1. Introduction of Tyrosine Kinase Inhibitors
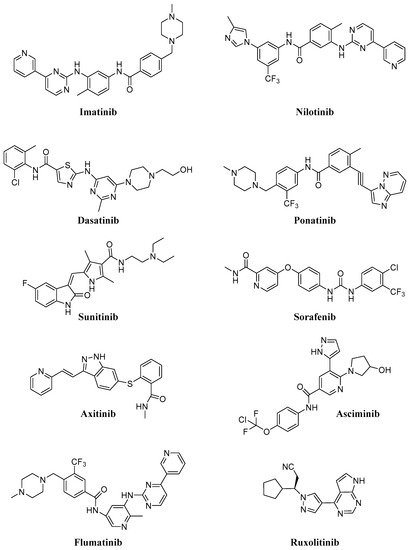
Intracellular protein tyrosine kinases, including Abelson (Abl), Src, JNK and many others, play a pivotal role in signal transduction pathways and cancer development, being highly activated in malignant tumor cells, but having very low activity and expression in normal cells [1]. Consequently, in the last thirty years, many small molecule tyrosine kinase inhibitors (TKIs) have entered in clinical trials and were approved to treat hematologic and non-hematologic tumors, thus improving cancer treatment. The majority of these molecules are ATP-competitive inhibitors and are not selective, acting also on receptor tyrosine kinases (in particular, platelet-derived growth factor receptor, PDGFR, and vascular endothelial growth receptor, VEGFR) or other intracellular kinases with different selectivity and potency. Unfortunately, all of these new compounds presented sub-optimal properties such as poor solubility (very high pH-dependent solubility), low oral bioavailability and severe adverse effects, which limited their clinical application; in addition, the onset of resistance became the biggest obstacle in clinical application for some of the new molecules (in particular for Imatinib,Figure 1).
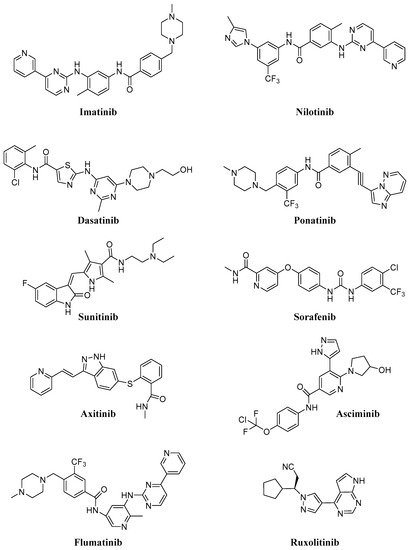
Consequently, in recent years many efforts have been made to find new molecules (e.g., Asciminib, Flumatinib; Figure 1) active on resistant CML (in particular on T315I mutation), for the treatment of different diseases (e.g., Ruxolitinib; Figure 1) currently without an effective therapy. In Table 1, selected TKIs (the most important for CML treatment and more recent and innovative than other ones) and their applications are reported. Issues related to solubility and resistance onset could be solved using safe and efficient delivery vehicles, that could improve the therapeutic efficacy, minimize toxicity, ameliorate tumor targetability and decrease drug resistance [2][3].
Consequently, in recent years many efforts have been made to find new molecules (e.g., Asciminib, Flumatinib;Figure 1) active on resistant CML (in particular on T315I mutation), for the treatment of different diseases (e.g., Ruxolitinib;Figure 1) currently without an effective therapy. InTable 1, selected TKIs (the most important for CML treatment and more recent and innovative than other ones) and their applications are reported. Issues related to solubility and resistance onset could be solved using safe and efficient delivery vehicles, that could improve the therapeutic efficacy, minimize toxicity, ameliorate tumor targetability and decrease drug resistance [2][3].
Table 1. Selected TKIs, their molecular targets, FDA approval years, number of clinical trials and treated diseases.
| Compound |
Target |
Number of Clinical Trials |
Diseases |
FDA Approval |
| Imatinib |
Abl, PDGFR, Kit |
754 |
CML, GIST, GVHD, many hematological and solid tumors |
2001 |
| Dasatinib |
Abl, PDGFR, Kit, Src |
320 |
CML, ALL, lymphoma, NSCLC and others solid tumors |
2006 |
| Nilotinib |
Abl, PDGFR, c-Kit, LCK, EPHA3, EPHA8, DDR1, DDR2, MAPK11, ZAK |
219 |
CML, ALL, GIST |
2007 |
| Ponatinib |
Abl, Src, FGFR, PDGFR, VEGFR, |
67 |
CML, ALL |
2012 |
| Asciminib |
Abl |
13 |
CML |
// |
| Flumatinib |
Abl, PDGFR, c-Kit, CSFR |
5 |
CML |
// |
| Sunitinib |
PDGFR, Kit, FLT3, VEGFR, CSF1R |
610 |
RCC, GIST |
2006 |
| Sorafenib |
PDGFR, c-Kit, FLT3, VEGFR, B-Raf |
870 |
RCC, liver and thyroid cancers |
2007 |
| Axitinib |
Abl, PDGFR, VEGRF, c-Kit |
161 |
RCC |
2012 |
| Ruxolitinib |
JAK1, JAK2 |
258 |
Myelofibrosis, polycythemia vera, GVHD, many other different diseases |
2011 |
Imatinib (IM, Gleevec®, Glivec®) was approved for CML in 2001 and today represents the first-line therapy for this type of hematological tumor, being able to block phosphorylation of Bcr-Abl, a fusion protein kinase which plays a fundamental role in CML development [4]. As IM inhibits PDGFR and c-Kit, two other transmembrane TKs, it has been approved as frontline therapy for: (i) gastrointestinal stromal tumors (GIST), characterized by mutated and over-expressed c-Kit or PDGFR-b [5]; (ii) other myeloid malignancies and hypereosinophilic syndromes and (iii) systemic mastocytosis [6][7] Most of them are obviously focused on CML, but also on solid tumors, such as acute lymphoblastic lymphoma (ALL), GIST, melanoma, sarcoma, glioblastoma and papillary thyroid cancer; interestingly, some trials concern asthma (NCT01097694), chronic graft-versus-host disease (GVHD) (NCT01862965), steroid-refractory sclerotic/fibrotic type GVHD (NCT01898377), multiple sclerosis (MS) (NCT03674099) and COVID-19 (NCT04422678), this compound having good immunosuppressive properties.
Currently, 350 clinical trials (63 in recruitment) regarding Dasatinib are focused on CML, ALL, Hodgkin and non-Hodgkin lymphoma, neck, head, breast, NSCLC, melanoma, mesothelioma, ovarian, colorectal, glioblastoma and CNS tumors (Table 1). In addition, Dasatinib, also acting on PDGFR, Kit, Src, Tek and Btk [8], could be useful as an immunosuppressive agent for immunological disorders [9]. Nilotinib is currently being studied in 219 clinical trials (41 in recruitment,Table 1) to evaluate its efficacy in CML, ALL, GIST and sarcoma (soft tissue sarcoma) patients, but also Huntington’s (NCT03764215), Parkinson’s (NCT02954978) and different forms of dementia pathologies (NCT02947893, NCT04002674).
Sorafenib (Figure 1) is an approved pankinase inhibitor able to target the Ras/Raf/Mek/Erk cascade pathway, PDGFR, VEGFR1/2 and the c-Kit receptor, and to block cell proliferation of different solid tumors; in particular, hepatocellular carcinoma (HCC) [10]. However, its long-term application in clinical practice was hampered by serious dermal toxicity and drug resistance, low water solubility and the first-pass effect [11] and consequent low drug concentration in tumor tissue. In addition, it can induce paradoxical activation of the MAPK pathway in both malignant and normal stromal cells [12] and this fact in hepatic stellate cells (HSCs) leads to their activation with consequent liver damage. Other pankinase inhibitors (e.g., Sunitinib and Axitinib;Figure 1) have been more recently approved for advanced RCC, unresectable HCC, thyroid cancer and GIST, and many other clinical trials are ongoing also on different solid tumors and leukemia types [13][14].
Seventy-six clinical trials (31 in recruitment,Table 1) focused on CML, ALL and different solid tumors (as NSCLC, GIST, glioblastoma, breast and many others) are reported for Ponatinib, (Iclusig,Figure 1) [15], approved in 2012 for CML treatment. In 2013, the FDA temporarily suspended Ponatinib sales because of the risk of life-threatening blood clots and severe narrowing of blood vessels, but at the end of the same year, this suspension was partially lifted.
Very recently, Novartis announced the results of a phase III ASCEMBL study (multicenter, open-label, randomized study) regarding Asciminib (ABL001,Figure 1), a new Abl allosteric inhibitor; the study evaluated Asciminib administration in adult patients with Philadelphia chromosome-positive CML in chronic phase, previously treated with two or more TKIs for 24 weeks [16][17][18]. On the basis of these interesting results, the FDA has granted Fast Track designation for Asciminib. Now, 14 clinical trials (two of them completed,Table 1) are focused on this compound (alone or in association with IM or Nilotinib) for CML and other leukemic patients; only one clinical trial is focused on asthma treatment (NCT03549897).
Flumatinib (HHGV678,Figure 1) is an orally bioavailable TKI, recently approved in China [19]; it inhibits the wild-type and mutated Bcr-Abl, PDGFR and mast/stem cell growth factor receptor (SCFR and c-Kit). Up to date, five clinical trials (one completed,Table 1) regarding only CML are in progress.
Ruxolitinib (Jakafi,Figure 1) is a selective JAK1 and JAK2 inhibitor approved for myelofibrosis (2011), polycythemia vera (2014) and GVHD in adult and pediatric patients (2019), but now it is also under study for COVID-19 (NCT04414098, NCT04359290, NCT04348071), atopic dermatitis (NCT039208529) and vitiligo (NCT04530344) (Table 1).
Although new compounds are continuously placed on the market and many are effective against different mutations, problems regarding poor solubility, resistance and severe side effects are not completely overcome. In part, the evolutionary probability of resistance can also be overcome with the association of two or more compounds, but this approach does not seem to be conclusive; consequently, the advent of nanotechnologies seems to be of great importance. In addition, it is also possible that the administration of one single nanoparticle containing several drugs may be more effective than the administration of several nanoparticles each containing one compound [20].
2. Nanoparticles of Tyrosine Kinase Inhibitors
A major part of these new nanoformulations have been patented in the last ten years [21][22]; in general, IM and Dasatinib represent the most studied compounds, whereas new molecules, such as Asciminib, Axitinib and others, are less investigated. Interesting results have been obtained for Sorafenib, Ponatinib and Nilotinib, as reported below. Regarding the routes of administration, these nanocarriers are usually injected intravenously; recent reports describe alternative administration routes thorough intratecal [23] and subcutaneous injection [24].
2.1. Imatinib
IM was the first molecule in this series to be nanoformulated and received great interest from researchers. A lot of papers reported the use of IM-encapsulated NPs and demonstrated their efficacy; some of these studies are reported as examples of IM delivery using nanotechnology.
2.2. Dasatinib
Many patents focus on Dasatinib nanoformulations and most of them are innovative and very recent
[25][26][27]. As previously reported, a major problem for oral administration of Dasatinib is its poor bioavailability caused by a low solubility, inappropriate partition coefficient, low drug permeation through lipid membrane, first-pass metabolism, P-glycoprotein-mediated efflux and drug degradation in the gastrointestinal tract due to the pH of the stomach or enzymatic degradation
[28]. Animal data suggest that, due to an extensive first-pass effect, the bioavailability of Dasatinib is about 14–34%. Thus, limited aqueous solubility is the bottleneck for the therapeutic outcome of Dasatinib. The majority of Dasatinib nanoformulations have been developed to treat CML cell lines, but as reported below, also for solid tumor treatment. In addition, in the last years Dasatinib-loaded NPs have been developed for different diseases, in particular ocular diseases (proliferative vitreoretinopathy, PVR)
[29][30].
2.3. Nilotinib
Nilotinib (Tasigna
®) is a recent pankinase inhibitor used for IM-resistant CML. In addition, a number of patents have been published on nanoformulations prepared to ameliorate Nilotinib activity and efficacy
[31][32].
Very recently, Koehl et al.
[33] explored the potential of lipid vehicles to improve the bioavailability of hydrophobic drugs such as Nilotinib, comparing a chase-dosing approach and lipid suspensions. To improve the dissolution kinetics, gastrointestinal absorption and bioavailability of some TKIs (including Nilotinib), Jesson et al.
[34] prepared hybrid NPs, consisting of amorphous TKI embedded in a polymer matrix; these nanosystems displayed an increase in Nilotinib release rate in both simulated gastric fluid and intestinal fluid, particularly when surfactants are present on the hybrid nanoparticle surface. The prepared hybrid NPs represent a promising approach to improve drug dissolution rate, gastrointestinal absorption and bioavailability following oral administration
[34].
Other targeted nanoformulations have been developed to minimize the resistance phenomenon and reduce cytotoxicity, not only for CML treatment, but also for application in different solid tumors. Recently, Fan et al.
[35] prepared collagenase I and retinol co-decorated polymeric micelles that possess a nanodrill-like and HSCs-targeting function based on poly(lactic-co-glycolic)-poly(ethyleneglycol)-maleimide (PLGA-PEG-Mal) (named CRM) for liver fibrosis treatment. These particular functionalized NPs could realize excellent accumulation in fibrotic liver and accurate targeting to activated HSCs in a mouse hepatic fibrosis model. Moreover, CRM loaded with Nilotinib showed optimal antifibrotic activity, suggesting that CRM is an efficient carrier for liver fibrosis drug delivery; in this study, the authors demonstrated that collagenase I, decorating NPs, could be a new strategy for building a more efficient HSCs-targeting nanodrug delivery system
[35].
In another work, wool-like NPs were developed to treat CML; in detail, a poly(ε-caprolactone) (PCL) nanosystem, composed of a biodegradable pH-sensitive core releasing Nilotinib and an enzyme-sensitive outer shell releasing IM mesylate, were prepared. This combinatorial delivery showed reduced IC
50 values on leukemia cells compared to single free drugs administration. In addition, in vitro results evidence a consistent drug release and a more therapeutic efficiency at a low dose with respect to the single-drug nanoformulation, confirming that both drugs reached the target cell precisely, maximizing the cytotoxicity and minimizing drug cell resistance
[36].
2.4. Ponatinib
As reported for Nilotinib, many patents were focused on nanoformulation of Ponatinib
[31][32][37] and different authors published various methods to obtain Ponatinib formulations
[38].
Targeted Ponatinib-loaded NPs have been recently investigated to evaluate their biological effect on osteosarcoma cell lines. In detail, Zinger et al.
[39] reported the design and synthesis of biomimetic/targeted NPs incorporating Ponatinib. These SLNs incorporate membrane proteins purified from activated leukocytes that enable immune evasion and enhanced targeting of inflamed endothelium. The NP formulations showed promising dose−response results in two different murine osteosarcoma cell lines, indicating efficient Ponatinib loading and a possible application for numerous therapeutic agents with toxicity profiles.
Kallus et al.
[40] encapsulated Ponatinib and Nintedanib into liposomes to obtain increased tumor accumulation/specificity and reduced side effects. Different methods of drug loading were tested and, interestingly, in an FGFR inhibitor-sensitive murine osteosarcoma transplantation model (K7M2), only liposomal, but not free, Ponatinib showed a significant tumor growth inhibition with reduced side effects.
2.5. Sunitinib
Regarding Sunitinib, a major part of efforts has been focused on the production of polymeric nanoparticles. In addition, a more recent Chinese patent is focused on PLA–PEG–PLA Sunitinib NPs
[41].
Otroi et al.
[42] prepared Sunitinib-loaded poly (3-hydroxybutyrate-co-3-hydroxyvalerate acid) NPs, obtaining dry powders after spray drying, and evaluated their cytotoxicity effects on A549 cells by MTT assay. This formulated inhalable powder could represent a promising medication for local therapy of lung cancer.
Nanopolymeric pharmaceutical excipients, such as CS nanoparticles, were synthesized and evaluated as in vitro drug release systems for Sunitinib
[43].
Shi et al.
[44] developed different targeted liposome formulations able to treat resistant breast cancer in vitro. In detail, targeted Sunitinib plus vinorelbine liposomes showed a good inhibitory effect on resistant MCF-7/Adr cells and represented a novel type of nanoformulations, which could accumulate in the resistant breast cancer cells.
In another study, the same authors developed a novel type of targeted liposomes by modifying a mitochondriotropic material (i.e., D-a-tocopheryl polyethylene glycol 1000 succinate–triphenylphosphine conjugate, TPGS1000-TPP), to encapsulate Sunitinib. Biological in vitro evaluations were carried out, in breast cancer cell lines (MCF-7 and MDA-MB-435S) and in vivo in mice. Targeted drug liposomes were internalized via cellular uptake and accumulated in the mitochondria of invasive breast cancer cells, inducing acute cytotoxic injury and apoptosis
[45]. Interestingly, other studies showed successful development of Sunitinib-loaded PLGA-NPs not only for cancer therapy, but also for neovascular age-related macular degeneration disease
[46].
2.6. Sorafenib
To overcome the delivery problems previously presented for Sorafenib, many efforts have been made to obtain different NPs, particularly SLN
[47], graphene nanosheets
[48], PSi and AuNPs in a polymeric nanocomplex
[49], PLA NPs
[50], hydroxypropylmethylcellulose (HPMC) or polyvinyl pyrrolidone and poloxamer NPs
[51], dextran and poly(-lactide-co-glycolide) [DexPLGA] NPs
[52]. Overall, these studies showed the importance of systematic formulation design to overcome poor solubility of the drug. In comparison with free Sorafenib, the majority of the reported Sorafenib NP formulations exhibited a significant increase in the retention time, a higher drug concentration in tumor tissues and an increased efficacy in inhibiting tumor growth.
Even more interesting results have been obtained with design, synthesis and biological evaluation of targeted Sorafenib nanoformulations. Wang et al.
[53] prepared PSi nanoparticles functionalized with a specific peptide able to direct Sorafenib to the tumor tissue and thus enhance the cellular uptake and drug delivery efficiency. In detail, the targeting peptides were obtained by azide alkyne cycloaddition click reaction, an important tool for surface modification of nanomaterials. The new Sorafenib-loaded targeted NPs efficiently delivered the drug into the cells, resulting in enhanced in vitro antiproliferative activity, and should represent an interesting system for targeted cancer therapy.
Hong et al.
[54] developed CXCR4-targeted NPs specific for activated HSCs in fibrotic livers. CXCR4 is a chemokine receptor induced in HSCs by various cellular stresses during the progression of liver fibrosis. As Sorafenib treatment could attenuate liver fibrosis and was associated with the inhibition of angiogenesis, the authors examined the anti-angiogenic activity of Sorafenib and Selumetinib (a MEK inhibitor) co-formulated in peptide-modified NPs (constituting PLGA, dipalmitoyl phosphatidylcholine, peptides (CTCE9908) and PEG). In mice with CCl
4-induced liver fibrosis, treatment with Sorafenib/Selumetinib-loaded CXCR4-targeted NPs significantly suppressed hepatic fibrosis progression and further prevented fibrosis and liver metastasis
[55][56].
Other polymeric or targeted NPs have been recently reported for the treatment of HCC. As an example, Yu et al.
[57] designed and synthesized bovine serum albumin (BSA)-coated zinc phthalocyanine (ZnPc) and Sorafenib NPs (ZnPc/SFB/BSA) able to trigger photodynamic therapy (PDT), photothermal therapy and chemotherapy. Upon irradiation at 730 nm, these NPs significantly suppressed HCC cell proliferation and metastasis and promoted in vitro cell apoptosis, with low toxicity and adequate blood compatibility. In addition, injection of ZnPc/SFB/BSA reduced tumor growth in a xenograft HCC model. All these results confirm that this type of nanoformulation could represent a promising strategy for HCC patients.
Recently, Li et al.
[58] developed new Sorafenib-loaded dendritic polymeric NPs with excellent stability, high cellular uptake efficiency in HepG2 human liver cells and higher cytotoxicity than free Sorafenib. Furthermore, this NP formulation inhibited tumor growth in mice bearing HepG2 xenografts, with negligible side effects, thus representing a novel approach for enhanced therapy of HCC.
Sorafenib-loaded polymeric NPs (constituted by TPGS-b-PCL copolymer) were synthesized from ε-caprolactone and D-α-tocopheryl polyethylene glycol 1000 succinate via ring-opening polymerization. The obtained NPs contained Pluronic P123 modified with anti-GPC3 antibody (NP-SFB-Ab) and displayed good stability, high drug release into cell culture medium and improved cytotoxicity in comparison with non-targeted NP-Sorafenib and the free drug. In addition, these targeted NPs significantly inhibited the growth of HepG2 xenograft tumors in nude mice without producing side effects. These findings suggest NP-SFB-Ab as a promising new method for achieving targeted therapy in HCC
[59].
The association of Sorafenib with other different therapeutic agents has also been investigated for HCC treatment. Cao et al.
[60] reported the co-delivery of Sorafenib and curcumin by directed self-assembled NPs. This nanosystem was prepared taking advantage of the hydrophobic interactions among Sorafenib, curcumin and the hydrophobic segments of PEG derivatives of vitamin E succinate. This innovative nanoformulation showed in vitro cytotoxicity and cell apoptosis in BEL-7402 and Hep G2 cells, in addition to a good antiangiogenetic action.
Zhang et al.
[61] reported Paclitaxel- and Sorafenib-loaded albumin nanoparticles to avoid taxol toxicities and to evaluate the anticancer efficacy of this combination. Interestingly, the authors obtained lower myelosuppression and hemolysis and an increased antitumor effect in animal models.
The co-delivery of plantamajoside (natural herbal medicines with excellent antiproliferative effect against many drug-resistant cancers) and Sorafenib by multi-functional PLA NPs was investigated to overcome drug resistance in HCC. NPs were produced and co-loaded with Sorafenib and plantamajoside and decorated with a polypeptide which specifically binds to biomolecules overexpressed on the surface of cancer cells. The authors demonstrated that this functionalization improved drug accumulation and penetration at tumor sites, resulting in a strong inhibition of tumor growth
[62]. Li et al.
[63] formulated a dual-targeting delivery system for enhanced HCC therapy by encapsulating Sorafenib and anti-miRNA21 (an antisense oligonucleotide with great potential in cancer therapy) in pentapeptide-modified reconstituted high-density lipoprotein NPs. In addition, these NPs expressed apolipoprotein A-I (ApoA-I) which specifically binds to overexpressed scavenger type B1 receptor (SR-B1) present in HCC parenchyma. This nanosystem was able to drive loaded drugs simultaneously to tumor neovascular and parenchyma, achieving precise delivery of therapeutics to maximize the efficacy. At the targeted sites, anti-miRNA21 would assist Sorafenib to exert powerful anticancer and anti-angiogenetic effects. The obtained results evidence that this chemo-gene system significantly increased Sorafenib action with negligible toxicity and reversed drug resistance, with improved efficacy in HCC
[64].
Other nanoformulations have been developed to target different solid tumors, such as renal cell carcinoma (RCC). Liu et al.
[65] prepared different Sorafenib-loaded PLGA, 1,2-dipalmitoyl-sn-glycero-3-phosphocholine (DPPC) liposomes, and hydrophobically modified chitosan-coated DPPC liposomes with good action against RCC 786-0 renal cancer cells. Poojari et al.
[66] assembled layer-by-layer (LbL) polyelectrolytes dextran-sulfate/poly-L-arginine with Sorafenib-encapsulated calcium carbonate NPs for oral cancer therapy. This innovative nanoformulation exhibited more potent antiproliferative, apoptotic and antimigratory activities in KB cells than the free drug, providing new insights for oral cancer therapy.