1000/1000
Hot
Most Recent

Coronavirus disease 2019 (COVID-19) has quickly become a worldwide health crisis. Although respiratory disease remains the main cause of morbidity and mortality in COVID patients, myocardial damage is a common finding. Many possible biological pathways may explain the relationship between COVID-19 and acute myocardial infarction (AMI). Increased immune and inflammatory responses, and procoagulant profile have characterized COVID patients. All these responses may induce endothelial dysfunction, myocardial injury, plaque instability, and AMI. Disease severity and mortality are increased by cardiovascular comorbidities. However, a marked fall in AMI admissions has been observed during lockdown, likely due, almost in part, to fear of in-hospital infection. Thus, attention should be also directed to psychological distress and fear, as COVID19 indirect effects on no-COVID diseases can be more harmful than the infection itself.
At the end of 2019, the new coronavirus SARS-CoV-2 was identified as the cause of an acute respiratory infection and cause of a worldwide pandemic. At the moment, there are many unclear issues related to the pathogenesis of the infection and the reasons underlying the extremely different clinical course, from asymptomatic to severe clinical manifestations, often carried out in a very short time period. The virus enters in several cell types, including cardiomyocytes following proteolytic cleavage of its S protein by a serine protease, and binding to the transmembrane angiotensin-converting enzyme 2 (ACE2) [1]. Moreover, whether it seems that pre-existing cardiovascular (CV) risk factors and disease may increase COVID-19 susceptibility, it has been also observed that patients with CV disease may experience more severe symptoms of infection [2]. In fact, the virus can worsen underlying CV lesions, precipitate de novo acute CV events, such as acute myocardial infarction (AMI), and induce CV chronic damage [3][4]. Thus, while the focus may be on the pulmonary system, it is important to be aware of the CV implications, which can be a significant determinant for complications and mortality associated with this virus.
Nonetheless, despite these common features and interactive factors, a significant decrease in patient admissions to intensive coronary unit (ICU) has been observed following containment measures, suggesting that other determinants may reduce the capacity to quickly manage acute patients who are simultaneously or not infected with COVID-19 [5][6][7][8].
Hence, we aim here to discuss how, besides common pathophysiological mechanisms linking COVID to CV disease and favoring acute events, other factors (e.g., fear of contagion, difficulty in contacting general practitioners, attention focused on COVID-19 patients, and a massive flow of health information and disparate viewpoints) may account for the unexpected and paradoxical decrease in AMI during lockdown, unlikely caused by a real decrease in the incidence of CV events. These reflections will help us to face a possible second COVID-19 pandemic wave or other outbreaks.
Healthcare practitioners all over the world have noticed a significant “AMI fall” during the COVID period. The number of emergency department visits in two major northern Italy referral hospitals (21 February–6 April) showed an inverse trend with daily COVID-19 mortality [9]. In Austria, a reduction of 40% in AMI admission was observed during March 2020 [10]. Data collected in the period January–March 2020 from nine high-volume USA centers, evidenced a 40% fall in the number of cardiac STEMI catheterizations [11]. The decrease was significant for STEMI (26.5%) and NSTEMI (65.1%), both in North Italy and in Central/South Italy [12]. Moreover, in a single large center in northern Italy, data obtained in March 2020 compared to March 2019 showed a significant reduction of 30% for STEMI, 66% for NSTEMI, and 50% for severe bradyarrhythmia [5]. These findings were confirmed by our experience, as we assessed a significant decline in STEMI admissions to the ICU-Cardiology Department of Ospedale del Cuore-Massa between 1 January and 10 June 2020, with respect to data collected in the same period in 2019 (Figure 1, panel A). Notably, in relation to fear, no patient with COVID-19 lab-confirmed infection was found between those admitted to our hospital, all swab-tested, until 10 June 2020.
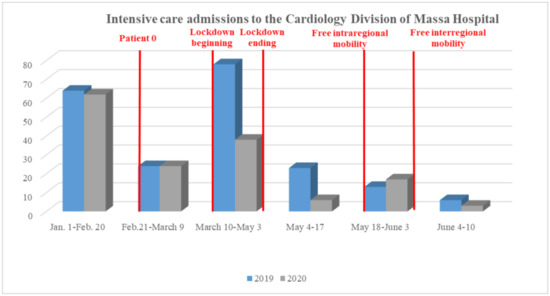
Figure 1. Comparison between 1 January–10 June 2019 versus 2020 segment elevation myocardial infarction admissions to the Ospedale del Cuore-Massa.
These data are worrying considering the result obtained in a small number of Chinese AMI patients (n = 7), which showed a great delay in the “symptom onset to first medical contact” time after control measure implementation, when compared to 2018–2019 (5 h versus an hour and a half) [13].
Table 3 shows key time points in STEMI care in the COVID period compared to pre-/post- outbreak periods (Ospedale del Cuore-Massa), where the major difference was observed in the time from “symptom onset to first medical contact”.
Table 3. Key time points (in minutes) in STEMI care (Ospedale del Cuore-Massa) before and after COVID-19 outbreak.
| 1 January– 21 February |
22 February– 3 June |
4 June– 10 June |
|
|---|---|---|---|
| Symptom Onset to First Medical Contact | 110 (15–570) | 133 (15–600) | 208 (15–1280) |
| Door to Hospital Arrival Time | 95 (25–405) | 94 (20–390) | 83 (20–390) |
| Hospital Arrival to Insufflation Time | 46 (15–120) | 38 (15–90) | 48 (15–120) |
The relationship between COVID-19 and AMI is supported by many clues (Figure 2). An increased risk of AMI is likely related to COVID-19 infection, due to the inflammatory response and hypercoagulability. Accordingly, abnormalities of cardiac troponins are the most common finding in COVID-19-affected patients. Patients with pre-existing CV disease and CV comorbidities may exhibit higher vulnerability to COVID-19 and a worse clinical outcome.
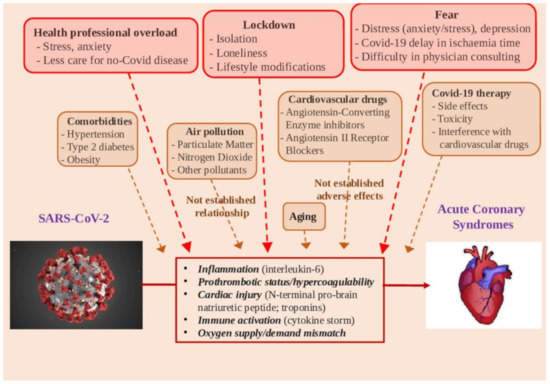
Figure 2. Potential determinants in the relationships between SARS-CoV-2 infection and acute myocardial infarction.
The relationship of air pollution with COVID-19 needs to be established, and together with an adequate collection of health data, environmental and demographic information are crucial for studying possible associations between exposure to atmospheric pollutants, diffusion, and severity of COVID-19. Importantly, although PM and nitrogen oxides are recognized as exacerbating risk factors for ACS, their levels were reduced due to the lockdown. In northern Italy, these decreases reached values of up to 58% and 38%, respectively, for nitric oxide and NO2, whereas PM10 and PM2.5 showed a smaller decrease since they are affected by secondary emissions even from long distances [14]. While it is plausible that the observed drop in concentrations of air pollutants may have contributed to a reduction in hospital admissions for AMI, this hypothesis, and the risk quantification, remains to be demonstrated by etiological design studies based on short-term exposure assessment.
Moreover, therapies under investigation for COVID-19 infection can have significant CV side effects.
However, at this point, it is particularly important to assess the role of psychological issues, such as distress and fear. In particular, it will be interesting to understand whether a patient’s fear may reduce AMI presentation, provoking a delay in appropriate and timely revascularization in the short-term, as well as long-term increased morbidity and mortality. Moreover, it is always possible that other (also actually unknown) reasons may affect the decrease in the incidence of AMI during the lockdown. As an example, it was recently hypothesized that increase in sleep duration in the time of COVID may positively impact overall health and beneficially contribute to the observed AMI reduction [15].
In this context, every effort must be directed to clear and reliable information for general audience patients, avoiding the spread of inconsistent or distorted news that can generate fear or false optimism. As the pandemic continues, public campaigns to raise awareness of ischemic symptoms should be reinforced, as the indirect effects of the COVID-19 pandemic on non-COVID diseases can be even more catastrophic than the infection itself.