Malaysia is a rapidly developing economy experiencing a nutrition transition. It suffers from a double burden of over- and undernutrition, making it essential to understand diet quality in the population. In this scoping review, we have collated the existing literature on Malaysian diet quality, including factors that influence it, and the association between diet quality and health outcomes across the lifespan of Malaysians. Overall, diet quality was poor in all age groups studied. The Healthy Eating Index (HEI) and its iterations were predominantly used in urban and clinical settings to evaluate diet-chronic disease relationships. These indices were significantly associated with cardio-metabolic and disease risks in adults. The Diet Diversity Score (DDS) and Food Variety Score (FVS) were used to gauge diet quality in maternal and child nutrition studies and were associated with appropriate growth and caloric intake.
- diet quality
- diet index
- nutrition assessment
- diet variety
1. Introduction
2. Study Selection
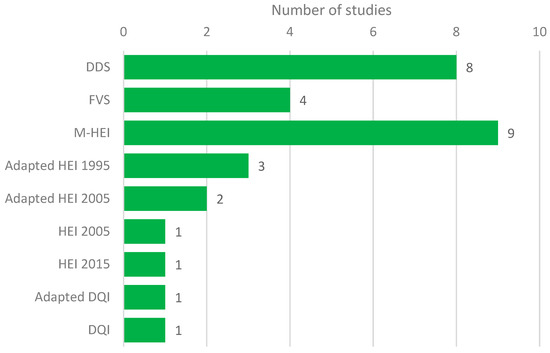
3. Diet Quality Measures and Status
4. Discussion
5. Conclusions
References
- World Bank. The World Bank in Malaysia. Available online: (accessed on 25 February 2021).
- Von Goh, E.; Azam-Ali, S.; McCullough, F.; Mitra, S.R. The nutrition transition in Malaysia; key drivers and recommendations for improved health outcomes. BMC Nutr. 2020, 6, 1–14.
- Shyam, S.; Khor, G.-L.; Ambak, R.; Mahadir, B.; Hasnan, M.; Ambu, S.; Chu, W.-L.; Aris, T. Association between dietary patterns and overweight risk among Malaysian adults: Evidence from nationally representative surveys. Public Health Nutr. 2019, 23, 319–328.
- Muda, W.A.M.W. The Hunger-Obesity Paradox in Malaysia. Available online: (accessed on 25 February 2021).
- Public Health Institute National Health and Morbidity Survey (NHMS). 2019. Available online: (accessed on 28 January 2021).
- Ministry of Health National Strategic Plan for Non-Communicable Disease (NSPNCD) 2016–2025. Available online: (accessed on 25 February 2021).
- United Nations International Children’s Emergency Fund (UNICEF). Malaysia’s Double Burden. Available online: (accessed on 25 February 2021).
- Hoffmann, I. Transcending reductionism in nutrition research. Am. J. Clin. Nutr. 2003, 78, 514S–516S.
- Yau, J.W.; Thor, S.M.; Ramadas, A. Nutritional Strategies in Prediabetes: A Scoping Review of Recent Evidence. Nutrients 2020, 12, 2990.
- Miller, V.; Webb, P.; Micha, R.; Mozaffarian, D. Defining diet quality: A synthesis of dietary quality metrics and their validity for the double burden of malnutrition. Lancet Planet. Health 2020, 4, e352–e370.
- Hiza, H.A.; Koegel, K.L.; Pannucci, T.E. Diet Quality: The Key to Healthy Eating. J. Acad. Nutr. Diet. 2018, 118, 1583–1585.
- Gil, Á.; De Victoria, E.M.; Olza, J. Indicators for the evaluation of diet quality. Nutr. Hosp. 2015, 31, 128–144.
- Dalwood, P.; Marshall, S.; Burrows, T.L.; McIntosh, A.; Collins, C.E. Diet quality indices and their associations with health-related outcomes in children and adolescents: An updated systematic review. Nutr. J. 2020, 19, 1–43.
- Alkerwi, A. Diet quality concept. Nutrition 2014, 30, 613–618.
- Wu, X.Y.; Zhuang, L.H.; Li, W.; Guo, H.W.; Zhang, J.H.; Zhao, Y.K.; Hu, J.W.; Gao, Q.Q.; Luo, S.; Ohinmaa, A.; et al. The influence of diet quality and dietary behavior on health-related quality of life in the general population of children and adolescents: A systematic review and meta-analysis. Qual. Life Res. 2019, 28, 1989–2015.
- Wirt, A.; Collins, C.E. Diet quality–what is it and does it matter? Public Health Nutr. 2009, 12, 2473–2492.
- Trijsburg, L.; Talsma, E.F.; De Vries, J.H.M.; Kennedy, G.; Kuijsten, A.; Brouwer, I.D. Diet quality indices for research in low- and middle-income countries: A systematic review. Nutr. Rev. 2019, 77, 515–540.
- Savy, M.; Martinprevel, Y.; Sawadogo, P.; Kameli, Y.; Delpeuch, F. Use of variety/diversity scores for diet quality measurement: Relation with nutritional status of women in a rural area in Burkina Faso. Eur. J. Clin. Nutr. 2005, 59, 703–716.
- Hiza, H.; Guenther, P.M.; Rihane, C.I. Diet Quality of Children Age 2–17 Years as Measured by the Healthy Eating Index-2010; United States Department of Agriculture: Washington, DC, USA, 2013.
- McCullough, M.L.; Feskanich, D.; Stampfer, M.J.; Giovannucci, E.L.; Rimm, E.B.; Hu, F.B.; Spiegelman, D.; Hunter, D.J.; A Colditz, G.; Willett, W.C. Diet quality and major chronic disease risk in men and women: Moving toward improved dietary guidance. Am. J. Clin. Nutr. 2002, 76, 1261–1271.
- Chong, S.P.; Appannah, G.; Sulaiman, N. Predictors of Diet Quality as Measured by Malaysian Healthy Eating Index among Aboriginal Women (Mah Meri) in Malaysia. Nutrients 2019, 11, 135.
- Pei, C.S.; Appannah, G.; Sulaiman, N. Household food insecurity, diet quality, and weight status among indigenous women (Mah Meri) in Peninsular Malaysia. Nutr. Res. Pr. 2018, 12, 135–142.
- Fokeena, W.B.; Jamaluddin, R.; Khaza’ai, H. Development and assessment of the reliability and validity of a diet quality index in a sample of Malaysia university students. J. Food. Nutr. Res. 2016, 4, 251–257.
- Kim, S.; Haines, P.S.; Siega-Riz, A.M.; Popkin, B.M. The Diet Quality Index-International (DQI-I) Provides an Effective Tool for Cross-National Comparison of Diet Quality as Illustrated by China and the United States. J. Nutr. 2003, 133, 3476–3484.
- Panagiotakos, D.B.; Pitsavos, C.; Stefanadis, C. Dietary patterns: A Mediterranean diet score and its relation to clinical and biological markers of cardiovascular disease risk. Nutr. Metab. Cardiovasc. Dis. 2006, 16, 559–568.
- Moazzen, S.; van der Sloot, K.W.J.; Bock, G.H.; Alizadeh, B.Z. Systematic review and meta-analysis of diet quality and colorectal cancer risk: Is the evidence of sufficient quality to develop recommendations? Crit. Rev. Food Sci. Nutr. 2020, 1–10.
- Hatløy, A.; E Torheim, L.; Oshaug, A. Food variety—A good indicator of nutritional adequacy of the diet? A case study from an urban area in Mali, West Africa. Eur. J. Clin. Nutr. 1998, 52, 891–898.
- Haghifar, S.; Jamshidi Naeini, Y.; Esmaeil Akbari, M.; Abdollahi, M.; Shadnoush, M.; Ajami, M.; Davoodi, S.H. Relationship between diet diversity score and breast cancer risk. Tehran Univ. Med. J 2018, 76, 550–557.
- Innovation, V.H. Covidence Systematic Review Software. Available online: (accessed on 28 January 2021).
- Chua, H.S.; Ali, A.; Zakaria, N.S.; Yusof, H.M. Assessment of diet quality and its association with nutritional status among fishermen’s children in Terengganu. Malays. Appl. Bio. 2018, 47, 137–144.
- Shariff, Z.M.; Tham, B.L. Food security and child nutritional status among Orang Asli (Temuan) households in Hulu Langat, Selangor. Med. J Malays. 2002, 57, 36–50.
- Chua, E.Y.E.; Zalilah, M.S.; Chin, Y.S.; Norhasmah, S. Dietary diversity is associated with nutritional status of Orang Asli children in Krau Wildlife Reserve, Pahang. Malays. J. Nutr. 2012, 18, 1–13.
- Badari, S.A.Z.; Arcot, J.; Haron, S.A.; Paim, L.; Sulaiman, N.; Masud, J. Food Variety and Dietary Diversity Scores to Understand the Food-Intake Pattern among Selected Malaysian Households. Ecol. Food Nutr. 2012, 51, 265–299.
- Pondor, I.; Gan, W.Y.; Appannah, G. Higher Dietary Cost Is Associated with Higher Diet Quality: A Cross-Sectional Study among Selected Malaysian Adults. Nutrients 2017, 9, 1028.
- Khalib, M.K.N.; Manaf, Z.A.; Shahar, S.; Ludin, A.F.M. Delivery of healthy lunch to worksites: A two weeks pilot study in a sample of working adults in Selangor, Malaysia. Malays. J Nutr. 2018, 24, 575–585.
- Teng, N.I.M.F.; Shahar, S.; Manaf, Z.A.; Haron, H.; Ngah, W.Z.W. Fasting Calorie Restriction Improved the Quality of Dietary Intake among Aging Men in Klang Valley, Malaysia. Pak. J. Nutr. 2013, 12, 607–614.
- Karppaya, H.; Shariff, Z.M.; Ngan, W.L.; Azman, N.A. Nutritional status of orang asli (Che Wong tribe) adults in Krau Wildlife Reserve, Pahang. Malays. J Nutr. 2010, 16, 55–68.
- Karupaiah, T.; Swee, W.C.S.; Liew, S.Y.; Ng, B.K.; Chinna, K. Dietary Health Behaviors of Women Living in High Rise Dwellings: A Case Study of an Urban Community in Malaysia. J. Community Health 2012, 38, 163–171.
- Shariff, Z.M.; Sulaiman, N.; Jalil, R.A.; Yen, W.C.; Yaw, Y.H.; Taib, M.N.M.; Kandiah, M.; Lin, K.G. Food insecurity and the metabolic syndrome among women from low income communities in Malaysia. Asia Pac. J. Clin. Nutr. 2014, 23, 138–147.
- Sulaiman, N.; Shariff, Z.M.; Jalil, R.A. Prevalence, demographic and socio-economic determinants and dietary consequences of food insecurity in Kelantan. Malays. J. Consum. Fam. Econ. 2012, 15, 85–102.
- Mohamadpour, M.; Sharif, Z.M.; Keysami, M.A. Food Insecurity, Health and Nutritional Status among Sample of Palm-plantation Households in Malaysia. J. Heal. Popul. Nutr. 2012, 30, 291–302.
- Shariff, Z.M.; Khor, G.L. Obesity and household food insecurity: Evidence from a sample of rural households in Malaysia. Eur. J. Clin. Nutr. 2005, 59, 1049–1058.
- Ihab, A.N.; Rohana, A.J.; Manan, W.M.W.; Suriati, W.N.W.; Zalilah, M.S.; Rusli, A.M. The Coexistence of Dual Form of Malnutrition in A Sample of Rural Malaysia. Int. J. Prev. Med. 2013, 4, 690–699.
- Ihab, A.N.; Rohana, A.J.; Manan, W.W.; Suriati, W.W.; Zalilah, M.S.; Rusli, A.M. Assessment of food insecurity and nutritional outcomes in Bachok, Kelantan. J. Nutr. Food Sci. 2015, 5, 373.
- Rohana, A.; Ihab, A.; Manan, W.W.; Suriati, W.W.; Zalilah, M.; Rusli, A. Food Expenditure and Diet Diversity Score are Predictors of Household Food Insecurity among Low Income Households in Rural District of Kelantan Malaysia. Pak. J. Nutr. 2012, 11, 967–973.
- Yong, H.Y.; Shariff, Z.M.; Yusof, B.N.M.; Rejali, Z.; Tee, Y.Y.S.; Bindels, J.; Van Der Beek, E.M. Pre-Pregnancy BMI Influences the Association of Dietary Quality and Gestational Weight Gain: The SECOST Study. Int. J. Environ. Res. Public Heal. 2019, 16, 3735.
- Leiu, K.H.; Chin, Y.S.; Shariff, Z.M.; Arumugam, M.; Chan, Y.M. High body fat percentage and low consumption of dairy products were associated with vitamin D inadequacy among older women in Malaysia. PLoS ONE 2020, 15, e0228803.
- Nohan, A.F.; Adznam, S.N.A.; Jamaluddin, R.; Norazman, C.W. Diet quality and its associated factors among community dwelling older adults in urban district in Kuala Lumpur, Malaysia. Malays. J. Med. Health Sci. 2020, 16, 153–162.
- Jamil, N.A.; Ling, C.J.; Ibrahim, H.I.M.; Hamzaid, N.H.; Chin, K.Y.; Yong, C.K. Nutritional and bone health status in young men with mild-to-moderate intellectual disability and without intellectual disability residing in community setting in Malaysia. J. Appl. Res. Intellect. Disabil. 2020, 33, 632–639.
- LS, K.N.; Mun, C.Y.; Zalilah, M.S. Diet quality and its relationship with overweight and laboratory parameters in breast cancer patients undergoing treatment. BMC Nutr. 2020. Preprint.
- Shahril, M.R.; Sulaiman, S.; Shaharudin, S.H.; Akmal, S.N. Healthy eating index and breast cancer risk among Malaysian women. Eur. J. Cancer Prev. 2013, 22, 342–347.
- Tiew, K.F.; Chan, Y.M.; Lye, M.S.; Loke, S.C. Factors Associated with Dietary Diversity Score among Individuals with Type 2 Diabetes Mellitus. J. Heal. Popul. Nutr. 2014, 32, 665–676.
- Shu, P.S.; Chan, Y.M.; Huang, S.L. Higher body mass index and lower intake of dairy products predict poor glycaemic control among Type 2 Diabetes patients in Malaysia. PLoS ONE 2017, 12, e0172231.
- Siddiqui, S.; Zainal, H.; Harun, S.N.; Ghadzi, S.M.S. Diet quality and its association with glycemic parameters in different diabetes progression stages. A cross-sectional questionnaire study at a primary care clinic. Clin. Nutr. ESPEN 2020, 39, 165–172.
- Appannah, G.; Emi, N.A.; Yusin, N.A.A.; Gan, W.Y.; Shariff, Z.M.; Shamsuddin, N.H.; Zaini, A.A.; Appukutty, M. Evaluation of dietary quality using Malaysian healthy eating index and its relationships with cardiometabolic risk factors in Malaysian adolescents. Malays. J. Med. Health Sci. 2020, 16, 46–55.
- The Economist Intelligence Unit Global Food Security Index (GFSI). Available online: (accessed on 25 February 2021).
- Habib, F.Q.; Dardak, R.A.; Zakaria, S. Consumers’ preference and consumption towards fast food: Evidences from Malaysia. Bus. Manag. Q. Rev. 2011, 2, 14–26.
- Galler, J.; Rabinowitz, D.G. The Intergenerational Effects of Early Adversity. In Progress in Molecular Biology and Translational Science; Akbarian, S., Lubin, F., Eds.; Academic Press: Cambridge, MA, USA, 2014; Volume 128, pp. 177–198.
- Khatun, W.; Alam, A.; Rasheed, S.; Huda, T.M.; Dibley, M.J. Exploring the intergenerational effects of undernutrition: Association of maternal height with neonatal, infant and under-five mortality in Bangladesh. BMJ Glob. Health 2018, 3, e000881.
- Martorell, R.; Zongrone, A. Intergenerational Influences on Child Growth and Undernutrition. Paediatr. Périnat. Epidemiol. 2012, 26, 302–314.
- Department of Statistics Malaysia. Household Income and Basic Amenities (HIS/BA) Survey Report of 2019; Deapartment of Statistics, Malaysia: Putrajaya, Malaysia, 2020.
- Imamura, F.; Micha, R.; Khatibzadeh, S.; Fahimi, S.; Shi, P.; Powles, J.; Mozaffarian, D. Dietary quality among men and women in 187 countries in 1990 and 2010: A systematic assessment. Lancet Glob. Health 2015, 3, e132–e142.
- Lee, T.T.; Norimah, A.K.; Safiah, M.Y. Development of Healthy Eating Index (HEI) for Malaysian adults. In Proceedings of the 26th Scientific Conference of the Nutrition Society of Malaysia, Kuala Lumpur, Malaysia, 24–25 March 2011.
- Lee, S. Revealing Malaysia’s Biggest Food Trends. Available online: (accessed on 25 January 2021).
 Encyclopedia
Encyclopedia



