1000/1000
Hot
Most Recent

The abscopal effect (AbE) is defined as radiation-induced shrinkage of distant, non-treated, neoplastic lesions and it is considered the best clinical picture of the efficient immune stimulation by irradiation.
Head and neck squamous cell cancer (HNSCC) is the sixth most common cancer worldwide, more than 90% involving oral cavity, pharynx, or larynx. Known risk factors are excessive use of tobacco and alcohol, acquiring infection with human papilloma virus, especially HPV 16, HPV 18, and Epstein–Barr virus [1]. Radiotherapy represents a cornerstone in its management, and it is clinically implemented in different regimens; for locally advanced disease, modulated intensity radiotherapy (IMRT) is classically used, with daily doses ranging from 1.8 to 2.0 Gy, either alone or in combination with concomitant chemotherapy or cetuximab [2][3]. In recurrent or metastatic disease, the standard first line is platinum-based chemotherapy with 5-fluorouracil and cetuximab [4], however, stereotactic body radiotherapy (SBRT) with fractionation between 8 and 15 Gy is widely used [5]; in fact, thanks to its high spatial precision it could achieve a better control of local symptoms reducing toxicities. Its growing use increased reports of the abscopal effect as a systemic distant response of non-irradiated tumors or metastasis, as a consequence of proinflammatory changes in tumor microenvironment (TME) against cancer antigens [6][7]. A further boost has been given by the introduction of the immunotherapy targeting Cytotoxic T-Lymphocyte Antigen 4 (CTLA-4) and Programmed Death–Ligand 1 (PD-L1)/PD-1 axis: RT stimulates a robust tumor antigen cross-presentation in nodes while CTLA-4 blockade enhanced the priming of responsive T-cells in TME, highlighting an interesting clinical synergism. [8][9]. The goal of radioimmunotherapy should be to stimulate but also improve the duration of the immune response. Among various combination strategies, SBRT is most effective in inducing the abscopal effect, although the right dose and ideal fractionation has yet to be identified [9].
Radiotherapy immunogenicity is strictly related to tumor-specific characteristics, such as heterogeneity and radiosensitivity, and specific RT aspects like dose, fractionation, and timing of administration. Most of the clinical data regarding the use of radio-immunotherapy combinations are limited to either anti-CTLA-4 or anti-PD-1 agents: RT stimulates antigen cross-presentation and T-cell priming in draining nodes while CTLA-4 inhibitors enhance priming phase of effector T-cell activation induced by RT, leading to pro-immunogenic infiltrate of the TME. Blocking CTLA-4 enhances T-cell activation, increasing the CD8+/T-reg ratio, and strengthening the in situ vaccination effect [35][36][37][38][39].
PD-1 is expressed on T-cells, DCs, and NK cells: PD-1/PD-L1 pathway primarily inhibits T-cell proliferation by blocking cell-cycle progression, thus protecting tumor cells from T-cell attack. A recent study suggested that radiation-induced double-strand breakage of DNA results in upregulation of the expression of PD-L1 thanks to Ataxia-telangiectasia-mutated (ATM) and ataxia telangiectasia and Rad3-related (ATR) kinases [40][41][42][43]. Therefore, PD-L1 hyperexpression on cancer cells could be associated with a higher rate of responses to specific inhibitors while radiotherapy could act as a “Trojan horse” [42][43].
An excellent murine model published by Twyman-Saint Victor et al. clarified that radiotherapy and anti-CTLA4 monoclonal antibodies (mAbs) led to upregulation of PD-L1 on melanoma cells, mediating T-cell exhaustion and explaining at least in part the limited local and abscopal responses observed [44]. Anti-CTLA4 predominantly inhibits T-reg cells, thereby increasing CD8/T-reg ratio while radiation enhances the diversity of T-cell receptor (TCR) repertoire of intratumoral T-cells [44]. Addition of PD-L1 inhibitor reverses T-cell exhaustion, mitigates depression in the CD8/Treg ratio, and further encourages oligoclonal T-cell expansion [44]. Similarly to results from mice, patients with melanoma showing high PD-L1 levels on neoplastic cells did not respond to radiotherapy plus anti-CTLA4 mAb, demonstrated persistent T-cell exhaustion and rapidly progressive disease.
Evidence regarding the optimal timing, dose, schedules, sequences, and fractionation of radiotherapy are conflicting. Pre-clinical studies highlighted that starting anti-PD-L1 treatment 7 days following RT was inferior to starting on either the first or the last day [45]; however, some data also show how radiotherapy-anti PD-L1 sequence, with late administration of the checkpoint inhibitor, reinvigorates exhausted T-cells while an early sequence favors the differentiation and initial activation of T-cells [46][47]. Nowadays, it is clear that there is a synergism between immunotherapy and RT either as a single-fraction or in fractionated courses. Following irradiation with 12 Gy on 2 consecutive days, overall leukocyte and CD8+ T-cell frequencies peak at 5 days post-RT and then gradually decline to pre-RT levels [48]. Five days post-RT also reflects the highest CD8/T-Reg ratio, probably the ideal time-point for checkpoint blockade. Moreover, Frey et al. showed that after irradiation of 5 Gy × 2 fractions, CD8+ peak at day 8 and then decline while T-regs have a bimodal peak on days 8 and 10 [49]. Knowing the kinetics of infiltration of immune cells should be correlated with the time of administration of the ICIs, in order to achieve the maximum immunostimulant effect.
Hypofractionated radiotherapy (hRT) is the delivery of fewer, larger (>2 Gy) doses of radiotherapy and is a potential strategy for improving dose intensity. hRT appears particularly immunogenic: T lymphocytes, including Tumor-infiltrating lymphocytes (TILs), have generally been considered as highly radiosensitive [50][51], that is why it could be postulated that extending hRT schedules might be less immunogenic if administered in the period in which T lymphocytes, stimulated by RT/ICI combination, migrate to TME [50][51]. Following the experience of Frey [49], Zhang et al. compared a combination of anti-PD1 treatment and hRT with different schedules and equivalent biologically effective doses in mice affected by melanoma. Anti-PD1 antibody was given weekly while primary tumor was irradiated with 3 × 9.18 Gy in 3 or 5 days or with 5 × 6.43 Gy in 10 days [52]. All the combinations inhibited growth of irradiated primary and non-irradiated secondary tumors greater than hRT and anti-PD1 monotherapy; similarly, local and systemic tumor-specific CD8+ T-cell responses and TILs were also similar across short or extended hRT schedules [52]. Zhang’s experience also highlighted how regional and abscopal antineoplastic biological effects of the extended schedules are similar to the shorter ones only if the regional lymph nodes provide sufficient cancer-specific T-cells in the TME [52].
Historically, HNSCC was considered poorly responsive to high-dose hRT rather than low-dose hRT, however, low-dose schedules may induce lymphopenia and immunosuppression [53]. Morisada et al. analyzed immune correlates, primary tumor, and abscopal control rates as a result of two different radio-immunotherapy combinations of PD-1 monoclonal antibody with either daily low-dose fractionated radiotherapy (LDRT, 2 Gy × 10) or high-dose hypofractionated treatment (8 Gy × 2) in syngeneic mice. High-dose hRT did not affect peripheral and tumor-infiltrating CD8+ T-cells, reduced neoplastic accumulation of granulocyte-like myeloid suppressor cells, while T-reg lymphocytes were largely unaltered. Expression of IFN-responsive MHC class I peptides and PD-L1 were enhanced in tumors treated with 8 Gy × 2 compared to 2 Gy × 10 schedule. Functionally, tumor-specific CD8+-lymphocytes responses within tumor draining lymph nodes were enhanced following 8 Gy × 2 schedule but suppressed following 2 Gy × 10 irradiation [53]. When combined with PD-1 mAb, reversal of adaptive immune resistance was observed following 8 Gy × 2, but not following 2 Gy × 10, with subsequent enhancement of CD8+ cell-dependent primary and abscopal tumor response. These data strongly support that high-dose hRT preserves or enhances anti-tumor immunity compared to daily low-dose fractionated irradiation and, when combined with PD-1 inhibitor, reverses adaptive immune resistance, promotes anti-tumor immunity, and controls primary and distant lesions [53].
In order to determine the optimal dose for tumor and immunological response, Schaue et al. conducted a single fraction dose escalation study with doses ranging from 5 to 15 Gy and demonstrated that fractions of 7.5 Gy and above are immune-stimulatory, determining an increased number of tumor-reactive T-cells [54]. Instead a dose higher than 15 Gy in single fraction increased splenic T-reg fraction, while the same total dose fractionated boosted the number of effector T-cells in the spleen and decreased T-regs, with an optimal dose fractionation of 7.5 Gy × 2 [54]. Dewan et al. investigated three different regimens of radiotherapy (20 Gy × 1, 8 Gy × 3, or 6 Gy × 5) to obtain abscopal response in syngeneic mice models, with or without antiCTLA-4, finding that a significant AbE was only induced when RT was administered in fractionated schedules [55]. Additionally, observations by Vanpouille-Box, et al. suggest that AbE could only be achieved with hRT (8 Gy × 3) when combined with immune checkpoint inhibitors [32][33].
The systemic antitumor response of focal hRT combined with ICI may also be mitigated by the immunosuppressive properties of the non-irradiated distant tumors, that hinder T-cell entry and T-cell functioning [56][57]. In this regard, strategies that attempt to modulate the stroma of metastasis to improve T-cell infiltration are basic to invigorate the systemic antitumor response of combined hRT and immune checkpoint inhibitors. In fact, despite its very poor tumor-killing effect, LDRT is effective to T-cell recruitment [58][59]. Klug et al. have shown that LDRT (with one fraction of 2 Gy) may reprogram macrophages in TME, leading to the production of inducible nitric oxide synthase (iNOS), which normalizes tumor vasculature, thus promoting T-cell infiltration and enhancing the efficacy of adoptive T-cell therapy [58]. Moreover Yin et al. preclinically demonstrate that LDRT on established metastases, in combination with ICIs, significantly enhances the abscopal response to hRT treatment on the primary tumor compared to hRT/anti-PD1, hRT/LDRT, or LDRT/anti-PD1 combined treatments [60]. The enhanced abscopal effect was linked to an increased infiltration of CD8+ effector T-cells and an upregulated expression of T-cell-attracting chemokines, so localized LDRT to a second lesion should be indispensable for an enhanced systemic antitumor response, triggered by combined focal hRT and anti-PD1 therapy [60].
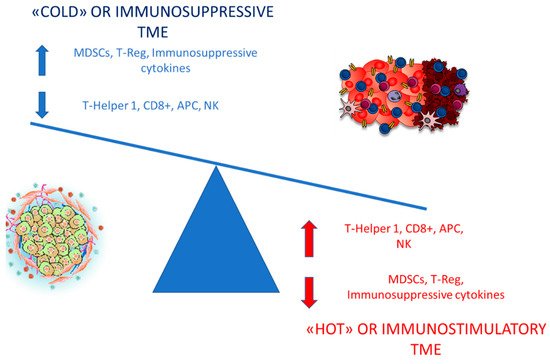
This preclinical model has been later confirmed by a post-hoc analysis of a 3 immunoradiation trial by Menon et al. in which patients, that received LDRT (1–20 Gy), either as scatter from high-dose radiation or from intentional treatment of a second isocenter with low-dose radiation, in association with high-dose radiation and immunotherapy, were evaluated for response [61]. The LDRT lesions were compared to those that received no radiation (<1 Gy total). They assessed that LDRT may increase systemic response rates of metastatic disease treated with high-dose radiation and ICI combinations, offering a clinical proof-of-principle of the ability of LDRT to polarize tumor macrophage in M1 subtype and shift TME from “cold” to “hot” [61][62].