma ascorbate levels in patients with type 2 diabetes mellitus consuming adequate dietary vitamin C. Diabet Med, 11(9), 893-8 (1994) doi:10.1111/j.1464-5491.1994.tb00375.x
91. H. Chen, R. J. Karne, G. Hall, U. Campia, J. A. Panza, R. O. Cannon, Y. Wang, A. Katz, M. Levine and M. J. Quon: High-dose oral vitamin C partially replenishes vitamin C levels in patients with Type 2 diabetes and low vitamin C levels but does not improve endothelial dysfunction or insulin resistance. Am J Physiol Heart Circ Physiol, 290(1), H137-45 (2006) doi:10.1152/ajpheart.00768.2005
92. R. Bonner, O. Albajrami, J. Hudspeth and A. Upadhyay: Diabetic Kidney Disease. Prim Care, 47(4), 645-659 (2020) doi:10.1016/j.pop.2020.08.004
93. M. Afkhami-Ardekani and A. Shojaoddiny-Ardekani: Effect of vitamin C on blood glucose, serum lipids & serum insulin in type 2 diabetes patients. Indian J Med Res., 126(5), 471-474. (2007)
94. A. S. Donin, J. E. Dent, C. M. Nightingale, N. Sattar, C. G. Owen, A. R. Rudnicka, M. R. Perkin, A. M. Stephen, S. A. Jebb, D. G. Cook and P. H. Whincup: Fruit, vegetable and vitamin C intakes and plasma vitamin C: cross-sectional associations with insulin resistance and glycaemia in 9-10 year-old children. Diabet Med, 33(3), 307-15 (2016) doi:10.1111/dme.13006
95. S. Parajuli, G. Jasmin, H. Sirak, A. F. Lee and B. U. Nwosu: Prediabetes: Adherence to Nutrition Visits Decreases HbA1c in Children and Adolescents. Front Endocrinol (Lausanne), 13, 916785 (2022) doi:10.3389/fendo.2022.916785
96. J. J. Strain and C. W. Mulholland: Vitamin C and vitamin E--synergistic interactions in vivo? EXS, 62, 419-22 (1992) doi:10.1007/978-3-0348-7460-1_40
97. A. Azzi: Tocopherols, tocotrienols and tocomonoenols: Many similar molecules but only one vitamin E. Redox Biol, 26, 101259 (2019) doi:10.1016/j.redox.2019.101259
98. L. Pangrazzi, L. Balasco and Y. Bozzi: Natural Antioxidants: A Novel Therapeutic Approach to Autism Spectrum Disorders? Antioxidants (Basel), 9(12) (2020) doi:10.3390/antiox9121186
99. G. R. Buettner: The pecking order of free radicals and antioxidants: lipid peroxidation, alpha-tocopherol, and ascorbate. Arch Biochem Biophys, 300(2), 535-43 (1993) doi:10.1006/abbi.1993.1074
100. A. Ayala, M. F. Muñoz and S. Argüelles: Lipid peroxidation: production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxid Med Cell Longev, 2014, 360438 (2014) doi:10.1155/2014/360438
101. A. de Souza Bastos, D. T. Graves, A. P. de Melo Loureiro, C. R. Júnior, S. C. T. Corbi, F. Frizzera, R. M. Scarel-Caminaga, N. O. Câmara, O. M. Andriankaja, M. I. Hiyane and S. R. P. Orrico: Diabetes and increased lipid peroxidation are associated with systemic inflammation even in well-controlled patients. J Diabetes Complications, 30(8), 1593-1599 (2016) doi:10.1016/j.jdiacomp.2016.07.011
102. J. Augustine, E. P. Troendle, P. Barabas, C. A. McAleese, T. Friedel, A. W. Stitt and T. M. Curtis: The Role of Lipoxidation in the Pathogenesis of Diabetic Retinopathy. Front Endocrinol (Lausanne), 11, 621938 (2020) doi:10.3389/fendo.2020.621938
103. A. Sato, Y. Takino, T. Yano, K. Fukui and A. Ishigami: Determination of tissue-specific interaction between vitamin C and vitamin E. Br J Nutr, 128(6), 993-1003 (2022) doi:10.1017/S0007114521004384
104. E. Porkkala-Sarataho, J. T. Salonen, K. Nyyssönen, J. Kaikkonen, R. Salonen, U. Ristonmaa, U. Diczfalusy, R. Brigelius-Flohe, S. Loft and H. E. Poulsen: Long-term effects of vitamin E, vitamin C, and combined supplementation on urinary 7-hydro-8-oxo-2'-deoxyguanosine, serum cholesterol oxidation products, and oxidation resistance of lipids in nondepleted men. Arterioscler Thromb Vasc Biol, 20(9), 2087-93 (2000) doi:10.1161/01.atv.20.9.2087
105. H. Y. Huang, L. J. Appel, K. D. Croft, E. R. Miller, T. A. Mori and I. B. Puddey: Effects of vitamin C and vitamin E on in vivo lipid peroxidation: results of a randomized controlled trial. Am J Clin Nutr, 76(3), 549-55 (2002) doi:10.1093/ajcn/76.3.549
106. Z. Mazloom, N. Hejazi, M. H. Dabbaghmanesh, H. R. Tabatabaei, A. Ahmadi and H. Ansar: Effect of vitamin C supplementation on postprandial oxidative stress and lipid profile in type 2 diabetic patients. Pak J Biol Sci, 14(19), 900-4 (2011) doi:10.3923/pjbs.2011.900.904
107. S. Neri, S. Calvagno, B. Mauceri, M. Misseri, A. Tsami, C. Vecchio, G. Mastrosimone, A. Di Pino, D. Maiorca, A. Judica, G. Romano, A. Rizzotto and S. S. Signorelli: Effects of antioxidants on postprandial oxidative stress and endothelial dysfunction in subjects with impaired glucose tolerance and type 2 diabetes. Eur J Nutr, 49(7), 409-16 (2010) doi:10.1007/s00394-010-0099-6
108. A. K. Holley, V. Bakthavatchalu, J. M. Velez-Roman and D. K. St Clair: Manganese superoxide dismutase: guardian of the powerhouse. Int J Mol Sci, 12(10), 7114-62 (2011) doi:10.3390/ijms12107114
109. S. H. Lee, H. A. Jouihan, R. C. Cooksey, D. Jones, H. J. Kim, D. R. Winge and D. A. McClain: Manganese supplementation protects against diet-induced diabetes in wild type mice by enhancing insulin secretion. Endocrinology, 154(3), 1029-38 (2013) doi:10.1210/en.2012-1445
110. E. Burlet and S. K. Jain: Manganese supplementation reduces high glucose-induced monocyte adhesion to endothelial cells and endothelial dysfunction in Zucker diabetic fatty rats. J Biol Chem, 288(9), 6409-16 (2013) doi:10.1074/jbc.M112.447805
111. S. Du, X. Wu, T. Han, W. Duan, L. Liu, J. Qi, Y. Niu, L. Na and C. Sun: Dietary manganese and type 2 diabetes mellitus: two prospective cohort studies in China. Diabetologia, 61(9), 1985-1995 (2018) doi:10.1007/s00125-018-4674-3
112. X. Wang, M. Zhang, G. Lui, H. Chang, W. Liu, Z. Li, Y. Liu and G. Huang: Associations of Serum Manganese Levels with Prediabetes and Diabetes among ≥60-Year-Old Chinese Adults: A Population-Based Cross-Sectional Analysis. Nutrients, 8(8) (2016) doi:10.3390/nu8080497
113. H. Chen, Z. Cui, W. Lu, P. Wang, J. Wang, Z. Zhou, N. Zhang, Z. Wang, T. Lin, Y. Song, L. Liu, X. Huang, P. Chen, G. Tang, Y. Duan, B. Wang, H. Zhang, X. Xu, Y. Yang, X. Qin and F. Song: Association between serum manganese levels and diabetes in Chinese adults with hypertension. J Clin Hypertens (Greenwich), 24(7), 918-927 (2022) doi:10.1111/jch.14520
114. N. van der Schaft, J. D. Schoufour, J. Nano, J. C. Kiefte-de Jong, T. Muka, E. J. G. Sijbrands, M. A. Ikram, O. H. Franco and T. Voortman: Dietary antioxidant capacity and risk of type 2 diabetes mellitus, prediabetes and insulin resistance: the Rotterdam Study. Eur J Epidemiol, 34(9), 853-861 (2019) doi:10.1007/s10654-019-00548-9
115. R. Brigelius-Flohé and L. Flohé: Regulatory Phenomena in the Glutathione Peroxidase Superfamily. Antioxid Redox Signal, 33(7), 498-516 (2020) doi:10.1089/ars.2019.7905
116. M. L. Katz, W. L. Stone and E. A. Dratz: Fluorescent pigment accumulation in retinal pigment epithelium of antioxidant-deficient rats. Investigative ophthalmology & visual science, 17(11), 1049-1058 (1978)
117. A. N. Ogawa-Wong, M. J. Berry and L. A. Seale: Selenium and Metabolic Disorders: An Emphasis on Type 2 Diabetes Risk. Nutrients, 8(2), 80 (2016) doi:10.3390/nu8020080
118. G. Marcelino, D. J. Machate, K. C. Freitas, P. A. Hiane, I. R. Maldonade, A. Pott, M. A. Asato, C. J. Candido and R. C. A. Guimarães: β-Carotene: Preventive Role for Type 2 Diabetes Mellitus and Obesity: A Review. Molecules, 25(24) (2020) doi:10.3390/molecules25245803
119. Y. W. Jiang, Z. H. Sun, W. W. Tong, K. Yang, K. Q. Guo, G. Liu and A. Pan: Dietary Intake and Circulating Concentrations of Carotenoids and Risk of Type 2 Diabetes: A Dose-Response Meta-Analysis of Prospective Observational Studies. Adv Nutr, 12(5), 1723-1733 (2021) doi:10.1093/advances/nmab048
120. A. A. o. Pediatrics: https://www.aap.org/en/practice-management/bright-futures/bright-futures-materials-and-tools/bright-futures-guidelines-and-pocket-guide/. In: Ed J. Joseph F. Hagan, Judith S. Shaw, and Paula M. Duncan. (2022)
121. W. T. B. Eddolls, M. A. McNarry, G. Stratton, C. O. N. Winn and K. A. Mackintosh: High-Intensity Interval Training Interventions in Children and Adolescents: A Systematic Review. Sports Med, 47(11), 2363-2374 (2017) doi:10.1007/s40279-017-0753-8
References
- Diabetes. Available online: https://www.who.int/news-room/fact-sheets/detail/diabetes (accessed on 12 July 2022).
- Chen, L.; Magliano, D.J.; Zimmet, P.Z. The worldwide epidemiology of type 2 diabetes mellitus—Present and future perspectives. Nat. Rev. Endocrinol. 2011, 8, 228–236. https://doi.org/10.1038/nrendo.2011.183.
- Liu, J.; Li, Y.; Zhang, D.; Yi, S.S. Trends in Prediabetes Among Youths in the US From 1999 Through 2018. JAMA Pediatr. 2022, 176, 608–611. https://doi.org/10.1001/jamapediatrics.2022.0077.
- How Type 2 Diabetes Affects Your Workforce. Available online: https://www.cdc.gov/diabetes/prevention/how-type2-affects-workforce.htm#:~:text=Diabetes%20Is%20Costly,over%20a%205%2Dyear%20period (accessed on 13 July 2022).
- Davidson, K.W.; Barry, M.J.; Mangione, C.M.; Cabana, M.; Caughey, A.B.; Davis, E.M.; Donahue, K.E.; Doubeni, C.A.; Krist, A.H.; Kubik, M.; et al. Screening for Prediabetes and Type 2 Diabetes: US Preventive Services Task Force Recommendation Statement. JAMA 2021, 326, 736–743. https://doi.org/10.1001/jama.2021.12531.
- Prevalence of Both Diagnosed and Undiagnosed Diabetes. Available online: https://www.cdc.gov/diabetes/data/statistics-report/diagnosed-undiagnosed-diabetes.html (accessed on 22 May 2023).
- Reinehr, T. Type 2 diabetes mellitus in children and adolescents. World J. Diabetes 2013, 4, 270–281. https://doi.org/10.4239/wjd.v4.i6.270.
- Pansier, B.; Schulz, P.J. School-based diabetes interventions and their outcomes: A systematic literature review. J. Public Health Res. 2015, 4, 467. https://doi.org/10.4081/jphr.2015.467.
- Alu, S.N.; Los, E.A.; Ford, G.A.; Stone, W.L. Oxidative Stress in Type 2 Diabetes: The Case for Future Pediatric Redoxomics Studies. Antioxidants 2022, 11, 1336.
- Garber, A.J.; Abrahamson, M.J.; Barzilay, J.I.; Blonde, L.; Bloomgarden, Z.T.; Bush, M.A.; Dagogo-Jack, S.; DeFronzo, R.A.; Einhorn, D.; Fonseca, V.A.; et al. Consensus statement by the american association of clinical endocrinologists and american college of endocrinology on the comprehensive type 2 diabetes management algorithm-2018 executive summary. Endocr. Pract. 2018, 24, 91–120. https://doi.org/10.4158/CS-2017-0153.
- Mechanick, J.I.; Garber, A.J.; Grunberger, G.; Handelsman, Y.; Garvey, W.T. Dysglycemia-based chronic disease: An american association of clinical endocrinologists position statement. Endocr Pract. 2018, 24, 995–1011. https://doi.org/10.4158/PS-2018-0139.
- Hansen, T. Type 2 diabetes mellitus--a multifactorial disease. Ann. Univ. Mariae Curie Sklodowska Med. 2002, 57, 544–549.
- Wright, E.; Scism-Bacon, J.L.; Glass, L.C. Oxidative stress in type 2 diabetes: The role of fasting and postprandial glycaemia. Int J. Clin. Pract. 2006, 60, 308–314. https://doi.org/10.1111/j.1368-5031.2006.00825.x.
- Chikezie, P.C.; Ojiako, O.A.; Ogbuji, A.C. Oxidative Stress in Diabetes Mellitus. Int. J. Biol. Chem. 2015, 9, 92–109. https://doi.org/10.3923/ijbc.2015.92.109.
- DeFronzo, R.A.; Tripathy, D. Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care 2009, 32 (Suppl 2), S157–S163. https://doi.org/10.2337/dc09-S302.
- Mueckler, M. Insulin resistance and the disruption of Glut4 trafficking in skeletal muscle. J. Clin. Investig. 2001, 107, 1211–1213. https://doi.org/10.1172/JCI13020.
- Maier, V.H.; Gould, G.W. Long-term insulin treatment of 3T3-L1 adipocytes results in mis-targeting of GLUT4: Implications for insulin-stimulated glucose transport. Diabetologia 2000, 43, 1273–1281. https://doi.org/10.1007/s001250051523.
- Kampmann, U.; Christensen, B.; Nielsen, T.S.; Pedersen, S.B.; Ørskov, L.; Lund, S.; Møller, N.; Jessen, N. GLUT4 and UBC9 protein expression is reduced in muscle from type 2 diabetic patients with severe insulin resistance. PLoS ONE 2011, 6, e27854. https://doi.org/10.1371/journal.pone.0027854.
- Anderson, E.J.; Lustig, M.E.; Boyle, K.E.; Woodlief, T.L.; Kane, D.A.; Lin, C.T.; Price, J.W.; Kang, L.; Rabinovitch, P.S.; Szeto, H.H.; et al. Mitochondrial H2O2 emission and cellular redox state link excess fat intake to insulin resistance in both rodents and humans. J. Clin. Investig. 2009, 119, 573–581. https://doi.org/10.1172/JCI37048.
- Fazakerley, D.J.; Minard, A.Y.; Krycer, J.R.; Thomas, K.C.; Stöckli, J.; Harney, D.J.; Burchfield, J.G.; Maghzal, G.J.; Caldwell, S.T.; Hartley, R.C.; et al. Mitochondrial oxidative stress causes insulin resistance without disrupting oxidative phosphorylation. J. Biol. Chem. 2018, 293, 7315–7328. https://doi.org/10.1074/jbc.RA117.001254.
- Lean, M.E.; Leslie, W.S.; Barnes, A.C.; Brosnahan, N.; Thom, G.; McCombie, L.; Peters, C.; Zhyzhneuskaya, S.; Al-Mrabeh, A.; Hollingsworth, K.G.; et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): An open-label, cluster-randomised trial. Lancet 2018, 391, 541–551. https://doi.org/10.1016/S0140-6736(17)33102-1.
- Juray, S.; Axen, K.V.; Trasino, S.E. Remission of Type 2 Diabetes with Very Low-Calorie Diets-A Narrative Review. Nutrients 2021, 13, 2086. https://doi.org/10.3390/nu13062086.
- Maffettone, A.; Rinaldi, M.; Fontanella, A. Postprandial hyperglycemia: A new frontier in diabetes management? Ital. J. Med. 2018, 12, 108–115. https://doi.org/10.4081/itjm.2018.961.
- Sottero, B.; Gargiulo, S.; Russo, I.; Barale, C.; Poli, G.; Cavalot, F. Postprandial Dysmetabolism and Oxidative Stress in Type 2 Diabetes: Pathogenetic Mechanisms and Therapeutic Strategies. Med. Res. Rev. 2015, 35, 968–1031. https://doi.org/10.1002/med.21349.
- Cavalot, F.; Petrelli, A.; Traversa, M.; Bonomo, K.; Fiora, E.; Conti, M.; Anfossi, G.; Costa, G.; Trovati, M. Postprandial blood glucose is a stronger predictor of cardiovascular events than fasting blood glucose in type 2 diabetes mellitus, particularly in women: Lessons from the San Luigi Gonzaga Diabetes Study. J. Clin. Endocrinol. Metab. 2006, 91, 813–819. https://doi.org/10.1210/jc.2005-1005.
- Cavalot, F.; Pagliarino, A.; Valle, M.; Di Martino, L.; Bonomo, K.; Massucco, P.; Anfossi, G.; Trovati, M. Postprandial blood glucose predicts cardiovascular events and all-cause mortality in type 2 diabetes in a 14-year follow-up: Lessons from the San Luigi Gonzaga Diabetes Study. Diabetes Care 2011, 34, 2237–2243. https://doi.org/10.2337/dc10-2414.
- Singh, R.; Barden, A.; Mori, T.; Beilin, L. Advanced glycation end-products: A review. Diabetologia 2001, 44, 129–146. https://doi.org/10.1007/s001250051591.
- Vlassara, H.; Uribarri, J. Advanced glycation end products (AGE) and diabetes: Cause, effect, or both? Curr. Diab. Rep. 2014, 14, 453. https://doi.org/10.1007/s11892-013-0453-1.
- Greifenhagen, U.; Frolov, A.; Blüher, M.; Hoffmann, R. Plasma Proteins Modified by Advanced Glycation End Products (AGEs) Reveal Site-specific Susceptibilities to Glycemic Control in Patients with Type 2 Diabetes. J. Biol. Chem. 2016, 291, 9610–9616. https://doi.org/10.1074/jbc.M115.702860.
- Ando, K.; Beppu, M.; Kikugawa, K.; Nagai, R.; Horiuchi, S. Membrane proteins of human erythrocytes are modified by advanced glycation end products during aging in the circulation. Biochem. Biophys. Res. Commun. 1999, 258, 123–127. https://doi.org/10.1006/bbrc.1999.0606.
- Yan, L.J. Redox imbalance stress in diabetes mellitus: Role of the polyol pathway. Anim. Model Exp. Med. 2018, 1, 7–13. https://doi.org/10.1002/ame2.12001.
- Pinto-Junior, D.C.; Silva, K.S.; Michalani, M.L.; Yonamine, C.Y.; Esteves, J.V.; Fabre, N.T.; Thieme, K.; Catanozi, S.; Okamoto, M.M.; Seraphim, P.M.; et al. Advanced glycation end products-induced insulin resistance involves repression of skeletal muscle GLUT4 expression. Sci. Rep. 2018, 8, 8109. https://doi.org/10.1038/s41598-018-26482-6.
- Drews, G.; Krippeit-Drews, P.; Düfer, M. Oxidative stress and beta-cell dysfunction. Pflug. Arch. 2010, 460, 703–718. https://doi.org/10.1007/s00424-010-0862-9.
- Stirban, A.; Gawlowski, T.; Roden, M. Vascular effects of advanced glycation endproducts: Clinical effects and molecular mechanisms. Mol. Metab. 2014, 3, 94–108. https://doi.org/10.1016/j.molmet.2013.11.006.
- Schleicher, E.; Friess, U. Oxidative stress, AGE, and atherosclerosis. Kidney Int. Suppl. 2007, 72, S17–S26. https://doi.org/10.1038/sj.ki.5002382.
- Powers, S.K.; Radak, Z.; Ji, L.L. Exercise-induced oxidative stress: Past, present and future. J. Physiol. 2016, 594, 5081–5092. https://doi.org/10.1113/JP270646.
- Ristow, M.; Zarse, K.; Oberbach, A.; Klöting, N.; Birringer, M.; Kiehntopf, M.; Stumvoll, M.; Kahn, C.R.; Blüher, M. Antioxidants prevent health-promoting effects of physical exercise in humans. Proc. Natl. Acad. Sci. USA 2009, 106, 8665–8670. https://doi.org/10.1073/pnas.0903485106.
- Woerle, H.J.; Neumann, C.; Zschau, S.; Tenner, S.; Irsigler, A.; Schirra, J.; Gerich, J.E.; Göke, B. Impact of fasting and postprandial glycemia on overall glycemic control in type 2 diabetes Importance of postprandial glycemia to achieve target HbA1c levels. Diabetes Res. Clin. Pract. 2007, 77, 280–285. https://doi.org/10.1016/j.diabres.2006.11.011.
- Gunawardena, H.P.; Silva, R.; Sivakanesan, R.; Ranasinghe, P.; Katulanda, P. Poor Glycaemic Control Is Associated with Increased Lipid Peroxidation and Glutathione Peroxidase Activity in Type 2 Diabetes Patients. Oxid. Med. Cell Longev. 2019, 2019, 9471697. https://doi.org/10.1155/2019/9471697.
- Colberg, S.R.; Sigal, R.J.; Yardley, J.E.; Riddell, M.C.; Dunstan, D.W.; Dempsey, P.C.; Horton, E.S.; Castorino, K.; Tate, D.F. Physical Activity/Exercise and Diabetes: A Position Statement of the American Diabetes Association. Diabetes Care 2016, 39, 2065–2079. https://doi.org/10.2337/dc16-1728.
- van Dijk, J.W.; van Loon, L.J. Exercise strategies to optimize glycemic control in type 2 diabetes: A continuing glucose monitoring perspective. Diabetes Spectr. 2015, 28, 24–31. https://doi.org/10.2337/diaspect.28.1.24.
- Velicer, C. Available online: https://thrivingschools.kaiserpermanente.org/kids-and-type-2-diabetes-how-parents-and-teachers-can-help-curb-the-tide/ (accessed on 13 September 2022).
- Buffey, A.J.; Herring, M.P.; Langley, C.K.; Donnelly, A.E.; Carson, B.P. The Acute Effects of Interrupting Prolonged Sitting Time in Adults with Standing and Light-Intensity Walking on Biomarkers of Cardiometabolic Health in Adults: A Systematic Review and Meta-analysis. Sport. Med. 2022, 52, 1765–1787. https://doi.org/10.1007/s40279-022-01649-4.
- Singla, P.; Bardoloi, A.; Parkash, A.A. Metabolic effects of obesity: A review. World J. Diabetes 2010, 1, 76–88. https://doi.org/10.4239/wjd.v1.i3.76.
- Chang, T.; Li, H.; Zhang, N.; Jiang, X.; Yu, X.; Yang, Q.; Jin, Z.; Meng, H.; Chang, L. Highly integrated watch for noninvasive continual glucose monitoring. Microsyst. Nanoeng. 2022, 8, 25. https://doi.org/10.1038/s41378-022-00355-5.
- Rodriguez-León, C.; Villalonga, C.; Munoz-Torres, M.; Ruiz, J.R.; Banos, O. Mobile and Wearable Technology for the Monitoring of Diabetes-Related Parameters: Systematic Review. JMIR Mhealth Uhealth 2021, 9, e25138. https://doi.org/10.2196/25138.
- Van Dijk, J.W.; Venema, M.; van Mechelen, W.; Stehouwer, C.D.; Hartgens, F.; van Loon, L.J. Effect of moderate-intensity exercise versus activities of daily living on 24-hour blood glucose homeostasis in male patients with type 2 diabetes. Diabetes Care 2013, 36, 3448–3453. https://doi.org/10.2337/dc12-2620.
- Flores-Opazo, M.; McGee, S.L.; Hargreaves, M. Exercise and GLUT4. Exerc. Sport Sci. Rev. 2020, 48, 110–118. https://doi.org/10.1249/JES.0000000000000224.
- Richter, E.A.; Hargreaves, M. Exercise, GLUT4, and skeletal muscle glucose uptake. Physiol. Rev. 2013, 93, 993–1017. https://doi.org/10.1152/physrev.00038.2012.
- Kraniou, G.N.; Cameron-Smith, D.; Hargreaves, M. Acute exercise and GLUT4 expression in human skeletal muscle: Influence of exercise intensity. J. Appl. Physiol. 2006, 101, 934–937. https://doi.org/10.1152/japplphysiol.01489.2005.
- Kawamura, T.; Muraoka, I. Exercise-Induced Oxidative Stress and the Effects of Antioxidant Intake from a Physiological Viewpoint. Antioxidants 2018, 7, 119. https://doi.org/10.3390/antiox7090119.
- Quindry, J.; Stone, W.; King, J.; Broeder, C. The effects of acute exercise on neutrophils and plasma oxidative stress. Med. Sci. Sport. Exerc. 2003, 35, 1139–1145.
- Powers, S.K.; Deminice, R.; Ozdemir, M.; Yoshihara, T.; Bomkamp, M.P.; Hyatt, H. Exercise-induced oxidative stress: Friend or foe? J. Sport Health Sci. 2020, 9, 415–425. https://doi.org/10.1016/j.jshs.2020.04.001.
- Thannickal, V.J.; Fanburg, B.L. Reactive oxygen species in cell signaling. Am. J. Physiol. Lung Cell Mol. Physiol. 2000, 279,
- Hancock, J.T.; Desikan, R.; Neill, S.J. Role of reactive oxygen species in cell signalling pathways. Biochem. Soc. Trans. 2001, 29, 345–350. https://doi.org/10.1042/0300-5127:0290345.
- Cobley, J.N.; McHardy, H.; Morton, J.P.; Nikolaidis, M.G.; Close, G.L. Influence of vitamin C and vitamin E on redox signaling: Implications for exercise adaptations. Free Radic. Biol. Med. 2015, 84, 65–76. https://doi.org/10.1016/j.freeradbiomed.2015.03.018.
- Reid, M.B. Nitric oxide, reactive oxygen species, and skeletal muscle contraction. Med. Sci. Sport. Exerc. 2001, 33, 371–376. https://doi.org/10.1097/00005768-200103000-00006.
- He, F.; Li, J.; Liu, Z.; Chuang, C.C.; Yang, W.; Zuo, L. Redox Mechanism of Reactive Oxygen Species in Exercise. Front. Physiol. 2016, 7, 486. https://doi.org/10.3389/fphys.2016.00486.
- Ji, L.L. Antioxidant enzyme response to exercise and aging. Med. Sci. Sport. Exerc. 1993, 25, 225–231.
- Lipska, K.J. Patient education: Exercise and medical care for people with type 2 diabetes (Beyond the Basics). Available online: www.uptodate.com/contents/exercise-and-medical-care-for-people-with-type-2-diabetes-beyond-the-basics (accessed on 22 May 2023).
- Khandelwal, D.; Dutta, D.; Chittawar, S.; Kalra, S. Sleep Disorders in Type 2 Diabetes. Indian J. Endocrinol. Metab. 2017, 21,
- Kelly, S.J.; Ismail, M. Stress and type 2 diabetes: A review of how stress contributes to the development of type 2 diabetes. Annu. Rev. Public Health 2015, 36, 441–462. https://doi.org/10.1146/annurev-publhealth-031914-122921.
- Atrooz, F.; Salim, S. Sleep deprivation, oxidative stress and inflammation. Adv. Protein Chem. Struct. Biol. 2020, 119, 309–336. https://doi.org/10.1016/bs.apcsb.2019.03.001.
- Hill, V.M.; O’Connor, R.M.; Sissoko, G.B.; Irobunda, I.S.; Leong, S.; Canman, J.C.; Stavropoulos, N.; Shirasu-Hiza, M. A bidirectional relationship between sleep and oxidative stress in Drosophila. PLoS Biol. 2018, 16, e2005206. https://doi.org/10.1371/journal.pbio.2005206.
- Moller, P.; Wallin, H.; Knudsen, L.E. Oxidative stress associated with exercise, psychological stress and life-style factors. Chem. Biol. Interact. 1996, 102, 17–36. Available online: http://biomednet.com/db/medline/96424598 (accessed on).
- Belaïdi, E. Oxidative Stress and Sleep Disorders. Available online: https://www.mdpi.com/journal/antioxidants/special_issues/Oxidative_Stress_and_Sleep_Disorders (accessed on 26 April 2023).
- Lauridsen, C.; Jensen, S.K. α-Tocopherol incorporation in mitochondria and microsomes upon supranutritional vitamin E supplementation. Genes Nutr. 2012, 7, 475–482. https://doi.org/10.1007/s12263-012-0286-6.
- Sen, C.K.; Khanna, S.; Roy, S. Tocotrienols in health and disease: The other half of the natural vitamin E family. Mol. Asp. Med. 2007, 28, 692–728. https://doi.org/10.1016/j.mam.2007.03.001.
- Azzi, A.; Gysin, R.; Kempna, P.; Munteanu, A.; Negis, Y.; Villacorta, L.; Visarius, T.; Zingg, J.M. Vitamin E mediates cell signaling and regulation of gene expression. Ann. N. Y. Acad. Sci. 2004, 1031, 86–95.
- Zingg, J.M. Vitamin E: A Role in Signal Transduction. Annu. Rev. Nutr. 2015, 35, 135–173. https://doi.org/10.1146/annurev-nutr-071714-034347.
- Balbi, M.E.; Tonin, F.S.; Mendes, A.M.; Borba, H.H.; Wiens, A.; Fernandez-Llimos, F.; Pontarolo, R. Antioxidant effects of vitamins in type 2 diabetes: A meta-analysis of randomized controlled trials. Diabetol. Metab. Syndr. 2018, 10, 18. https://doi.org/10.1186/s13098-018-0318-5.
- Chow, C.K.; Ibrahim, W.; Wei, Z.; Chan, A.C. Vitamin E regulates mitochondrial hydrogen peroxide generation. Free Radic. Biol. Med. 1999, 27, 580–587. https://doi.org/10.1016/s0891-5849(99)00121-5.
- El-Aal, A.A.; El-Ghffar, E.A.A.; Ghali, A.A.; Zughbur, M.R.; Sirdah, M.M. The effect of vitamin C and/or E supplementations on type 2 diabetic adult males under metformin treatment: A single-blinded randomized controlled clinical trial. Diabetes Metab. Syndr. 2018, 12, 483–489. https://doi.org/10.1016/j.dsx.2018.03.013.
- Vafa, M.; Haghighat, N.; Moslehi, N.; Eghtesadi, S.; Heydari, I. Effect of Tocotrienols enriched canola oil on glycemic control and oxidative status in patients with type 2 diabetes mellitus: A randomized double-blind placebo-controlled clinical trial. J. Res. Med. Sci. 2015, 20, 540–547. https://doi.org/10.4103/1735-1995.165945.
- Baliarsingh, S.; Beg, Z.H.; Ahmad, J. The therapeutic impacts of tocotrienols in type 2 diabetic patients with hyperlipidemia. Atherosclerosis 2005, 182, 367–374. https://doi.org/10.1016/j.atherosclerosis.2005.02.020.
- Ho, J.I.; Ng, E.Y.; Chiew, Y.; Koay, Y.Y.; Chuar, P.F.; Phang, S.C.W.; Ahmad, B.; Kadir, K.A. The effects of vitamin E on non-proliferative diabetic retinopathy in type 2 diabetes mellitus: Are they sustainable with 12 months of therapy. SAGE Open Med. 2022, 10, https://doi.org/10.1177/20503121221095324.
- Kalvaitus, K.; Portnoy, S.A. Available online: https://www.healio.com/news/endocrinology/20120325/experts-recommend-two-pronged-approach-to-treating-prediabetes (accessed on 11 January 2023).
- Suleman, F.; Khan, D.A.; Pervez, M.A.; Aamir, M. Effects of delta-tocotrienol supplementation on glycaemic control in individuals with prediabetes: A randomized controlled study. J. Pak. Med. Assoc. 2022, 72, 4–7. https://doi.org/10.47391/JPMA.966.
- Fang, F.; Kang, Z.; Wong, C. Vitamin E tocotrienols improve insulin sensitivity through activating peroxisome proliferator-activated receptors. Mol. Nutr. Food Res. 2010, 54, 345–352. https://doi.org/10.1002/mnfr.200900119.
- Mason, S.A.; Parker, L.; van der Pligt, P.; Wadley, G.D. Vitamin C supplementation for diabetes management: A comprehensive narrative review. Free Radic. Biol. Med. 2023, 194, 255–283. https://doi.org/10.1016/j.freeradbiomed.2022.12.003.
- Sun, H.; Karp, J.; Sun, K.M.; Weaver, C.M. Decreasing Vitamin C Intake, Low Serum Vitamin C Level and Risk for US Adults with Diabetes. Nutrients 2022, 14, 3902. https://doi.org/10.3390/nu14193902.
- Liu, M.; Park, S. A Causal Relationship between Vitamin C Intake with Hyperglycemia and Metabolic Syndrome Risk: A Two-Sample Mendelian Randomization Study. Antioxidants 2022, 11, 857. https://doi.org/10.3390/antiox11050857.
- Ebenuwa, I.; Violet, P.C.; Padayatty, S.; Wang, Y.; Sun, H.; Adhikari, P.; Smith, S.; Tu, H.; Niyyati, M.; Wilkins, K.; et al. Abnormal urinary loss of vitamin C in diabetes: Prevalence and clinical characteristics of a vitamin C renal leak. Am. J. Clin. Nutr. 2022, 116, 274–284. https://doi.org/10.1093/ajcn/nqac063.
- Shi, L.; Du, X.; Guo, P.; Huang, L.; Qi, P.; Gong, Q. Ascorbic acid supplementation in type 2 diabetes mellitus: A protocol for systematic review and meta-analysis. Medicine 2020, 99, e23125. https://doi.org/10.1097/MD.0000000000023125.
- Mason, S.A.; Keske, M.A.; Wadley, G.D. Effects of Vitamin C Supplementation on Glycemic Control and Cardiovascular Risk Factors in People With Type 2 Diabetes: A GRADE-Assessed Systematic Review and Meta-analysis of Randomized Controlled Trials. Diabetes Care 2021, 44, 618–630. https://doi.org/10.2337/dc20-1893.
- Jiang, C.L.; Tsao, C.Y.; Lee, Y.C. Vitamin C attenuates predisposition to high-fat diet-induced metabolic dysregulation in GLUT10-deficient mouse model. Genes Nutr. 2022, 17, 10. https://doi.org/10.1186/s12263-022-00713-y.
- Wilson, R.; Willis, J.; Gearry, R.; Skidmore, P.; Fleming, E.; Frampton, C.; Carr, A. Inadequate Vitamin C Status in Prediabetes and Type 2 Diabetes Mellitus: Associations with Glycaemic Control, Obesity, and Smoking. Nutrients 2017, 9, 997. https://doi.org/10.3390/nu9090997.
- Stanimirovic, J.; Radovanovic, J.; Banjac, K.; Obradovic, M.; Essack, M.; Zafirovic, S.; Gluvic, Z.; Gojobori, T.; Isenovic, E.R. Role of C-Reactive Protein in Diabetic Inflammation. Mediat. Inflamm 2022, 2022, 3706508. https://doi.org/10.1155/2022/3706508.
- Valko, M.; Izakovic, M.; Mazur, M.; Rhodes, C.J.; Telser, J. Role of oxygen radicals in DNA damage and cancer incidence. Mol. Cell Biochem. 2004, 266, 37–56. https://doi.org/10.1023/b:mcbi.0000049134.69131.89.
- Sagun, K.C.; Cárcamo, J.M.; Golde, D.W. Vitamin C enters mitochondria via facilitative glucose transporter 1 (Glut1) and confers mitochondrial protection against oxidative injury. FASEB J. 2005, 19, 1657–1667. https://doi.org/10.1096/fj.05-4107com.
- Bansal, A.; Hadimani, C.P. Low Plasma Ascorbate Levels in Type 2 Diabetic Patients With Adequate Dietary Vitamin C. J. Lab. Physicians 2021, 13, 139–143. https://doi.org/10.1055/s-0041-1730751.
- Sinclair, A.J.; Taylor, P.B.; Lunec, J.; Girling, A.J.; Barnett, A.H. Low plasma ascorbate levels in patients with type 2 diabetes mellitus consuming adequate dietary vitamin C. Diabet. Med. 1994, 11, 893–898. https://doi.org/10.1111/j.1464-5491.1994.tb00375.x.
- Chen, H.; Karne, R.J.; Hall, G.; Campia, U.; Panza, J.A.; Cannon, R.O.; Wang, Y.; Katz, A.; Levine, M.; Quon, M.J. High-dose oral vitamin C partially replenishes vitamin C levels in patients with Type 2 diabetes and low vitamin C levels but does not improve endothelial dysfunction or insulin resistance. Am. J. Physiol. Heart Circ. Physiol. 2006, 290, H137–145. https://doi.org/10.1152/ajpheart.00768.2005.
- Bonner, R.; Albajrami, O.; Hudspeth, J.; Upadhyay, A. Diabetic Kidney Disease. Prim. Care 2020, 47, 645–659. https://doi.org/10.1016/j.pop.2020.08.004.
- Afkhami-Ardekani, M.; Shojaoddiny-Ardekani, A. Effect of vitamin C on blood glucose, serum lipids & serum insulin in type 2 diabetes patients. Indian J. Med. Res. 2007, 126, 471–474.
- Donin, A.S.; Dent, J.E.; Nightingale, C.M.; Sattar, N.; Owen, C.G.; Rudnicka, A.R.; Perkin, M.R.; Stephen, A.M.; Jebb, S.A.; Cook, D.G.; et al. Fruit, vegetable and vitamin C intakes and plasma vitamin C: Cross-sectional associations with insulin resistance and glycaemia in 9–10 year-old children. Diabet. Med. 2016, 33, 307–315. https://doi.org/10.1111/dme.13006.
- Parajuli, S.; Jasmin, G.; Sirak, H.; Lee, A.F.; Nwosu, B.U. Prediabetes: Adherence to Nutrition Visits Decreases HbA1c in Children and Adolescents. Front. Endocrinol. 2022, 13, 916785. https://doi.org/10.3389/fendo.2022.916785.
- Strain, J.J.; Mulholland, C.W. Vitamin C and vitamin E--synergistic interactions in vivo? EXS 1992, 62, 419–422. https://doi.org/10.1007/978-3-0348-7460-1_40.
- Azzi, A. Tocopherols, tocotrienols and tocomonoenols: Many similar molecules but only one vitamin E. Redox Biol. 2019, 26, 101259. https://doi.org/10.1016/j.redox.2019.101259.
- Pangrazzi, L.; Balasco, L.; Bozzi, Y. Natural Antioxidants: A Novel Therapeutic Approach to Autism Spectrum Disorders? Antioxidants 2020, 9, 1186. https://doi.org/10.3390/antiox9121186.
- Buettner, G.R. The pecking order of free radicals and antioxidants: Lipid peroxidation, alpha-tocopherol, and ascorbate. Arch. Biochem. Biophys. 1993, 300, 535–543. https://doi.org/10.1006/abbi.1993.1074.
- Ayala, A.; Muñoz, M.F.; Argüelles, S. Lipid peroxidation: Production, metabolism, and signaling mechanisms of malondialdehyde and 4-hydroxy-2-nonenal. Oxid. Med. Cell Longev. 2014, 2014, 360438. https://doi.org/10.1155/2014/360438.
- de Souza Bastos, A.; Graves, D.T.; de Melo Loureiro, A.P.; Júnior, C.R.; Corbi, S.C.T.; Frizzera, F.; Scarel-Caminaga, R.M.; Câmara, N.O.; Andriankaja, O.M.; Hiyane, M.I.; et al. Diabetes and increased lipid peroxidation are associated with systemic inflammation even in well-controlled patients. J. Diabetes Complicat. 2016, 30, 1593–1599. https://doi.org/10.1016/j.jdiacomp.2016.07.011.
- Augustine, J.; Troendle, E.P.; Barabas, P.; McAleese, C.A.; Friedel, T.; Stitt, A.W.; Curtis, T.M. The Role of Lipoxidation in the Pathogenesis of Diabetic Retinopathy. Front. Endocrinol. 2020, 11, 621938. https://doi.org/10.3389/fendo.2020.621938.
- Sato, A.; Takino, Y.; Yano, T.; Fukui, K.; Ishigami, A. Determination of tissue-specific interaction between vitamin C and vitamin E. Br. J. Nutr. 2022, 128, 993–1003. https://doi.org/10.1017/S0007114521004384.
- Porkkala-Sarataho, E.; Salonen, J.T.; Nyyssönen, K.; Kaikkonen, J.; Salonen, R.; Ristonmaa, U.; Diczfalusy, U.; Brigelius-Flohe, R.; Loft, S.; Poulsen, H.E. Long-term effects of vitamin E, vitamin C, and combined supplementation on urinary 7-hydro-8-oxo-2’-deoxyguanosine, serum cholesterol oxidation products, and oxidation resistance of lipids in nondepleted men. Arter. Thromb. Vasc. Biol. 2000, 20, 2087–2093. https://doi.org/10.1161/01.atv.20.9.2087.
- Huang, H.Y.; Appel, L.J.; Croft, K.D.; Miller, E.R.; Mori, T.A.; Puddey, I.B. Effects of vitamin C and vitamin E on in vivo lipid peroxidation: Results of a randomized controlled trial. Am. J. Clin. Nutr. 2002, 76, 549–555. https://doi.org/10.1093/ajcn/76.3.549.
- Mazloom, Z.; Hejazi, N.; Dabbaghmanesh, M.H.; Tabatabaei, H.R.; Ahmadi, A.; Ansar, H. Effect of vitamin C supplementation on postprandial oxidative stress and lipid profile in type 2 diabetic patients. Pak. J. Biol. Sci. 2011, 14, 900–904. https://doi.org/10.3923/pjbs.2011.900.904.
- Neri, S.; Calvagno, S.; Mauceri, B.; Misseri, M.; Tsami, A.; Vecchio, C.; Mastrosimone, G.; Di Pino, A.; Maiorca, D.; Judica, A.; et al. Effects of antioxidants on postprandial oxidative stress and endothelial dysfunction in subjects with impaired glucose tolerance and type 2 diabetes. Eur. J. Nutr. 2010, 49, 409–416. https://doi.org/10.1007/s00394-010-0099-6.
- Holley, A.K.; Bakthavatchalu, V.; Velez-Roman, J.M.; St Clair, D.K. Manganese superoxide dismutase: Guardian of the powerhouse. Int. J. Mol. Sci. 2011, 12, 7114–7162. https://doi.org/10.3390/ijms12107114.
- Lee, S.H.; Jouihan, H.A.; Cooksey, R.C.; Jones, D.; Kim, H.J.; Winge, D.R.; McClain, D.A. Manganese supplementation protects against diet-induced diabetes in wild type mice by enhancing insulin secretion. Endocrinology 2013, 154, 1029–1038. https://doi.org/10.1210/en.2012-1445.
- Burlet, E.; Jain, S.K. Manganese supplementation reduces high glucose-induced monocyte adhesion to endothelial cells and endothelial dysfunction in Zucker diabetic fatty rats. J. Biol. Chem. 2013, 288, 6409–6416. https://doi.org/10.1074/jbc.M112.447805.
- Du, S.; Wu, X.; Han, T.; Duan, W.; Liu, L.; Qi, J.; Niu, Y.; Na, L.; Sun, C. Dietary manganese and type 2 diabetes mellitus: Two prospective cohort studies in China. Diabetologia 2018, 61, 1985–1995. https://doi.org/10.1007/s00125-018-4674-3.
- Wang, X.; Zhang, M.; Lui, G.; Chang, H.; Liu, W.; Li, Z.; Liu, Y.; Huang, G. Associations of Serum Manganese Levels with Prediabetes and Diabetes among ≥60-Year-Old Chinese Adults: A Population-Based Cross-Sectional Analysis. Nutrients 2016, 8, 497. https://doi.org/10.3390/nu8080497.
- Chen, H.; Cui, Z.; Lu, W.; Wang, P.; Wang, J.; Zhou, Z.; Zhang, N.; Wang, Z.; Lin, T.; Song, Y.; et al. Association between serum manganese levels and diabetes in Chinese adults with hypertension. J. Clin. Hypertens 2022, 24, 918–927. https://doi.org/10.1111/jch.14520.
- van der Schaft, N.; Schoufour, J.D.; Nano, J.; Kiefte-de Jong, J.C.; Muka, T.; Sijbrands, E.J.G.; Ikram, M.A.; Franco, O.H.; Voortman, T. Dietary antioxidant capacity and risk of type 2 diabetes mellitus, prediabetes and insulin resistance: The Rotterdam Study. Eur. J. Epidemiol. 2019, 34, 853–861. https://doi.org/10.1007/s10654-019-00548-9.
- Brigelius-Flohé, R.; Flohé, L. Regulatory Phenomena in the Glutathione Peroxidase Superfamily. Antioxid. Redox Signal. 2020, 33, 498–516. https://doi.org/10.1089/ars.2019.7905.
- Katz, M.L.; Stone, W.L.; Dratz, E.A. Fluorescent pigment accumulation in retinal pigment epithelium of antioxidant-deficient rats. Investig. Ophthalmol. Vis. Sci. 1978, 17, 1049–1058.
- Ogawa-Wong, A.N.; Berry, M.J.; Seale, L.A. Selenium and Metabolic Disorders: An Emphasis on Type 2 Diabetes Risk. Nutrients 2016, 8, 80. https://doi.org/10.3390/nu8020080.
- Marcelino, G.; Machate, D.J.; Freitas, K.C.; Hiane, P.A.; Maldonade, I.R.; Pott, A.; Asato, M.A.; Candido, C.J.; Guimarães, R.C.A. β-Carotene: Preventive Role for Type 2 Diabetes Mellitus and Obesity: A Review. Molecules 2020, 25, 5803. https://doi.org/10.3390/molecules25245803.
- Jiang, Y.W.; Sun, Z.H.; Tong, W.W.; Yang, K.; Guo, K.Q.; Liu, G.; Pan, A. Dietary Intake and Circulating Concentrations of Carotenoids and Risk of Type 2 Diabetes: A Dose-Response Meta-Analysis of Prospective Observational Studies. Adv. Nutr. 2021, 12, 1723–1733. https://doi.org/10.1093/advances/nmab048.
- Available online: https://www.aap.org/en/practice-management/bright-futures/bright-futures-materials-and-tools/bright-futures-guidelines-and-pocket-guide/ (accessed on 11 January 2023).
- Eddolls, W.T.B.; McNarry, M.A.; Stratton, G.; Winn, C.O.N.; Mackintosh, K.A. High-Intensity Interval Training Interventions in Children and Adolescents: A Systematic Review. Sport. Med. 2017, 47, 2363–2374. https://doi.org/10.1007/s40279-017-0753-8.
