1. Development of Electronic Health and Artificial Intelligence in Surgery after the SARS-CoV-2 Pandemic Globally
The onset of the SARS-CoV-2 pandemic has dramatically transformed healthcare systems globally. For instance, the outbreak has prompted the realization that there is a vast connection between eHealth, artificial intelligence, and digital inequalities
[1]. These connections imply that the elderly and the impoverished individuals in society are more likely to miss out on the benefits of eHealth globally
[1]. Another study by Sockalingam, Leung, and Cassin showcased that the pandemic has increased eHealth use as physicians use the technology to reach out to patients and deal with various distresses after a surgical procedure
[2]. A review by Tsopra et al. indicated that developing eHealth and artificial intelligence in surgery after SARS-CoV-2 in the African continent is likely to encounter numerous challenges due to the differences in healthcare guidelines given for different countries
[3]. In addition, the authors posit that it is necessary for medical studies in the surgical field to involve general practitioners in the data collection process
[3]. Many hospitals globally have had to adopt measures that minimize the risk of hospital staff and patients contracting SARS-CoV-2. For instance, in facial surgeries, doctors have mostly prioritized injuries on critical locations such as the eyelids and deferred cases involving temporomandibular pathologies
[4]. The issues on the deferred list have had to rely on eHealth to meet their various medical requirements, hence presenting a chance for the further development of the concept.
2. Development of Electronic Health and Artificial Intelligence in Surgery after the SARS-CoV-2 Pandemic in the United States
The history of electronic health and artificial intelligence in surgery in the United States dated to 1996 when a French patient underwent a laparoscopic cholecystectomy virtually with a surgeon located in New York
[5]. Zemmar, Lozano, and Nelson further stated that the technology adopted in the United States allows patients to undergo surgery without contacting the doctor
[4]. For example, the first patient of SARS-CoV-2 underwent isolation with a robot equipped with a camera, microphone, and a stethoscope
[5]. A review conducted by Messiah et al. on the application of eHealth in metabolic and bariatric surgery revealed that electronic health strategies effectively allowed post-metabolic bariatric surgery weight loss and enhanced health outcomes
[6]. However, the authors noted that most of the studies reviewed had study design limitations; therefore, it was hard to rely on the results
[6]. More importantly, Bokolo insisted that the American Medical Association has established many resources to enable physicians to acquire relevant advice via electronic health
[7]. In addition, California passed a bill before the pandemic requiring practitioners to adopt virtual technologies and eliminate the various barriers in the reimbursement of Medicaid for communal medical centers.
Amid the pandemic, the United States has further integrated the “Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020” with the primary goal of waiving and modifying the various restriction to eHealth visible in the Medicare package
[7]. According to Alonso et al., most of the studies (42%) on electronic health and artificial intelligence during the pandemic focus on the United States, thus implying that the country is at the forefront of applying the concepts in various medical procedures such as surgery
[8]. Another article by Feizi et al. revealed that in the United States, the use of AI is evident during the pandemic via the Corpath robotic arm, whose primary goal is to perform coronary interventions, especially in instances where professionals are dealing with SARS-CoV-2 patients
[9]. Haleem et al. reported that the prominence of AI application in cardiological surgery has gone up during the pandemic and has led to numerous benefits such as predicting and diagnosing heart illness
[10]. Furthermore, artificial intelligence has reduced the time and cost of surgery in the United States while encouraging the successful undertaking of precise surgeries
[10]. In neurosurgery, the lack of good AI tools reduced the number of operations
[11]. The urgency of neurology surgeries necessitates the development of sound and efficient AI systems after the SARS-CoV-2 era.
A study carried out by Salman et al. in Washington revealed that deep learning went up during the pandemic, whereby surgical departments applied the concept to reduce human contact
[12]. The authors also developed a model of artificial intelligence that was one hundred percent accurate in detecting SARS-CoV-2
[12]. Other than that, Secinaro et al. argued that many hospitals in the United States had adopted robotic-assisted surgery in numerous fields such as colorectal, orthopedic, and neural surgeries
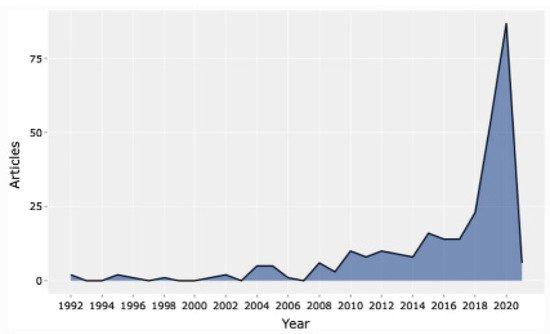
[13]. Consequently, studies concentrating on the importance of artificial intelligence in surgery have increased over the years, with the highest number witnessed during the SARS-CoV-2 pandemic, as displayed in
Figure 1.
Figure 1. Articles published on artificial intelligence from 1992–2020 (permission to reproduce from Secinaro et al.
[13]).
3. Development of Electronic Health and Artificial Intelligence in Surgery after the SARS-CoV-2 Pandemic in Europe
In Europe, the adoption of electronic health and artificial intelligence in surgery has gone up during the pandemic. For example, the Society of European Robotic Gynecological Surgery presented guidelines to doctors that promoted the integration of robot-assisted surgeries to minimize the risks of infection brought about by open surgery
[14]. In addition, the European Association of Urology released guidelines warning physicians to manage smoke dispersion in robotic surgery
[14]. These facts prove that the development of electronic health and AI in surgery after the SARS-CoV-2 in Europe is inevitable. In Italy, the need for electronic health and artificial intelligence upsurged after SARS-CoV-2 dramatically hit the region and caused the death of numerous residents
[15]. Bernardi et al. further insisted that the country-maintained follow-up medical cases, emergency procedures, and oncological surgeries
[15]. In a similar perspective, Gironi et al. argued that the field of dermatologic surgery experienced numerous cancellations, thereby forcing patients to turn to eHealth for consultations and non-urgent processes
[16]. Further, many hospitals in Italy have realized the need to adopt artificial intelligence as failure to integrate the notion has led to increased infections among staff and residents.
In Germany, the use of electronic health has increased during the SARS-CoV-2 pandemic, implying that future development is necessary and possible after the pandemic. For example, a study by Kirchberg et al. revealed that forty-two percent of the study participants, who were physicians, integrated medical applications in their phones
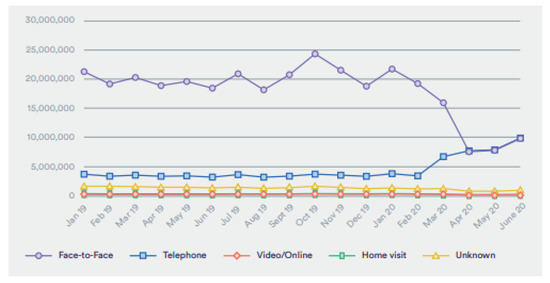
[17]. However, the study showcased that 82 percent of the research respondents admitted that they lacked sufficient knowledge on a myriad of eHealth factors such as the legal issues and information safety of medical apps in addition to cloud computing properties. In the United Kingdom, the adoption of eHealth in surgery has increased due to the reduction of GP visits. A study carried out by Hutchings revealed that GP visits were at 80% before the pandemic, which dramatically shifted to 40% after the pandemic, as shown in
Figure 3 [18]. These statistics reflect enhanced adoption of electronic health, and the trend is likely to continue after the pandemic as eHealth is efficient and effective. Moreover, the NHS introduced video consultations instead of face-to-face meetings with all patients to reduce the number of people visiting the hospital and the chances of transmitting the virus
[7].
Figure 3. Appointments to the general practitioners from January 2019 to June 2020 (permission to reproduce from Hutchings
[18]).
More importantly, France has demonstrated an increased use of electronic health during the pandemic, particularly in the field of colorectal cancer
[19]. Priou et al. argued that the factor needed further evaluation and better execution to handle concerns revolving around delayed detection in surgery
[19]. The use of artificial intelligence was less in the surgical domain in France, particularly lung transplant surgery. The lack of protective equipment and reduced lung donations has significantly contributed to reduced surgeries
[20]. In summary, despite the application of eHealth and AI during the pandemic in surgery, the adoption rate was minimal to attain satisfactory results. However, there is room for improvement since Donell et al. declared that European countries are still developing guidelines to ensure the medical staff and patients are safe
[21]. For instance, the European Hip Society and the European Knee Association have come together to develop eHealth and AI initiatives to deal with a future pandemic similar to SARS-CoV-2
[21]. Therefore, Europe is likely to enhance its adoption of electronic health and AI after the pandemic.
4. Development of Electronic Health and Artificial Health in Surgery after the SARS-CoV-2 Pandemic in Asia
According to Guo et al., in China, grown-ups with a higher socioeconomic status (SES) had higher eHealth literacy and received most of their information on SARS-CoV-2 through the Internet
[22]. Correspondingly, artificial intelligence in surgery is evident, whereby Wuhan Wuchang Hospital utilized robotics by establishing an intelligent field comprising fourteen robots tasked with cleaning, delivering drugs, and measuring the temperatures of surgical patients
[5]. In conjunction with that, Husain, Zhang, and Aung state that in health cases such as glaucoma in China, the health sector incorporated virtual consultation that reduced ocular morbidity from delayed care during the pandemic
[23]. In addition, after the SARS-CoV-2 pandemic, health care sectors in China started using digital technologies such as artificial intelligence and smartphone-based apps to change the control of glaucoma. Additionally, Bokolo posited that China adopted eHealth platforms such as WeChat and hotline to deal with surgery patients
[7]. Other hospitals in Wuhan incorporated innovative health tools, and big data analytics monitored remotely via observation cameras in Beijing
[7]. Consequently, the National Telemedicine Centre of China developed an emergency eHealth consultation system geared toward managing and monitoring patients’ health. During the pandemic, the country has further applied the Kirkpatrick training model in the emergency surgery department
[8].
5. Development of Electronic Health and Artificial Health in Surgery after the SARS-CoV-2 Pandemic in the Middle East
In the Middle East, the onset of the SARS-CoV-2 pandemic has triggered the utilization of electronic health and artificial intelligence in surgery. In Saudi Arabia, eHealth adoption increased during the pandemic since 89 percent of the population use the Internet, and more than 95 percent of Saudi residents have access to smartphones
[24]. The Ministry of Health of the state introduced the Tetamman app to allow healthcare professionals to deliver remote services to all patients, including those in the surgical domain. Further, Sharma and Ahmed claimed that Saudi Arabia had integrated many Internet of things applications to permit the diagnosis of the SARS-CoV-2 virus
[25]. For instance, the country has significantly applied cloud computing through the utilization of sensor devices. Hence, the development of eHealth and AI in Saudi Arabia is likely to pick up after the pandemic.
A study carried out by Ting et al. showcased that many hospitals situated in the Middle East did not have the relevant resources needed to distinguish SARS-CoV-2 from common flu, thereby indicating an eHealth and AI insufficiency in the locality
[26]. In a different view, Ferrara et al. stated that the virus’s rapid spread prompted countries in the Middle East to adopt strict containment measures to avoid spreading the virus
[27]. For example, in Lebanon, there have been numerous measures to promote eHealth adoption among refugees that are from Syria
[28]. Talhouk et al. revealed that challenges such as failure to provide medical services to refugees have significantly hindered eHealth incorporation among Syrian refugees in Lebanon
[28]. Subsequently, eHealth and artificial intelligence adoption in Syria cannot occur, given the increased levels of conflict in the locality. Bowsher et al. insisted that although the deployment of electronic health has increased during the pandemic, researchers still need to clarify the global norms applicable in the worldwide realm to ensure the prevalence of eHealth and AI in tumultuous regions
[29].
6. Development of Electronic Health and Artificial Intelligence in Surgery after the SARS-CoV-2 Pandemic in Africa
A study conducted by Ogundele et al. revealed the necessity of developing electronic health in pediatric surgery after the SARS-CoV-2 was necessary. There was a termination of elective surgeries in Nigeria and an enormous decline in emergency surgeries performed on toddlers
[30]. The reason why surgeons are not attending to their duties is that they do not feel safe operating on patients, especially those who have contracted SARS-CoV-2. Furthermore, people in Nigeria are currently living in fear of contracting the various, as it has affected their lives negatively and has also made the death toll rise. Further, Kelechi et al. argue that if technology and health care are linked, it will de-escalate the rate of SARS-CoV-2 infections and save more people
[31]. Additionally, the technology spreads awareness of the disease and assists the Government in monitoring and giving accurate compliance with the lockdown measures. According to Elkhouly, Salem, and Haggag, telemedicine in Egypt has helped reduce the rate of infection for a specific cluster of cancer patients
[32]. Treatment schedules were rescheduled to give patients seeking surgeries related to cancer priority to treatment.
Saba and Elsheikh stated that in Egypt, artificial intelligence models such as NARANN and ARIMA are used to assist in forecasting the prevalence of COVID-19, whereby the predicted information has a high determination coefficient for all groups of data
[33]. Further, Tara et al. reported that eHealth adoption in Egypt prompted the triaging of patients into three distinct categories
[34]. The telemedicine care division entailed using electronic channels to ensure patients received doctors’ necessary care
[34]. In Algeria, eHealth and artificial intelligence adoption are not successful due to the dysfunctional healthcare system adopted in the region
[34]. A review by Owoyemi et al. revealed that the eHealth and AI adoption in the African continent encounters the challenge of unavailability of large clinical datasets to steer the training of artificial intelligence models
[35]. In addition, legal issues concerning the use and privacy of eHealth and AI tools have significantly made it challenging for Africa to integrate the concepts into its healthcare domain so far.