Palliative care is intended to relieve caregivers of physical, psychological, and even spiritual elements of care. One of the most prevalent issues facing this form of care is a lack of healthcare resources and structures to deal with an aging population. This aging population is placing a strain on the healthcare system, prompting a need for a shift in system management. A potential answer to this issue may be the Multi-Agent System (MAS). This category of computerized networking system was created by programmers to gather relevant health information on a patient and allow for the system to act with other agents to decide the best course for disease management. It can also allow for a multidisciplinary healthcare team to make more informed plans of actions for their patients by providing accurate and up-to-date information resulting from a greater synergetic mesh. MASs could fulfill the demands of a rising chronic illness population and deliver high-quality care, indicating a major paradigm shift within the US.
- palliative care
- chronic disease
- multi-agent systems
1. Introduction
2. Chronic Disease and Contributing Factors
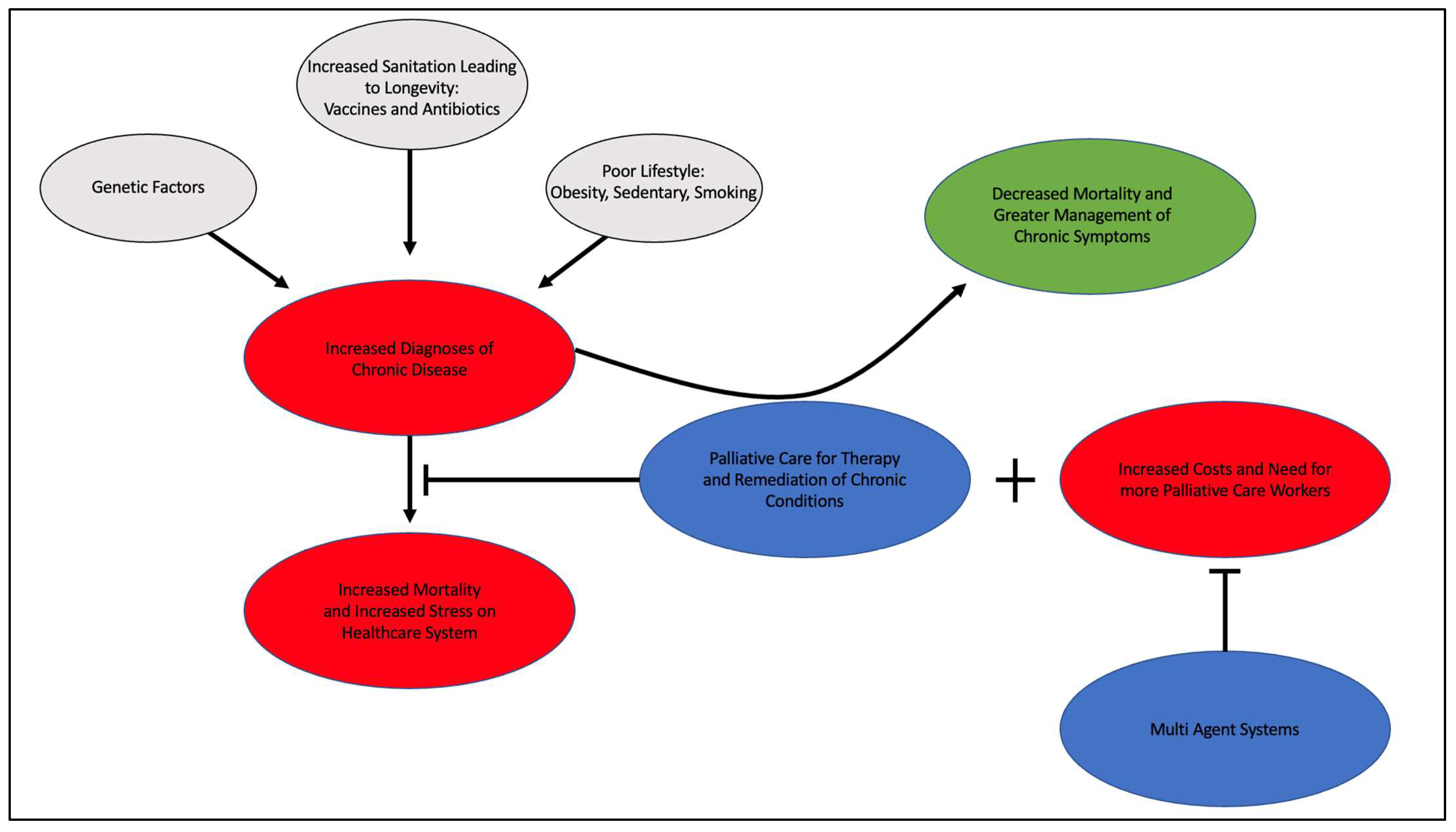
The prevalence of chronic disease within the United States has seen marked increases in the last few decades. In 2007, nearly half the population suffered from at least one chronic disease [5]. Data from 2022 suggests this number now encompasses almost 60% of Americans [6]. The staggering growth of an almost 10% increase in only 15 years’ time is related to multiple factors that have harmonized to produce a cacophonous dilemma, which is to say that the United States is facing a chronic disease epidemic. The contributing factors to this epidemic include increasing longevity due to improved sanitation/vaccines/antibiotics, poor lifestyle choices in the form of overeating/sedentation/smoking, and genetic factors that predispose one to chronic disease.
Another contributing factor to increasing chronic disease is the poor lifestyle seen within the US. Some of the high-risk factors for chronic disease that the CDC recommends avoiding are smoking, drinking, and a sedentary lifestyle [11][7]. Smoking habits within the US have seen decreases, from 20.9% in 2005 to 12.5% in 2020 [12][8]. The incidence of drinking within the US is nearly 50% with binge drinking at nearly 17% [13][9]. The prevalence of obesity in the US from 2017–2020 was 41.9%, with the prevalence in non-Hispanic black adults as high as 49.9% [14][10].
As the US struggles to treat these individual factors, the incidence of chronic disease is ever increasing. This places high demand on the healthcare system in the form of reactive rather than proactive care. When untreated, chronic illnesses progress gradually and thus individuals with chronic conditions require more long-term treatment. One such long-term treatment is palliative care, which is a branch of medicine that involves multidisciplinary care for the symptoms associated with advanced chronic illnesses. In the context of the US, palliative care is high-level care from a multidisciplinary team with efforts focused on curative ends [16][11]. Hospice care shares the same aspects as palliative care; however, it differs fundamentally in terms of comfort measures only because curative efforts have been largely abandoned [16][11]. Palliative and hospice care have been proven to improve the quality of life and medical care in end-of-life treatment [17][12]. With improved life expectancy and the contributing factors therein, the question of how these patients suffering from chronic illness will be cared for is of increasing import. The current medical system allots over 80% of its expenses to chronic disease treatment per year [18][13]. Despite the magnitude of the expenditures devoted to the treatment of chronic illness, data projects that the prevalence of chronic illness will continue to increase [5]. Therefore, the need for a new medical system, or one bolstered with a more powerful synergistic factor, is of great necessity in order to combat this growing epidemic. A potential candidate for this position may be the Multi-Agent System (MAS). With MASs, a system of agents can make predictions on the steps needed to improve the patient’s health and can be updated in real time at a central location, and thus may allow for an additional layer of synergism to be added to the healthcare schema [4]. The use of this system could greatly expand and make efficient the resources that are already present, mitigating the increased costs of instituting palliative care as a healthcare standard in the treatment of chronic disease.
3. Multi-Agent Systems and Palliative Care
Multi-agent systems are computerized networks that use agents to cross-reference and monitor relevant health data on a patient and then proactively or reactively make changes to benefit the patient without the need for human intervention [4]. The “agents” referred to in this framework are individual programs that can use artificial intelligence techniques in order to act on and correct course to a desired goal or range, as programmed [4]. These agents are highly variable in their specified capability as interpreted by their given programming; however, all agents must have three aspects: sociability, pro-activeness, and responsiveness [19][14]. Sociability refers to the interaction of the agent with other agents, physicians, and patients in an effort to solve a problem. Pro-activeness is the ability to predict the need for action before prompted and make efforts to mitigate that eventuality. Responsiveness refers to the ability to perceive the directed environment and make changes [19][14]. The principal advantage and usefulness of multi-agent systems is the ability to have multiple entities that will interact with differential capacities to reach a solution to a proposed problem through cooperation, coordination, and negotiation [19][14]
Multi-agent systems exist to combine the efforts of these agents to provide a more wholistic spectrum of care, make efficient use of existing resources, and reduce costs to the system they are engaged in. MASs enhance complex problem-solving capabilities amongst healthcare system collaborators to provide effective care to various patient populations. By 2030, approximately 20% of the U.S. population will be older than age 65. Therefore, there is a growing need for a more cost-effective healthcare decision-making platform [22,23][15][16]. Multi-agent systems provide solutions for multiple healthcare sectors, such as organ transplantation and palliative care, due to the number of stakeholders required to make a shared medical decision [24,25][17][18]. Different stakeholders in healthcare include, but are not limited to, patients, doctors, medical institutions, governments, and medical insurance agencies [26][19]. MASs address a significant barrier within healthcare systems: interoperability [27][20]. In healthcare, solving problems requires the coordination of numerous individuals with different skills and functions, and the required knowledge is spatially distributed in different places [24][17]. To provide the best treatment possible, it would be of great benefit for all agents and knowledge to be significantly coordinated. This coordination begets a level of interoperability that the current systems do not have. Interoperability implements a space for the coordination of actions and the exchange of information [10][21]. The application of MASs within healthcare can monitor and coordinate all stakeholders who perform different tasks based on distinct information in order to devise a comprehensive solution to a patient’s problem. This makes them a viable solution in the managing, coordinating, controlling, and modeling of many different healthcare problems [28][22]. It quickly becomes more of a requirement than an option, particularly in health information systems [27][20].
4. Conclusions
The aging population within the US is growing and will continue to cause greater strain on the healthcare system. If instituted as a healthcare standard for patients with chronic illness, palliative care services powered by MASs could satisfy the requirements of an ever-growing chronic illness-stricken population, while also providing high-quality healthcare. The use of MASs may prove to be a necessary paradigm shift in healthcare as the chronic disease patient population continues to expand. While many efforts have been made to prevent chronic disease before it begins, it is imperative that greater care be offered to those already suffering from it. Given the success of several studies that have shown the advantageous nature of MASs as a healthcare standard, this system is worthy of further investigation and potentially implementation as a staple healthcare system that may vastly improve our health as a nation.References
- Al-Mahrezi, A.; Al-Mandhari, Z. Palliative Care: Time for Action. Oman Med. J. 2016, 31, 161–163.
- Palliative Care Improves Quality of Life. Available online: https://newsinhealth.nih.gov/2017/01/palliative-care-improves-quality-life (accessed on 6 January 2023).
- Palliative Care and Disease Types|Get Palliative Care. Available online: https://getpalliativecare.org/whatis/disease-types/ (accessed on 6 January 2023).
- Alva, H.; Sequeira, A.H.; Narayana, V.N. Proactive Approach to Palliative Care through Routine Monitoring by Home Caregivers Using Multiagent Systems: A Conceptual Framework. Rochester, NY. 2017. Available online: https://papers.ssrn.com/abstract=3022771 (accessed on 6 January 2023).
- 071204_H4L_FocusonWellness.pdf . Available online: https://www.aha.org/system/files/content/00-10/071204_H4L_FocusonWellness.pdf (accessed on 6 January 2023).
- Hoffman, D. Commentary on Chronic Disease Prevention in 2022. National Association of Chronic Disease Directors. Available online: https://chronicdisease.org/wp-content/uploads/2022/04/FS_ChronicDiseaseCommentary2022FINAL.pdf (accessed on 6 January 2023).
- How You Can Prevent Chronic Diseases|CDC. Available online: https://www.cdc.gov/chronicdisease/about/prevent/index.htm (accessed on 6 January 2023).
- CDC Current Cigarette Smoking Among Adults in the United States. Centers for Disease Control and Prevention. 2022. Available online: https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm (accessed on 6 January 2023).
- Data on Excessive Drinking|CDC. Available online: https://www.cdc.gov/alcohol/data-stats.htm (accessed on 6 January 2023).
- CDC Obesity is a Common, Serious, and Costly Disease. Centers for Disease Control and Prevention. 2022. Available online: https://www.cdc.gov/obesity/data/adult.html (accessed on 6 January 2023).
- Palliative Care vs. Hospice: Which to Choose. CaringInfo. Available online: https://www.caringinfo.org/types-of-care/what-is-the-difference-between-palliative-care-and-hospice-care/ (accessed on 6 January 2023).
- Cruz-Oliver, D.M. Palliative Care: An Update. Mo. Med. 2017, 114, 110–115.
- Chronic Disease in the United States: A Worsening Health and Economic Crisis. AAF. Available online: https://www.americanactionforum.org/research/chronic-disease-in-the-united-states-a-worsening-health-and-economic-crisis/ (accessed on 6 January 2023).
- A Roadmap of Agent Research and Development. Available online: https://www.researchgate.net/publication/220660843_A_Roadmap_of_Agent_Research_and_Development (accessed on 6 January 2023).
- Bureau, U.C. Older People Projected to Outnumber Children for First Time in U.S. History. Census.gov. Available online: https://www.census.gov/newsroom/press-releases/2018/cb18-41-population-projections.html (accessed on 6 January 2023).
- Anderson, L.A.; Goodman, R.A.; Holtzman, D.; Posner, S.F.; Northridge, M.E. Aging in the United States: Opportunities and Challenges for Public Health. Am. J. Public Health 2012, 102, 393–395.
- Moreno, A. Medical Applications of Multi-Agent Systems. 12 April 2003. Available online: https://www.researchgate.net/publication/2901914_Medical_Applications_of_Multi-Agent_Systems (accessed on 6 January 2023).
- Shakshuki, E.; Reid, M. Multi-Agent System Applications in Healthcare: Current Technology and Future Roadmap. Procedia Comput. Sci. 2015, 52, 29–34.
- Yu, W.; Liu, X.; Zhao, F.; Li, M.; Zhang, L. Control of unreasonable growth of medical expenses in public hospitals in Shanghai, China: A multi-agent system model. BMC Health Serv. Res. 2020, 20, 490.
- Cardoso, L.; Marins, F.; Portela, F.; Santos, M.; Abelha, A.; Machado, J. The Next Generation of Interoperability Agents in Healthcare. Int. J. Environ. Res. Public. Health 2014, 11, 5349–5371.
- Pollard, A.J.; Bijker, E.M. A guide to vaccinology: From basic principles to new developments. Nat. Rev. Immunol. 2021, 21, 83–100.
- Safdari, R.; Shoshtarian Malak, J.; Mohammadzadeh, N.; Danesh Shahraki, A. A Multi Agent Based Approach for Prehospital Emergency Management. Bull. Emerg. Trauma 2017, 5, 171–178.
- Mohammadzadeh, N.; Safdari, R.; Rahimi, A. Multi-agent systems: Effective approach for cancer care information management. Asian Pac. J. Cancer Prev. APJCP 2013, 14, 7757–7759.
- Mohammadzadeh, N.; Safdari, R.; Rahimi, A. Multi-Agent System as a New Approach to Effective Chronic Heart Failure Management: Key Considerations. Healthc. Inform. Res. 2013, 19, 162–166.
