1000/1000
Hot
Most Recent

A number of medically-relevant zoonotic pathogens are negative-strand RNA viruses (NSVs). NSVs are derived from different virus families. Examples like Ebola are known for causing severe symptoms and high mortality rates. Some, like influenza, are known for their ease of person-to-person transmission and lack of pre-existing immunity, enabling rapid spread across many countries around the globe.
The human population is under the constant threat from infectious diseases, as seen in the consistent sporadic Ebola virus epidemics and the recent coronavirus and influenza virus pandemics. There is no doubt that the rapid global spread of viruses can have significant and far-reaching impact on health systems and the world’s economy. Research in emerging infectious diseases is advancing rapidly, with new breakthroughs in the understanding of host–pathogen interactions and the development of innovative and exciting vaccination strategies [1]. Since pandemics present such all-encompassing catastrophes, we must invest in developing basic research fundamentals and a better understanding of host–pathogen interactions for improved vaccine production to protect us from currently circulating infectious diseases and enable rapid response to emerging threats. As such, a significant challenge to achieve this goal is to refine the tools and processes necessary to efficiently develop and produce efficacious vaccines.
RNA viruses cause up to 44% of all emerging infectious diseases [2]. Negative strand RNA viruses (NSVs; order Mononegavirales) in particular are widely disseminated and of significant concern to human and animal health. These include the virus families Paramyxoviridae (measles (MV), mumps (MuV), respiratory syncytial virus (RSV), and human parainfluenza (HPIV) viruses), Orthomyxoviridae (influenza A virus (IAV)), Rhabdoviridae (rabies virus (RABV) and vesicular stomatitis virus (VSV)), Filoviridae (Ebola (EBOV), and Marburg (MARV) viruses). These viruses are responsible for a high burden of morbidity and mortality, especially in the developing world. Unlike positive strand RNA viruses, which are immediately translated by the host cells, thus directly facilitating replication and spread within the host, NSVs need to first have their RNA transcribed into a positive strand before initiating replication [3]. Due to their smaller genome size compared to DNA viruses, RNA viruses rely more heavily upon host cellular proteins [4]. However, this is hampered by their shorter generation time and the lack of polymerase proofreading function, leading to higher rates of mutation, up to five orders of magnitude compared to some DNA viruses [5]. This additional allows RNA viruses to more readily infect new host species [6]. Finally, the lack of effective animal models and the requirement of high containment facilities to perform NSV research contribute to the challenges of studying NSVs.
Some of the diseases caused by NSVs have been successfully controlled through immunization, as in the case of MV and MuV. Nevertheless, others still require the development of appropriate strategies for long term vaccination successes. These include both traditional and innovative strategies, involving live attenuated viruses, inactivated, subunit, protein, vectored, and nucleic acids vaccines [7][8][9][10]. Additionally, research has not only focused on the vaccine itself, but also on the procedures associated with their manufacture to improve the speed, yield, and cost of production. For example, methods using vaccine production substrates that incorporate approaches from the use of embryonated chicken eggs, baculovirus expression vectors in insect cells, and synthetic chemistry and use of engineered human or animal cells [6][7][8][9][10].
Nonetheless, the success of a vaccine stands not only on its manufacturing efficiency, but also on its ability to induce long lasting protective immunity. Vaccines present a range of different antigens to the cells located both on the surface and within virus particles, and it is critical that they induce appropriate responses to generate immune memory. As such, it is vital to understand host–pathogen interactions to ensure that vaccines are developed to stimulate the most appropriate and protective response for a long-lasting solution to NSVs. Moreover, given that NSVs have a multitude of ways in which they can co-opt or manipulate the host’s immune system to benefit viral growth and spread, it is additionally important to understand this interface to optimize treatment options and improve vaccine design and manufacture.
During the NSV infection, viral conserved components called pathogen associated molecular patterns (PAMPs) are recognized by host pathogen recognition receptors (PRRs), such as the retinoic acid-inducible gene-I (RIG-I) and toll-like receptors (TLRs) [11]. The activation of these innate sensing pathways eventually leads to the production of IFNs and cytokines/chemokines critical for efficient activation of adaptive immune responses (B- and T-cell responses) that help control and clear infection and produce immunological memory to rapidly respond to future infection. The detection of viral nucleic acid leads to the activation of latent transcriptions (IRF3, IRF7, and NFκB) and expression of type-I IFNs (IFNα and IFNβ) and proinflammatory cytokines (such as IL6 and TNFα) [12]. Type-I IFNs then act in an autocrine or paracrine fashion to stimulate the expression antiviral ISGs via STAT1/2 [12] (Figure 1).
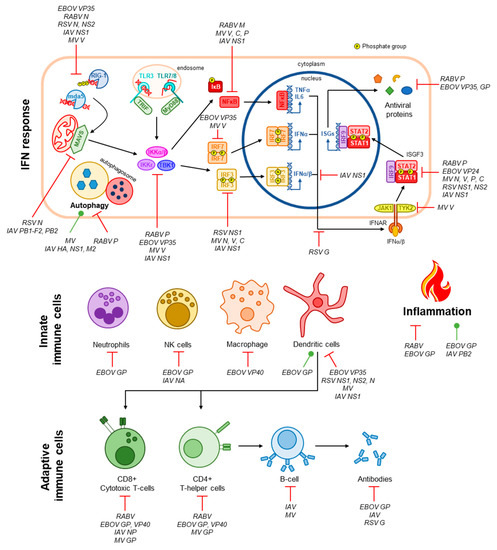
Figure 1. Immune evasion by NSVs. The IFN response is the primary antiviral pathway activated following virus infection. NSVs are detected by intracellular PRRs such as RIG-1 and mda5 in the cytoplasm or TLR3/7/8 in the endosomal compartment via interactions with viral RNA [12]. Signalling cascades involving MAVS (for RIG-I and mda5) or TRIF/MyD88 (for TLRs) result in the activation of the kinases IKKα/β/ε and TBK1 that subsequently activate the latent transcription factors IRF3, IRF7, and NFκB via phosphorylation [12]. These transcription factors promote the expression and secretion of proinflammatory and antiviral cytokines (TNFα, IL-6, and IFNα/β) [12]. IFNs signal in an autocrine and paracrine manner by binding to the IFNα/β receptor (IFNAR), resulting in the activation of the ISGF3 complex (STAT1, STAT2, and IRF9) through phosphorylation of STAT1 and STAT2 by IFNAR-associated kinases JAK1 and TYK2 [12]. ISGF3 then promotes the expression of antiviral genes [12]. Innate and adaptive immune cells, as well as inflammation and autophagy, which additionally contribute to viral clearance, are also depicted. Targeting of the antiviral immune response by NSVs, and the viral proteins involved if known, are indicated [33][34][35][36][37][38][39][40][41][42][43][45][44][46][47][48][49][50][51].
Therefore, the quality and magnitude of adaptive immunity is dependent on the innate immune response [13]. Supporting this, Nakaya et al. found that antibody titers at one-month post vaccination were positively correlated with early expression of type I IFNs associated genes [14]. Early induction of IFN was also reported to be important for the development of antibody responses in LAIV (live attenuated influenza vaccines) and TIV (trivalent influenza vaccines) vaccinated children [15]. TLRs have been shown to play an important role in both cell-mediated and antibody mediated protection in measles vaccine response. Secretion of type-I IFNs promotes the recruitment and activation of specialised immune cells that aid in the clearance of viral pathogens. Of this cell-mediated immune response, dendritic cells are central to bridging innate and adaptive immunity through their functions as antigen-presenting cells, leading to the activation T-helper cells that, in turn, activate humoral immunity via the production of a pathogen-specific antibody by B-cells [16]. Robust activation of T- and B-cells also leads to the generation of immune memory, a key requirement for vaccines to induce long-lasting immunity [17] (Figure 1). The importance of specific innate cell subsets such as natural killer (NK) and T follicular helper cells has been observed as correlates of protection in recipients of Ebola vaccine. Additionally, polymorphisms in dendritic cell-specific intercellular adhesion molecule-3 grabbing nonintegrin (DC-SIGN), a measles-specific receptor, may modulate cytokine responses to the measles component of the MMR vaccine [18]. Although the adaptive immune response has traditionally been the primary focus of vaccine development, these studies have highlighted the importance of innate immune responses after vaccination and infection. Thus, strategies can be developed to trigger specific innate pathways that can lead to stronger adaptive immune responses which are protective against infection.
T-cells and B-cells are critical components in adaptive immunity against IAV infection. CD4+ T-cells target IAV-infected epithelial cells through binding to MHC class II molecules and contribute to B cell activation promoting antibody production [19]. CD8+ T-cells differentiate into cytotoxic T lymphocytes (CTLs) and defend against IAV infection via producing cytokines and effector molecules in addition to direct cytotoxic effects on infected cells mediated by MHC class I [20]. Since cytotoxic T-cells target infected cells, and not the virus directly, T-cell mediated immunity typically provides protection without complete virus neutralization, allowing some degree of virus replication [21]. T-cell recognition of conserved viral antigens presented by antigen presenting cells (APC) can contribute to a more qualitative antibody response. However, current inactivated vaccines do not elicit a strong T-cell response, which may in part be overcome by the use of optimal adjuvants [22]. Polymorphisms in the signaling lymphocyte activation molecule (SLAM) and CD46 have been shown to drastically reduce MV-specific antibodies in individuals’ post-vaccination, which illustrates the importance of genetic variation in our immune cell surface markers on vaccine responses [23]. A correlation in the number of plasmacytoid dendritic cells and MV-specific antibodies has also been observed post-vaccination in infants, indicating another important link between the adaptive and innate immunity [24]. Induction of antibodies targeting conserved IAV antigens is desirable for vaccine responses with the potential to provide broad protection. Virus-neutralizing antibodies usually target viral surface antigens, for example the IAV haemagglutinin (HA) head domain. However, multiple immune mechanisms that do not result in virus neutralization can also contribute to heterosubtypic immunity against different subtypes of influenza viruses [25]. Ways by which the humoral branch of the vaccine response can also contribute to protection other than virus neutralization is through Fc receptor engagement via antibody-dependent cellular phagocytosis (ADCP) [26][27] or antibody-dependent cellular cytotoxicity (ADCC) [28][29][30], as well as antibody-dependent complement mediated-lysis (ADCL) [31]. Additionally, external factors that can modulate the effectiveness of the adaptive immune system, such as post-transplant immunosuppressant medication, can lead to a reduction in B-cells and protective antibody responses to MV over time [32].
As mentioned in Section 2, viruses must overcome robust immune defences in order to establish productive infection. The NSVs discussed in this manuscript expertly evade these responses through a multitude of mechanisms summarised in Figure 1 and reviewed elsewhere [33][34][35][36][52]. Understanding how these viruses evade these immune defenses, especially the host–pathogen interfaces involved, are integral to the development of efficacious vaccine strains both by reducing pathogenicity and ensuring formation of immunological memory. In this section, we highlight a few points of convergence where these NSVs target our immune responses and the implications for vaccine development.
The IFN response is the primary defense against viral infection. Two stages of this response that are commonly targeted by NSVs are proverbial ‘bottlenecks’, viral RNA sensing and the ISGF3 transcription complex (consisting of STAT1, STAT2, and IRF9). Viral RNA is detected by two families of pattern recognition receptors (PRRs), RIG-I-like receptors (RLRs), and toll-like receptors (TLRS). The RLRs RIG-I and mda-5 detect uncapped RNA and double-stranded RNA (dsRNA), respectively, in the cytoplasmic compartment [53]. Toll-like receptors (TLRs) instead sense viral RNA within the endosomal compartment, these include TLR3, which detects dsRNA, and TLR7 and 8, which detected single-stranded RNA (ssRNA) [54]. RLRs are the principal PRRs that detect the NSVs discussed in this entry [53] and, as such, each has a mechanism evading detection. In some cases, this is believed to be a ‘passive’ mechanism whereby the viral RNA is hidden from RLRs, such as by encapsidation by the RABV N protein and sequestration by EBOV VP35 [55][56]. RSV NS2 and MV V protein actively associate with RIG-I or MDA5, respectively, to inhibit its activity and RSV N sequesters MDA5 in viral inclusion bodies [51][57][58]. MV V also targets the phosphatases PPIα/γ and IAV NS1 targets the ubiquitin ligase TRIM25, both preventing their functions in the activation of RIG-I [59][60].
ISGF3 is responsible for the expression of hundreds of IFN-stimulated genes (ISGs), many of which have antiviral activity [61]. Thus, it is not unexpected that components of this complex, in particular STAT1, are common targets for viral IFN antagonists. The P gene products of both RABV (P1–P5) and MV (P, V, C) variously inhibit STAT1 function. RABV P1 binds to ‘active’, phosphorylated STAT1 (pY-STAT1) and excludes it from the nucleus, while the smaller P3 tethers pY-STAT1 to cellular microtubules to inhibit its nuclear import and additionally blocks its DNA-binding intranuclearly [62][63][64]. MV P associates with unphosphorylated STAT1 (U-STAT) to inhibit its phosphorylation and subsequent nuclear accumulation, and the V protein prevents phosphorylation of Tyk2, in addition to associating with Jak1, STAT1, and STAT2, to contribute to inhibition of ISGF3 activation and nuclear import [65][66][67][68]. The C protein instead targets pY-STAT1, inhibiting correct formation of STAT1 homodimers in response to the type-III IFN, IFNγ [69]. In addition, the MV N protein also contributes to this STAT1 blockade by inhibiting the nuclear accumulation of pY-STAT1 [70]. ISGF3 targeting by RSV, EBOV, and IAV are less multifaceted, RSV NS1 and NS2 target STAT2 for degradation, and IAV upregulates the expression of SOCS1 and SOCS3 that negatively regulated STAT signaling by dephosphorylating/inactivating JAK1 and TYK2 [71][72][73][74]. Finally, EBOV VP24 inhibits pY-STAT1 nuclear accumulation by competitively binding with the nuclear transport proteins importin-α1, α5, and α6 [75][76]; VP24 has also been found to bind to U-STAT1, but the contributions of this interaction to immune evasion are not yet known [77]. Importantly, inhibition of STAT1 contributes to the pathogenicity of all five viruses, evaluated through infection of STAT1 knockout mice or using mutant virus unable to target STAT1 [72][78][79][80][81]. Thus, disruption of the virus-STAT1 interface is central to the production of attenuated vaccines.
The NSVs discussed in this manuscript commonly target T-cells to prevent their antiviral immune functions and their ability to activate humoral immunity. During RABV infection, only transient infiltration of T-cells into the CNS is observed, this is believed to be due to the depletion of T-cell populations via upregulation of the immunosuppressive molecules FasL, B7-H1, and HLA-G on infected neurons [82][83][84]. MV inhibits the proliferation of uninfected T-cells at the cell surface involving the surface exposed GP complex, consisting of the HA and F proteins, though the specific mechanism is yet to be elucidated [85][86][87]. EBOV has similarly been shown to induce apoptosis of T-cells through interactions of its surface GP with TLR4 [88]. EBOV VP40 is also released from infected cells in exosomes, which have also been proposed to induce apoptosis in uninfected T-cells. While not targeting T-cells specifically, RSV inhibits the activation of T-cells by DCs via N protein, which localises to the surface of DCs and impairs formation of the immunological synapse through reduction of MHC clustering [89]. IAV also does not target T-cell directly, but its high mutation rate in immunological epitopes of its N protein have been shown to prevent recognition of infected cells by CD8+ T-cells [45]; this could possibly extend to evasion of CD4+ T-cells as well. In addition, IAV, RSV, and EBOV all suppress DC maturation, inhibiting their capacity to activate T-cells, while MV does not impact maturation, but the capacity for infected DCs to activate T-cells is greatly reduced [90][91][92][93][94].