The bladder is an essential organ of the urinary system having major roles in temporary urine storage via immense folded internal linings, as well as its expulsion due to bladder musculature contractions and relaxations
[1][2]. The bladder is featured with the apex at the upper location, main body, triangular-shaped posterior fundus, as well as neck for convergence of fundus
[3]. BC is the common cancer of the urinary tract, originating inside the linings of the bladder consisting of urothelial cells
[4]. Urothelial cells are the source of connection between the kidney and bladder
[5]. BC is the fourth most common cancer in men and tenth in women causing 15,000 deaths annually in the USA
[6]. BC includes a variety of forms, depending on how it develops in the bladder’s specific cells, i.e., urothelial carcinoma, squamous cell carcinoma, and very rare adenocarcinoma in mucus-secreting cells of the bladder
[7]. As far as symptoms of BC are concerned, it is often accompanied by hematuria, frequent painful urination, and pelvic pain
[8]. The mechanism besides the propagation of BC lies in the resistant mutations in the tumor suppressor genes
[9]. However, other risk factors include smoking, old age, chronic bladder inflammation, inheritance history, and exposure to certain chemicals and dyes
[4][10][11][12][13]. As far as a generalized diagnosis of the BC is concerned, it can be initially determined through cystoscopy by inserting a cystoscope tube having a lens into the urethra to examine structural changes. Cystoscopy can be modified via attaching a specialized tool for collecting a sample for biopsy determination. Furthermore, the urine sample can also be opted to collect for analysis of the cancer cells presence
[14][15]. After the confirmation of the presence of traces of cancer cells in urine confirming BC. Further preceded diagnostics can also be performed to examine the severity, and it includes CT scan, magnetic resonance imaging (MRI), positron emission tomography (PET), bone scan, and chest X-ray. The diagnosis of BC is challenging owing to the vast existence of gaps accompanying over-testing, over-diagnosis, over-treatment, non-specificity, and heterogeneous nature of malignant BC cells
[16]. However, treatment is varied according to the type and severity based on low grade (benign) and high grade (metastatic) BC
[8][17]. Therefore, the opted methods for BC therapy include surgery for removing cancer cells directly via transurethral resection of bladder tumor (TURBT), cystectomy, neobladder reconstruction, and ileal conduit
[18][19]. Chemotherapy for BC includes the use of combinatorial chemotherapeutic agents in the form of gemcitabine and cisplatin (GC), cisplatin, methotrexate, and vinblastine (CMV), and gemcitabine and paclitaxel (GP) directly in the bladder via intravesical chemotherapy or systemic chemotherapy
[17][20][21]. Radiation therapy uses beams of powerful energy, such as X-rays and protons, to destroy the cancer cells
[22]. Immunotherapy is the most used treatment protocol for BC via intravesical and intravenous methods
[23]. Intravesical immunotherapy can be done using the
bacillus Calmette-Guerin (BCG) vaccine to mediate the immune system reaction that directs germ-fighting cells to the bladder
[24]. However, intravenous immunotherapy can be performed through various immunotherapy drugs
[25]. Nevertheless, all these modalities methods are associated with an increased economic burden, non-patient compliance, and need for targeted delivery, and most importantly with the involvement of virulent factors in tumor suppressor genes
[26]. Chemotherapeutics agents utilized in chemotherapy are specifically associated with damaging cells in the bone marrow, intestinal mucosal linings and hair follicles, as well as developing severe infection and fatigue due to the depletion of leukocytes and red blood cells
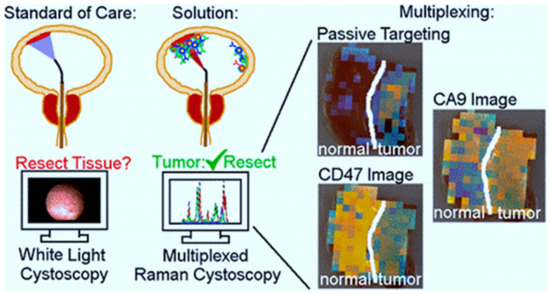
[27]. In terms of a generalized diagnosis of BC, it can be determined first by cystoscopy, which involves inserting a cystoscope tube with a lens into the urethra to investigate structural changes
[28]. Cystoscopy can be modified via attaching specialized tool for collecting sample for biopsy determination
[29][30]. Furthermore, urine sample can also be opted to collect for analysis of the cancer cells presence. After the confirmation of the presence of traces of cancer cells in urine confirming BC, further preceded diagnostics can also be performed to examine the severity and it includes CT scan, magnetic resonance imaging (MRI), positron emission tomography (PET), bone scan and chest X-ray
[31][32][33]. The diagnosis of BC is challenging owing to the vast existence of gaps accompanying over-testing, over-diagnosis, over-treatment, non-specificity, and heterogeneous nature of malignant BC cells
[34]. To overcome the limitations of conventional diagnostic methods for BC, a significant number of nanotechnology-based bioassays are highly encouraged
[35]. In this regard, fluorescent cystoscopy has been developed using 5 -aminolevulinic acid (5-ALA) phostosensitizer followed by intravesical administration, and have the capability of proficient absorption of cancer cells by showing intense red color compared to surrounding normal tissues
[36]. Similarly, ligand mediated approach-based nano-sensors are also of great interest as they can be developed by conjugating BC specified amino acid-based ligand PLZ4. PLZ4 functionalized nanomicelles preferentially enhance the uptake of only cancer cells under the mechanistic of photodynamic diagnosis
[37]. Role of gold nanoparticles (GNP) in the diagnosis of BCs by inducing plasmon resonance is irreplaceable and resulting in colors of visible difference to be observed by naked eyes
[38]. Cationic GNPs can be utilized with biocompatible anionic hyaluronic acid (HA) to produce visible blue color change
[39]. Ultra-small particles of iron oxide (USPIO) ranging from 30 to 50 nm in diameter have the capability of uptake by reticuloendothelial system for ultra-sensitive diagnosis
[40].
Nanotechnology advents the field of anti-cancer modalities via improving the drug loading by decorating the surface of nanoparticles with targeted receptor ligands, highly expressed on tumor surfaces
[41][42][43][44][45][46][47][48]. Nanomaterials bypass the side effects of conventional therapy by improving the specificity and pharmacokinetics of anti-cancer drugs
[49][50][51][52]. Anti-cancer NPs for treating BC are GNPs and they modified the acids and protein molecules for facilitating the rapid killing of cancer cells
[53]. GNPs help in providing stability, as well as a strong affinity for attachment of ligands targeting BC
[54]. Most effectively utilized nanocarriers in the treatment of BC include, polymeric nanoparticles because their synthesis is easy and cost-effective, provides superior viability and biodegradation
[55]. Polymeric nanoparticles utilized in the treatment of BC are available in a wide range of natural and synthetic polymers, constituting macromolecules poly (lactide-coglycolide), poly (lactic acid), poly (caprolactone), and chitosan
[55][56][57][58][59][60][61][62]. Similarly, the lipid-based nanoparticles are also imparting their role in treating BC by adapting formulation strategic forms of solid lipid nanoparticles (SLNs) and nanostructured lipid carriers (NLC) composed of phospholipids
[63]. Lipid-based nanoparticles are highly advantageous in encapsulating anti-cancer drugs and their site-specific loading via overcoming their solubility issues
[64]. Moreover, protein nanoparticles help in facilitating the targeted and controlled release of oral delivery using proteins such as albumin, gelatin, gliadin, and legumin
[65].