1000/1000
Hot
Most Recent

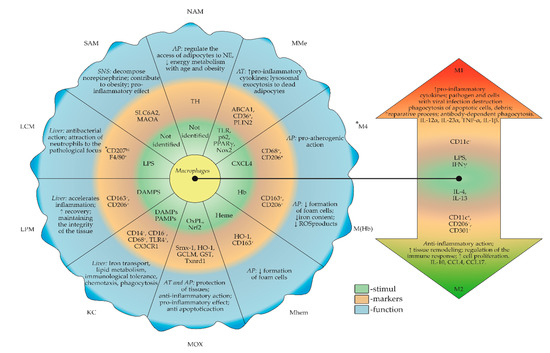
In clinical epidemiological studies, chronic stress was reported to be an independent risk factor for the development of atherosclerosis and the function of the intima. One of the hypotheses is based on the effect of chronic stress on the accumulation of macrophages in the intima and the acceleration of damage to the mucous membrane of vascular endothelial cells. Neutrophils, endothelial cells, platelets and fibroblasts are involved in the formation of a chronic inflammatory focus, accompanied by microcirculation disorders and angiogenic disorders. However, the main regulators of all cellular processes are immunocompetent cells and, predominantly, activated macrophages.