Viral pneumonia is one the most frequent respiratory diseases among very young people and the elderly, contributing to an increase in the number of hospitalizations and deaths, mainly in subjects over 60 years of age. To assess the presence of pulmonary involvement and extension of disease, diagnostic imaging techniques are traditional chest radiographs (CXR) and computed tomography (CT). CXR may show a negative radiological pattern or otherwise areas of monolateral or bilateral consolidations, in association with nodular opacities, bronchial wall thickening, and small pleural effusions.
1. Introduction
Viral pneumonia is one the most frequent respiratory diseases among very young people and the elderly, contributing to an increase in the number of hospitalizations and deaths, mainly in subjects over 60 years of age
[1][2]. Many risk factors can predispose to the onset of a viral respiratory tract infection, such as immune system disorders, malnutrition in children, and tobacco smoking and chronic obstructive pulmonary disease (COPD) in adults
[3]. One of the major risk factors is immune system impairment; in fact, immunocompromised patients have a higher risk of developing a viral infection because of the decreased resistance and response to it
[4]. The immunocompromised patient category is broad, considering the high number of people with immunity deficits, mainly due to the advent of new therapies (including long-term treatments with immunosuppressive drugs, chemotherapies, and steroids)
[5][6]. The symptoms of viral infections are quite similar and usually non-specific despite the different aetiologies, including cough, fever, and dyspnoea, making a differential diagnosis difficult and dependent on the immune status of the host
[7]. The pathogens responsible for these diseases can be classified according to the immunocompetent or compromised status of the patient, more predisposed to pneumonia induced by specific viral agents, being divisible in atypical pneumonia in otherwise healthy hosts, and viral pneumonia in immunocompromised ones
[8]. The most common respiratory viruses in both categories are influenza, human parainfluenza (HPIV), adenovirus and respiratory syncytial virus (RSV), but in immunocompromised people there can also be infections due to cytomegalovirus (CMV), herpes simplex virus (HSV), and Epstein–Barr and Varicella-zoster viruses
[9][10]. Despite recent advances in diagnostic methods such as culture, rapid antigen testing, polymerase chain reaction (PCR) testing, and serologic analysis, specific viral diagnosis often remains difficult
[11]. Although radiologic imaging alone is not sufficient for the diagnosis, imaging is essential in association with clinical and laboratory testing. To assess the presence of pulmonary involvement and extension of disease, diagnostic imaging techniques are traditional chest radiographs (CXR) and computed tomography (CT). CXR may show a negative radiological pattern or otherwise areas of monolateral or bilateral consolidations, in association with nodular opacities, bronchial wall thickening, and small pleural effusions. Lobar consolidation is uncommon in patients with viral pneumonia, being more characteristic of bacterial forms
[12]. Chest CT is the gold standard for the evaluation of viral pneumonia showing different patterns, sometimes with nonspecific imaging findings
[12]. Table 1 summarizes the main CXR and CT patterns of the viral pneumonia from specific viruses described in the article’s images. (Table 1).
Table 1. Summary table with the main CXR and chest CT features of the viruses explained in the following figures in this review. CT: computed tomography; GGO: ground-glass opacities.
|
Virus
|
Chest X-ray Signs
|
Chest CT Signs
|
Figure in the Text
|
|
Sars-CoV-2
|
Lung subpleural consolidations, ground-glass opacities, nodules and reticular–nodular opacities, manifesting as interstitial pneumonia with diffuse alveolar damage
|
In the early phase, predominantly peripheral, bilateral GGOs, in association with limited consolidations, interlobular and intralobular septal thickening creating a “crazy-paving” pattern. Air bronchograms, vascular enlargement, halo sign, and reverse halo sign are also reported
|
Figure 1 and Figure 2
|
|
Influenza A
|
Bilateral reticular-nodular opacities in association with areas of consolidation, usually in the lower lobes
|
Multifocal consolidations and diffuse areas of GGO. Lymphadenopathy, cavitation, pleural effusion, and pneumatocele were also observed
|
Figure 3
|
|
H1N1 virus
|
Unilateral/bilateral GGO with or without associated areas of consolidation with predominantly peribroncho-vascular and subpleural distribution
|
Unilateral or bilateral GGO with or without associated areas of consolidation with predominantly peribroncho-vascular and subpleural distribution
|
Figure 4
|
|
Adenovirus
|
Bilateral and multifocal GGO with lobar or segmental involvement, similarly to bacterial pneumonia. In case of complication, unilateral small lung with hyperlucency and air trapping on expiration (Swyer–James Syndrome)
|
Bilateral and multifocal GGO with lobar or segmental involvement, similarly to bacterial pneumonia
|
Figure 5
|
|
Herpes virus
|
Bilateral areas of consolidation with GGO with lobular, segmental, or sub-segmental distribution
|
Multifocal areas of segmental or sub-segmental GGO are observed; pleural effusion is frequent
|
Figure 6
|
|
Varicella Zoster
|
Multiple nodules (5–10 mm) with defined margins that may tend to confluence. Pleural effusion and lymphadenopathy may be present although they are not common
|
Well-defined nodules (1–10 mm) with a halo of GGO. These millimetric lesions may calcify.
|
Figure 7
|
|
Cytomegalovirus
|
Diffuse and bilateral consolidations with interstitial involvement.
|
Interstitial and alveolar infiltrates, bilateral and asymmetric GGO areas in association with areas of parenchymal consolidation
|
Figure 8
|
|
Epstein-Barr virus
|
Lymphadenopathies with smooth interstitial parenchymal involvement in both lungs
|
Lymphadenopathies and less frequently interstitial infiltrates with diffuse GGOs and consolidations
|
Figure 9
|
2. Lower Respiratory Tract Viral Infections in Immunocompetent
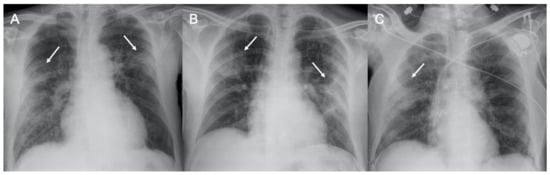
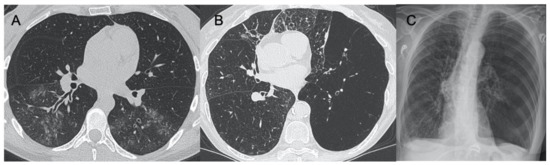
Figure 1. Chest radiograph in COVID-19 pneumonia. Three cases of supine chest X-ray with subpleural consolidations (arrows), in (A,B) with bilateral involvement, and in (C) with main involvement of the right lung.
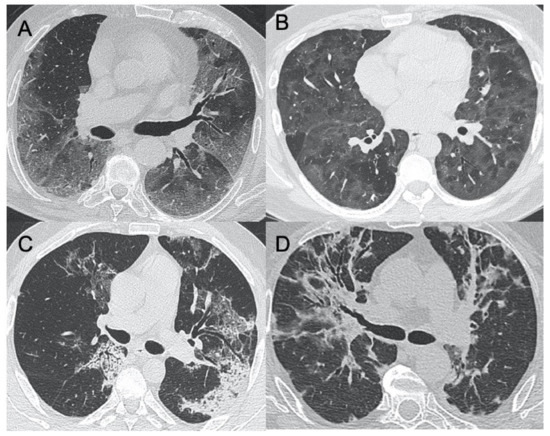
Figure 2. HRCT (High resolution computed tomography) in COVID-19 pneumonia. Diffuse ground-glass opacities involving both lungs (A) and with peri-lobular pattern (B) in the acute phase of the infection. (C,D) show two cases of sub-acute interstitial pneumonia, with decrease in ground-glass opacities and the presence of subpleural focal consolidations and thickening of the interlobular/intralobular interstitium.
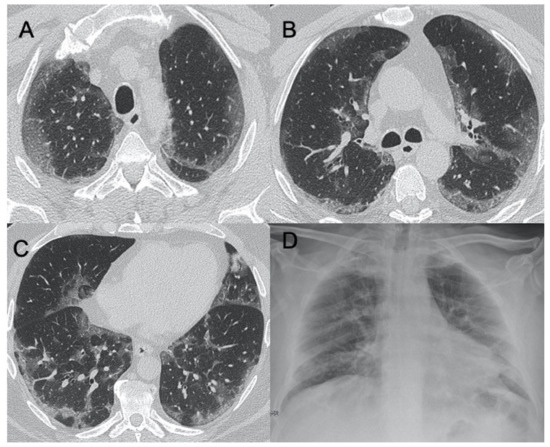
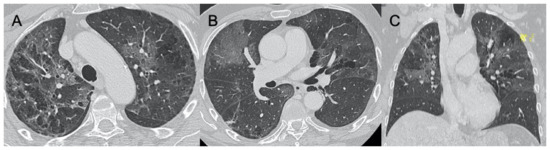
Figure 3. Influenza A. Figures in (A–C) show a case of influenza A with an interstitial pattern very similar to COVID-19: ground-glass opacities are mainly subpleural and bilateral, with a peri-lobular pattern of distribution. Figure (D) is a supine chest radiograph of the same patient, with diffuse interstitial involvement.
Figure 4. H1N1 interstitial pneumonia. These images (A–D) show a case of H1N1 related-pneumonia complicated in acute respiratory distress syndrome (ARDS), with diffuse and bilateral ground-glass opacities and traction bronchiectasis/bronchiolectasis.
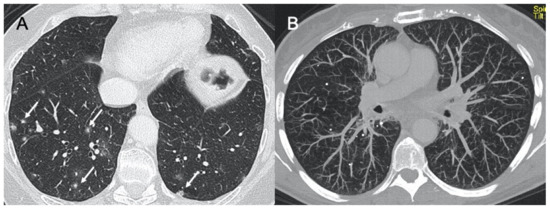
Figure 5. Adenovirus pneumonia and Swyer–James syndrome. Figure in (A) shows a case of acute adenovirus pneumonia, with typical multifocal and lobar ground-glass opacities, similar to bacterial pneumonia. Images in (B,C) show a case of long-term complication, a unilateral hyperlucent lung (Swyer–James–MacLeod syndrome).
3. Lower Respiratory Tract Viral Infections in Immunocompromised
Figure 6. Herpes virus pneumonia. A case of HSV (Herpes virus) (A–C) pneumonia with bilateral ground-glass opacities with patchy distribution, mainly in both upper lobes.
Figure 7. Varicella. A case of acute varicella pneumonia (A) with focal nodular consolidations (arrows) and its chronic form with small, tiny calcifications, well-visible in Maximum Intensity Projection (MIP) reconstruction (B).
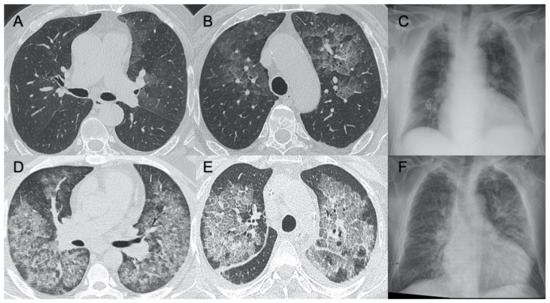
Figure 8. Cytomegalovirus pneumonia. Images in (A–C) show a case of mild parenchymal involvement on CMV pneumonia. Figures (D,E) show a patient with diffuse ground-glass opacities with a crazy-paving appearance, visible also in the chest radiograph (F).
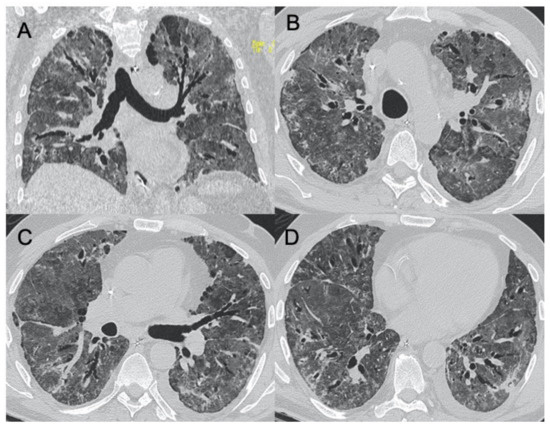
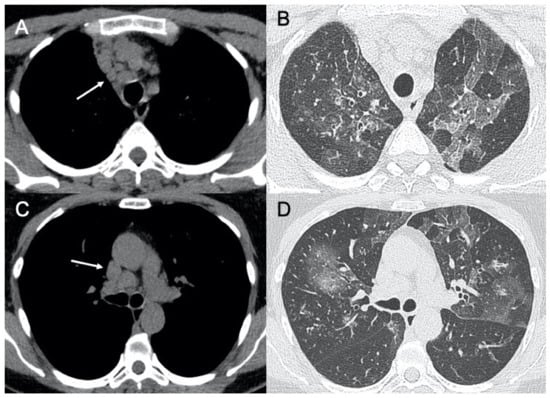
Figure 9. Epstein–Barr virus (EBV) pneumonia. A case of EBV pneumonia showing mediastinal lymphadenopathies (arrows in (A,C)) associated with focal, lobular ground-glass opacities in both lungs (B,D).
4. Conclusions
Last year has been a period characterized by the emergence of a new infection belonging to the coronavirus family, SARS-CoV-2, which has caused a severe worldwide pandemic with the need to develop effective methods in its diagnosis and evaluation, to ensure rapid management and treatment of patients affected by this pathology. Radiology has an important role in this task, being, together with RT-PCR nasopharyngeal and throat swab, the diagnostic method, especially in emergency departments, to provide a rapid assessment of pulmonary involvement. CXR is used in many countries, including Italy, as first-line imaging
[13][14]. Many recent studies indicate that CXR may not have the same power of CT, in terms of sensitivity, in the evaluation of pulmonary infection, but it still has an important role in the pandemic, especially for the greater complexity in being able to perform a CT investigation, regarding, for example, the need for disinfection after each examination performed to minimize the possibility of cross-infection, or for the higher radiation doses, especially in young patients
[15]. On the other hand, CT has a high sensitivity, around 97–98%, in assessing the presence of abnormalities that may represent pulmonary involvement, although it is not specific to this virus in identifying typical features
[16]. CT plays an important role in specific situations such as in the case of acute complications, for example, in the suspicion of pulmonary embolism or severe respiratory failure. Many other viruses belonging to different families in addition to COVID-19 can be responsible for the onset of pneumonia, both in immunocompetent and immunocompromised patients. Because of the great overlapping of manifestations that can occur on imaging, there is little sensitivity in differentiating radiological patterns resulting from viral infections. Although the diagnosis cannot be reached using diagnostic imaging alone, recognition of different patterns of lung involvement may help in differentiation among various viral pathogens. Radiologists can suggest the diagnosis of viral pneumonia, combining clinical and radiographic findings to substantially improve the diagnostic accuracy. Chest CT is the gold standard for the evaluation of viral pneumonia showing different patterns, sometimes with nonspecific imaging findings.