근전도 검사 (EMG)는 골격근에 의해 생성되는 전기적 활동을 평가하기위한 생체 전기 신호입니다. 근육 피로 연구에서 근육의 전기 생리 학적 측정은 골격근에서 전기 신호를 수집하는 데 중요한 역할을합니다. EMG 신호에는 일반적으로 일정량의 노이즈가 포함되어 있으므로 초기 단계에서 고품질 데이터를 얻는 것이 필수적입니다. 또한 사람들은 근육 수축 신호를 기록 할 때 통증이없고 편안한 방법을 선호합니다. 이 리뷰에서는 품질이 좋고 고통이 적은 EMG 데이터 수집 방법, 그 적용 및 실제 EMG 데이터 분석의 예를 다룹니다.
- biosensor
- wearable biosensor
- electrophysiology sensor
1. 근전도 검사
근전도 센서는 근육 세포의 자발적인 활동시 모터 유닛의 근육 섬유에 의해 생성되는 복합 전위 인 모터 유닛 전위를 감지하여 근육 활동을 분석 할 수 있습니다. 근육이 작동하려면 중추 신경계의 명령에 의해 생성 된 신경 물질에 의해 근육 세포에 전기 자극이 가해 져야합니다. 근육의 수축과 이완은 전기적 자극의 결과로 발생하며 이러한 현상은 여러 근육에서 발생하여 신체를 움직이게합니다 [ 4]. 우리의 뇌가 근육에 수축을 명령하면 뇌에 연결된 중추 신경계가 신경 전달 물질을 방출하고 이러한 물질을받는 뉴런은 근육에 전기 신호를 전달하여 신체를 움직이게합니다. 근육 세포에서 생성 된 전기 신호는 기계적 신호, 근육 수축 및 이완으로 나타나며,이 변환 과정을 여기-수축 커플 링 [ 5 ]이라고합니다. EMG 센서는이 과정에서 근육의 전기 신호를 측정하는 장치입니다. EMG 신호의 예로는 그림 1 과 같이 EMG 센서를 상완 이두근에 부착하여 1kg 덤벨로 근육이 수축 및 이완되었을 때의 원시 데이터를 측정했습니다.. 근육이 수축하면 근육이 이완되었을 때보 다 값이 더 컸습니다. 근육 수축 정도는 원시 데이터로 육안으로 확인할 수 있지만 정량적 평가를 위해서는 분석이 필요합니다. 근육 수축 정도를 확인하는 EMG는 주로 의학 및 생체 역학 연구 목적으로 사용됩니다 [ 6]. 의료 목적으로 특정 이유로 움직임이 불가능할 때 EMG 센서를 사용하여 신경계 문제로 인한 것인지 근육 자체의 손상으로 인한 것인지 진단합니다. 근육 기능 문제로 인해 근육이 수축하거나 이완 될 수없는 경우 EMG로 전기 신호를 측정 할 수 있습니다. 신경계에 문제가 발생하면 근전도 신호를 측정 할 수 없습니다. 또한 특정 동작 및 활동시 활성화되는 근육을 확인할 수 있으며이를 통해보다 효율적인 동작 및 활동을 연구 할 수 있습니다. EMG를 사용하면 특정 운동 중 근육 말초 및 중심 피로를 분석 할 수도 있습니다. 말초 피로로 인해 근육의 수축력이 감소하면 동일한 힘을 유지하려면 더 많은 전기 신호가 필요하기 때문에 EMG 신호의 원시 데이터를 늘려 피로를 측정 할 수 있습니다. 활동 전위와 여기가 중심 피로에 의해 전달되는 속도가 느려지면 전기 화학적 충격이 신경 경로로 전파되는 속도 인 전도 속도도 느려집니다. 근육 피로는 두 가지 유형의 피로의 조합이며 EMG 센서는 전체 피로 수준을 결정할 수 있습니다.7 ].
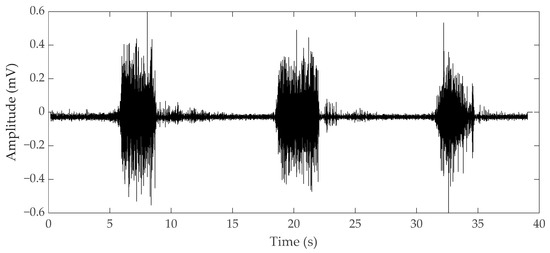
그림 1. 상완 이두근 수축 및 이완 동안 근전도 (EMG) 원시 데이터.
EMG는 비 침습적 측정 방법 인 표면 EMG (sEMG)와 침습적 방법 인 바늘 EMG의 두 가지 형태로 나타납니다. ( 그림 2 ) sEMG는 안정성 측면에서 큰 장점이 있기 때문에 더 널리 사용됩니다. 그러나 바늘 근전도는 바늘을 근육에 직접 삽입하므로 sEMG [ 8 ] 보다 정확한 결과를 얻을 수 있습니다 . 근통 증후군의 문제를 찾기 위해 트리거 포인트와 중추 신경계와의 관계를 조사하고 근전도 연구를 수행 한 결과 표면 기록 기술로는 필요한 근전도를 볼 수 없었습니다 [ 9 , 10 , 11]. Although there are limitations of sEMG in a specific field, the development of technology for sEMG is required for implementation in wearable sensors. Since the applicable fields differ depending on the type of EMG, we divided this section into needle and surface EMG to review the research on EMG currently underway.
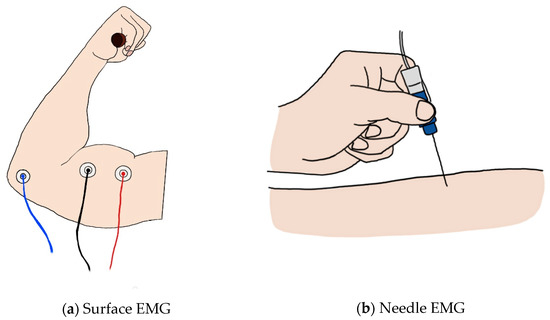
Figure 2. (a) Image of surface EMG: the red and black lines represent the + and − electrodes, and the blue line represents the ground; (b) image of the needle EMG.
1.1. Surface EMG
Surface EMG is the most widely known and used method in measuring muscle contraction. Electrical contributions made by the active motor units are measured in a noninvasive way on the skin using electrodes [7]. sEMG does not simply measure the electrical signals generated by the muscles; it represents the potential difference between two electrodes. If two electrodes are placed along muscle fibers at both ends of the motor for the muscle, the same muscle action potentials at both ends of the muscle are recorded at the same time, making it impossible to measure the potential difference. Therefore, the EMG signal is measured using a differential amplifier that rejects a common signal from both electrodes using two electrodes [12]. Since electrical signals exist even in muscles that are not in use, reference electrodes are required to exclude redundant signals. Finally, three electrodes must be attached to receive the EMG signal of one muscle. Through this process, sEMG can evaluate the contractile ability of one muscle from three signals.
In the early days of sEMG, it was used for biofeedback. For example, a study was conducted to reduce the frequency and severity of tension headaches through EMG biofeedback, and another study found that the resting level of frontalis EMG activity is higher in tension headache patients than in the general population. From this, it was argued that contraction headaches caused by constant contractions of the scalp and neck muscles could be relieved by learning to relax these muscles through biofeedback [13]. In another study, when biofeedback was given through computerized electromyographic evaluation of pelvic floor muscles, the subjective evaluation of pain decreased by 83% after 16 weeks and the resting tension level decreased by 68% [14]. However, in the above study, since only the amplitude of the simple EMG value was used to check the contraction degree of the muscle and proceeded with biofeedback, more detailed EMG parameters were studied to evaluate the muscle performance.
To obtain the parameters, EMG data are mainly analyzed in two domains: a time domain where EMG data can be viewed over time and a frequency domain that can check the frequency of EMG data within a certain range. In the time domain, the degree of muscle activation can be visually confirmed over time. Because muscles require a larger electrical signal to generate more force, they exhibit a larger amplitude in the EMG data. Therefore, it is possible to check the degree of activation for each muscle using the root mean square (RMS) value [15,16]. Fate analysis in the time domain is also possible. When a muscle continuously exerts the same force, a larger electrical signal is required to maintain the same output; therefore, the more fatigue it builds up, the greater the amplitude displayed. Fatigue can be analyzed with an increase in RMS indicating an increase in amplitude [17]. In addition, various parameters such as integrated EMG and maximum amplitude are used in the time domain [18]. In the frequency domain, fatigue is mainly analyzed. As muscle fatigue builds up, the speed of transmitting electrical signals slows down and the frequency is lowered, so that the conduction velocity slows down [19]. To capture this, fatigue is quantified by using parameters such as mean frequency, median frequency, and peak frequency in a specific range [18]. An example of EMG parameters for fatigue analysis can be seen in Figure 3.
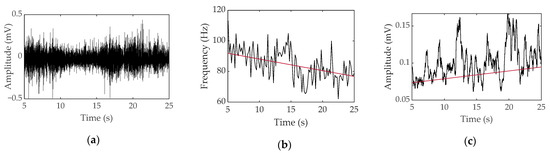
Figure 3. Surface EMG data obtained during voluntary contraction of a bicep with a 1-kg weight for a female: (a) raw data, (b) median frequency and linear regression, and (c) root mean square and linear regression.
Using these parameters, clinical studies have been conducted to measure muscle fatigue. Since the amplitude of EMG is different for each individual, fatigue was given using maximum voluntary contraction (MVC) and reliability was confirmed by analyzing the EMG parameters for fatigue (Table 1). Fatigue parameters were studied as RMS in the time domain, mean power frequency (MNF), and median power frequency (MDF) in the frequency domain, since the power spectrum frequency shift decreased. Mainly, the vastus lateralis (VL), rectus femoris (RF), vastus medialis (VM), lumbar 1–5, bicep brachii, and quadriceps were studied. Since the EMG signal has an accurate value when measured individually for one muscle rather than a complex signal of several muscles, it is limited to isometric contraction rather than dynamic contraction, which has a risk of complex measurement of several muscles. As a result of measuring EMG data during fatigue with isometric contraction, it was reported that most were reliable as indicators of fatigue, but due to the difficulty of application in dynamic contraction fatigue experiments and noise from electrode attachment, research on EMG continues.
Table 1. Reliability of EMG parameters for fatigue indices.
| Ref | Purpose | Electrode Location | Subjects | Experimental Method | Parameters Used | Conclusion |
|---|---|---|---|---|---|---|
| [20] 2000 |
Investigation of EMG variable (MNF, RMS) for valid indicators of muscular fatigue | VL, RF, VM | 11 males, 10 females | Repetitive maximum isokinetic knee extensions | RMS, MNF, MDF, torque, knee joint position |
MNF is a good criterion validity. |
| [21] 1999 |
Investigation reliability of sEMG | VL, RF | 9 males, 9 females |
Isometric knee extension | RMS, MDF, torque | MVC measurement is best suited for clinical applications from rectus femoris muscle. |
| [22] 1999 |
Correlation of EMG fatigue data in the lower back to the subject’s assessment of fatigue | L1, L5 | 25 males, 25 females |
Sørensen test | MDF, endurance time, Borg scale | The Borg scale correlated with endurance time and EMG median and mean power frequency slopes. |
| [23] 1982 |
Examination of the changes in frequency and amplitude of sEMG | Adductor pollicis, handgrip muscles, biceps, quadriceps | 6 males | MVC, fatiguing contraction (25,40,70% MVC) | RMS, center frequency | The center frequency of sEMG appears to be a good noninvasive index of muscle fatigue. |
| [24] 1979 |
Study of quantitative changes in the EMG pattern muscle fiber-type distribution | VL | 11 males | MV knee extensions | Integrated EMG, MNF | MNF decreases in FT-type muscles. |
| [25] 1986 |
Determination of the effects of motor unit recruitment and firing frequency on the surface EMG power spectra during sustained MVC and 50% MVC of the bicep brachii muscle | Bicep brachii | 12 males | 50% MVC | RMS, MNF | Increasing RMS EMG amplitude and decreasing MPF could better represent the MU activity during fatigue. |
| [26] 1994 |
Examination of the relationship between EMG manifestation of fatigue and endurance time during isometric contraction of the back extensors to fatigue | Erector spine at the levels of the 10th thoracic and 3rd lumbar vertebrae | 21 males, 208 females |
Sørensen test | MF, endurance time | MFgrad is a suitable technique for monitoring back muscle fatigue. |
sEMG has a limitation in that it is a noninvasive method that is not directly inserted into the muscle. Because of the noise caused by the electrode, which is an attachment type, and due to the muscle attachment position of the electrode, it affects the conduction velocity and median frequency, parameters of EMG [27]. Standardization of the attachment method and attachment location per laboratory was required. Therefore, a study on standardizing the electrode position was conducted to obtain accurate and repeatable data on the sEMG signal parameters. Recommendations for the use and technical considerations of sEMG and a questionnaire and interpretations required for the use of sEMG were presented [6]. Several researchers studied the standardized electrode locations. For example, to provide information on the degree of uniformity of the inner zone position of 13 superficial muscles in the lower limb, an experiment was conducted and the optimal electrode placement was between the inner zone and the tendon termination according to the landmark in eight of 13 muscles [28]. This placement was suggested by examining the muscle fiber orientation and palpable bony landmarks in the abdominal muscle [29]. The surface EMG for a Noninvasive Assessment of Muscles (SENIAM) project standardized the electrode attachment location and electrode size for concerted action in the Biomedical Health and Research program of the European Union [30]. However, even if the standard electrode location is used, the biggest drawback of sEMG is not compensated. The limitations from previous studies are presented in Table 2. Some obtained the same results as the isometric contraction in dynamic contraction, and some did not obtain valid data. The studies that did not obtain valid data from the isometric contraction suggested that the reason was due to the movement of various muscles rather than one muscle when performing a specific movement.
Table 2. Clinical studies conducted by measuring EMG during movement.
| Ref | Purpose | Electrode Location | Subject | Experimental Method | Parameters Used | Conclusion |
|---|---|---|---|---|---|---|
| [31] 1993 |
Investigation of EMG median frequency of calf muscles during an exhausting treadmill exercise | Right soleus, gastrocnemius medialis, gastrocnemius lateralis | 7 males, 2 females |
Uphill treadmill run till the moment of exhaustion | Heartrate, ECG, median frequency, | Immediately after the run, isometric median power frequency declined. |
| [32] 2007 |
Determination if a difference existed in the rate of fatigue of select shoulder muscles during isometric shoulder elevation and if the measured rate of fatigue was consistent from day to day |
Upper trapezius, middle deltoid, serratus anterior, lower trapezius muscles | 7 males, 9 females |
60% of their maximal voluntary isometric contraction force (MVIC) |
MPF | Middle deltoid appears to fatigue faster than the other shoulder muscles tested at the selected level of shoulder elevation. |
| [33] 2009 |
Determination of the difference in fatigue between athletes and non-athletes | VL, VM, RF | 11 males | Maximum versus forced repetition knee extension | Blood lactate, load in forced repetition, integrated EMG | Strength athletes produced neural fatigue in high-intensity resistance exercise. |
| [34] 1998 |
EMG assessment of back muscle function during cyclical lifting | Mind-belly of the longissimus thoracis, iliocostalis lumborum, multifidus muscles at L1, L2, L5 | 3 males, 1 female |
Dynamic and static lifting | instantaneous median frequency (Choi–Williams) | During dynamic contractions, instantaneous median frequency behavior is nonlinear and more complex than static contraction. |
| [35] (2005) |
Evaluation of handgrip forces using sEMG of forearm muscles | 6 forearm muscles | 8 males | Isometric gripping tasks | Grip force, normalized EMG | For standardized grips, valid predictions of grip based on EMG were produced. |
| [36] (2001) |
Evaluation of the potential health effects with respect to the low back of an office chair | L3, T10 | 3 females, 7 males |
Simulated office work on a chair | Exposure variance analysis | Trunk kinematics and erector spinae EMG were strongly affected by the task performed but not by chair type. |
When the EMG sensor is applied to a smart device, it is possible to recognize and prevent a muscle from being injured during exercise by monitoring the movement of the muscle. Since 70 years have passed since it was used for research, if a wearable sensor is made using the results of the research conducted so far, quality of life will be greatly improved. For example, there was a study that analyzed the frequency spectrum of electrocardiography (ECG) data that can detect EMG and EEG and can differentiate sleep states divided into four with 98–99% accuracy [37]. In addition, some studies have shown that driver fatigue can be measured by ECG and EMG [38,39]. In the case of drowsy driving, ECG and EMG can be developed for wearable biosensors to detect the risk of drowsiness at one of four levels and can greatly reduce accident rates. However, since sEMG and EEG need to have electrodes attached, they are inconvenient to wear and have not yet been commercialized due to noise problems. It was mainly analyzed only in the isometric contraction of a single muscle, and since dynamic movement appears when the movements of several muscles are integrated, it is difficult to measure accurate and significant data when performing dynamic movements. Also, a wireless sensor is essential for use outside the laboratory, such as running on a track or in a playground. Currently, a wireless sEMG sensor has been developed to analyze dynamic motion, but the noise that occurs in dynamic motion has not yet been resolved. For the EMG sensor to become a wearable sensor, it is necessary to solve the problem of noise generated on the surface electrode. The solution to this will be covered in detail in the section on noise below.
1.2. Needle EMG
Unlike surface EMG, needle EMG records the electrical activity of a muscle by inserting a needle electrode directly into the muscle or by obtaining the high-frequency electrical activity generated by moving the position of the needle electrode in the muscle and an electrical signal in a rest state [40]. The measurement of needle EMG by physical stimulation causes more severe pain than that of sEMG. In order to solve this problem, a study was conducted to investigate the pain of needle EMG [41], which can be divided into two types: a concentric needle electrode and a monopolar needle electrode (Figure 4). In the former, the surrounding cannula is the reference electrode, and the latter is recorded through the surface electrode. The electrode for measuring needle EMG is mainly a concentric needle electrode that has a small recording area and can obtain a value that cancels out noise. Since needle EMG can measure accurate data, one unit of motion can be analyzed through action potentials obtained from muscle fibers that contract at a location very close to the needle electrode using triggered averaging and decomposition methods [42]. After inserting a needle to induce minimal muscle contraction, the motion unit potential is analyzed by continuously obtaining one and the same motion unit potential using amplitude triggering while gradually moving the position. Muscles are evaluated mainly by comparing the average duration and amplitude with normal values [43]. After that, multi-motor unit potentials (MUP) analysis was developed and a technique capable of simultaneously obtaining and analyzing multiple-MUP from one recording site became available and was applied [44]. The pain of needle EMG, which was caused by the movement of the existing electrode, is less than in the past with multi-MUP analysis, which is possible with one insertion. However, there are still various limitations.
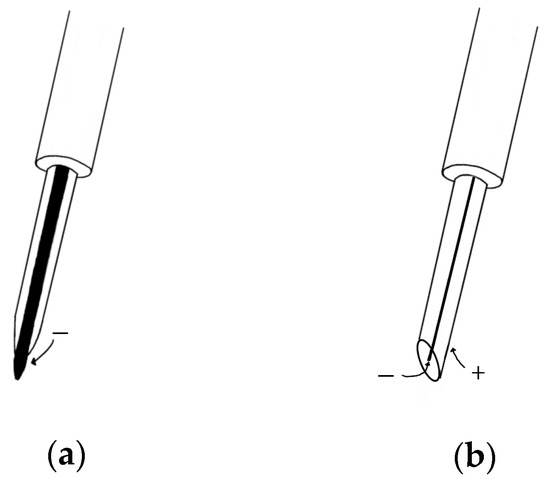
Figure 4. (a) Monopolar needle electrode; (b) concentric needle electrode.
Electrodiagnostic physicians should conduct a needle EMG test after checking the patient’s history based on clinical data. Care should be taken regarding some patients with skin infections, skin diseases, bleeding disorders, and obesity. Since there is a risk due to various variables such as muscle location and muscle size, needle EMG requires that the placement of a needle in the longitudinal midline of the muscle is accurately inserted into the muscle of interest. Instead of these drawbacks, it can be used as a measure of the accuracy of sEMG. For example, in the vastus intermedius muscle, sEMG was used to determine if the whole muscle could be used to assess neuromuscular activation. The observation of a good correlation could be used to assess total neuromuscular activation of the VL muscle during isometric contraction at low force levels [45]. There is also a paper on the feature extraction of a forearm EMG signal for prosthetics. EMG data analysis was conducted using both needle and sEMG for recording accuracy during hand movement [46]. For analysis of neuromuscular jitter that can be measured only in a single fiber, only needle EMG can be used [47,48,49] (Figure 5). EMG, which can obtain sensitive signals, is used for physiological analysis and diagnosis in a single motor unit during muscle contraction. Needle EMG is known to have a more accurate value than sEMG and is being used and studied. Needles have little noise, but considering the risk and difficulty of including them in a wearable sensor, it cannot be applied to the future development of biosensors. However, if the surface electrode is made in a way that reduces noise by bringing the reference electrode closer like a needle EMG to make it more accurate and easy to wear, it can be used in a wider range.
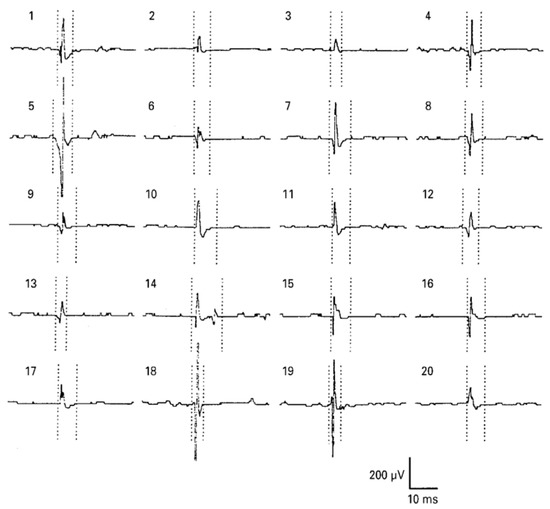
그림 5. 혀의 바늘 EMG : 건강한 피험자의 오른쪽 genioglossus 근육에서 모터 단위 활동 전위 (MUAP). MUAP 기간에 대한 마커는 5 개의 평균 MUAP 중 가장 오염되지 않은 것으로 설정되었습니다. BMJ Publishing Group Ltd.의 허가를 받아 [ 50 ] 에서 복제 됨 .
This entry is adapted from the peer-reviewed paper 10.3390/mi12010064
 Encyclopedia
Encyclopedia



