1000/1000
Hot
Most Recent

Micronutrients have a potential interventional role to strengthen the immune system against the emerging infection caused by COVID-19.
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which belongs to the family of coronaviruses (CoVs), is the causative agent of pandemic coronavirus disease 2019 (COVID-19). There are four subfamilies of Coronaviridae, including the α, β, γ, and δ coronaviruses [1]. SARS-CoV-2 is a β-coronavirus and has a positive-sense single-stranded RNA genome [2]. CoVs can cross the species barrier and jump from mammals and birds to humans. The previous outbreaks of CoVs include those that caused the Middle East respiratory syndrome (2012) and severe acute respiratory syndrome (2002), known as MERS and SARS, respectively [3]. In December 2019, a flulike novel coronavirus, named SARS-CoV-2 and later found to be closely related to the MERS and SARS CoVs, emerged in Wuhan, China [4]. The World Health Organization (WHO) declared COVID-19 to be pandemic a month after its first outbreak because of the extremely high morbidity and mortality rates worldwide.
Presently, most of the drugs and vaccines for treating and preventing COVID-19 are still under trial, while the number of infected individuals continues to rise. There is no definite therapy for this novel infection, making it necessary to identify other options to control and prevent the escalating number of cases. An alternative approach that may help to combat this virus is to optimize the immune system. Many scientists have stressed the importance of nutritional intervention to improve the immune response. A well-balanced diet is essential for maintaining immune homeostasis. Any micronutrient deficiency may hinder the immune response against pathogens [5]. The ability of nutrients to protect against many infectious diseases and their role in reducing lung damage in pulmonary infections have been established in recent studies [6][7].
Based on the clinical manifestations, patients with COVID-19 are divided into three groups, presymptomatic, asymptomatic, and symptomatic [8]. The reasons why some develop severe disease and others do not are not entirely known; however, the immune system of an infected individual is one of the primary factors. When a virus infects an individual, a specific immune response is triggered, which is essential to eradicate the virus and prevent its progression. If the host immune system is weak, the virus will propagate and cause extensive tissue damage, especially in organs that express angiotensin-converting enzyme 2 (ACE2) receptors [9].
For the virus to enter host cells, the receptor-binding domain (RBD) of the viral spike protein binds to ACE2 receptors on host cells [9][10]. The virus can be taken up by antigen-presenting cells (APCs) such as dendritic cells and macrophages, which present it to the T cells. APCs contribute to the activation and differentiation of T cells and later to the massive release of cytokines. The host’s natural immune system recognizes viral components through pattern recognition receptors (PRRs) such as toll-like receptors (TLRs). Binding to TLRs induces the expression of inflammatory factors that can mediate lung inflammation and fibrosis [11][12].
Mast cells serve as a protective barrier against pathogens, and they also can be activated by a viral infection. Activated mast cells release histamines and proteases and trigger the release of proinflammatory markers, including IL-1, IL-6, and IL-33 [13]. These events lead to the activation of T cells and the massive release of cytokines, contributing to the amplification of the immune response. CD4+ or helper T cells stimulate the synthesis of virus-specific antibodies by activating B cells, whereas the function of CD8+ cells or cytotoxic T cells is to kill the virus-infected cells [11]. T helper cells also release chemokines and cytokines and provide signals to help monocytes and neutrophils reach the infected site, as shown in Figure 1 [14][15]. The extensive release of proinflammatory cytokines is known as a cytokine storm, leading to acute respiratory distress syndrome (ARDS) in these patients [16]. A primary cause of the high fatality rate of COVID-19 is the development of ARDS. The immediate release of free radicals and cytokines significantly increases oxidative stress, which is a hallmark of ARDS, causing cellular injury, multiple organ failure, and eventually death.
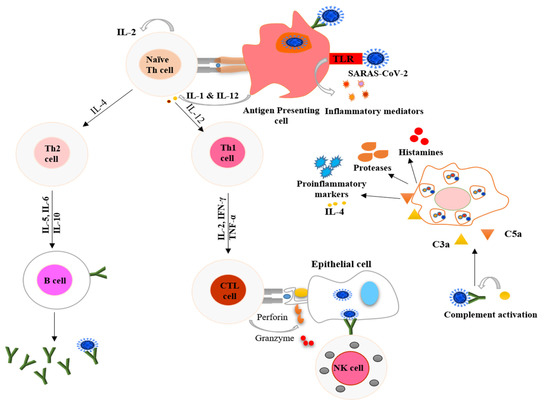
Figure 1. Schematic representation of processes used by the host immune system to combat COVID-19. The antigen-presenting cells (dendritic cells and macrophages) present the virus to naïve Th cells and stimulate the adaptive immune system. T cells also signal monocytes and macrophages to attract them to the infection site, where they release chemokines. Toll-like receptors (TLR) present on antigen-presenting cells recognize specific receptors on the virus and secrete inflammatory markers in innate immune system response. Mast cells activated by the pathogen release proinflammatory markers, proteases, and histamines. The upregulated secretion of proinflammatory markers causes a cytokine storm. IL-1 = interleukin 1; IL-2 = interleukin 2; IL-12 = interleukin 12; IL-4 = interleukin 4; IL-5 = interleukin 5; IL-6 = interleukin 6; IL-10 = interleukin 10, IFN-γ = interferon gamma; TNF-α = tumor necrosis factor alpha; CTL = cytotoxic T lymphocytes; NK = natural killer; C3a = complement component 3a; and C5a = complement component 5a.
Healthy and balanced nutrition is linked with strong immunity, and it represents our most potent tool in the ongoing COVID-19 crisis. Generally, poorly nourished individuals are at a higher risk of developing various types of infections [17]. Moreover, chronic and severe infections can cause nutritional disorders and worsen a patient’s nutritional status, making them susceptible to other infections. Thus, especially during the COVID-19 pandemic, it is imperative for everyone to monitor their diet and nutritional status [18]. Recent reports have identified certain groups at higher risk of COVID-19-associated complications, with the elderly and individuals with comorbidities such as hypertension, diabetes, and cancer more severely affected [19][20][21]. These risk factors are associated with malnutrition, which may alter the health status of the individuals.
In the absence of a specific antiviral therapy for SARS-CoV-2, several supportive and adjunct treatments are recommended. These include corticosteroid, ascorbic acid, anti-inflammatory, and interleukin-directed therapies. The overall aim is to manage the cytokine storm and the progression of infection [22]. The limited number of studies on the supportive care management of COVID-19 cases state that nutritional status should be assessed in all patients at the time of hospital admission. It is recommended that nutritional support be given to those in the high-risk group, asymptomatic carriers, and patients with moderate or severe COVID disease [23]. A variety of micronutrients strategies to treat COVID-19 have reached the clinical trial stage (Table 1). The immediate supplementation of certain nutrients in mild cases can prevent the progression of diseases.
Table 1. Examples of clinical trials on the use of vitamins against COVID-19 registered by the WHO [24].
| Trial ID | Study Design | Sample Size | Settings | Intervention in COVID-19 Patients |
|---|---|---|---|---|
| ChiCTR2000032400 | Cohort | 60 | China | High dose of vitamin C. |
| RCT20200401046909N1 | Randomized clinical trial | 260 | Iran | 1000 IUs of vitamin D daily for 8 weeks. |
| IRCT20180520039738N2 | Randomized clinical trial | 140 | Iran | Vitamin A (25,000 IU/day) for 10 days. |
| DRKS00021214 | Randomized clinical trial | 1300 | Germany | Vitamin B3 (nicotinamide) 1000 mg/day for 4 weeks. |
| EUCTR2020-001602-34-FR | Randomized clinical trial | 260 | France | A high dose of vitamin D (400,000 IU) versus a standard dose (50,000 IU) once daily for 14 days. |
| TCTR20200404004 | Randomized clinical trial | 400 | Thailand | Comparison of chloroquine, (10 mg base/kg) and vitamin C (1000 mg). |
| IRCT20170117032004N3 | Randomized clinical trial | 30 | Iran | Vitamin A (50,000 IU) along with routine treatment for 2 weeks. |
| CTRI/2020/06/026189 | Randomized clinical trial | 210 | India | Vitamin D (60,000 IU) single-dose and magnesium glycinate (250 mg bi-dose) for 14 days. |
| IRCT20200319046819N1 | Randomized clinical trial | 60 | Iran | Vitamin A (25,000 IU), Vitamin D (600,000 IU) once during the intervention, Vitamin E (300 IU) twice daily, Vitamin C (500 mg) five times a day, and Vitamin B (Soluvit ampoule) daily. |
| NCT04335084 | Randomized clinical trial | 600 | USA | Hydroxychloroquine, Vitamin C, D, and Zinc. |
| NCT04264533 | Randomized clinical trial | 140 | China | Vitamin C (12 g) twice a day for 7 days. |
IU, International units.
Micronutrient deficiencies suppress the immune system by altering the T cell- and antibody-mediated immune response and dysregulating the host immune system [25]. A balanced diet includes healthy portions of vegetables, fruits, nuts, legumes, whole grains, and moderate levels of dairy, fish, and poultry. It is recommended to limit the intake of sugar, refined carbohydrates, processed foods, and red meat. The fats consumed should include olive oils [26][27]. The rationale behind such a diet is that it will provide the necessary amount of healthy macronutrients, essential vitamins, and minerals and ensure an excellent metabolic state and maintain a healthy body weight [28]. Healthy eating provides necessary vitamins and minerals that produce sufficient numbers of immune cells and antibodies, resulting in better immunity, which prepares the body to fight off infections.