Onychotillomania is defined as repetitive picking or pulling of the nail unit, causing damage to the nail matrix, nail bed, nail plate and/or periungual skin.
1. Overview of Onychotillomania
Onychotillomania is defined as repetitive picking or pulling of the nail unit, causing damage to the nail matrix, nail bed, nail plate and periungual skin. This behavior is self-induced using the patient’s own fingers and nails, though tools (e.g., scissors, nail files, knives) can also be used for nail manipulation
[1]. Onychotillomania is grouped with other BFRBs, including onychophagia, trichotillomania, and excoriation disorder. A variant of onychotillomania is habit tic, a nervous habit characterized by repetitive rubbing, picking, and pushing back the cuticle
[2]. Other related nail behavioral disorders include onychotemnomania (cutting nails extremely short), onychoteiromania (excessive nail rubbing until they become very thin), and onychodaknomnaia (nail biting causing painful pleasure)
[3][4].
2. Prevalence
The true prevalence of onychotillomania is unknown and likely underreported. Mild nail picking is relatively common in the general population, but only a small percentage experience considerable distress from excessive nail picking
[5][1]. In a cross-sectional study assessing for onychophagia and onychotillomania in 339 Polish medical students, 160 cases of onychophagia were noted, while only three cases of onychotillomania were reported, corresponding to a prevalence of 0.9%. The three students who reported nail picking (two females and one male) had a mean age of onset of 8.6 ± 2.3 years and duration of 14 ± 2.5 years
[6].
3. Psychiatric Classification
Onychotillomania has not been fully classified in the DSM-5. Like onychophagia, the DSM-5 does not include onychotillomania as a separate diagnosis. Nail picking may be categorized under “Other Specified Obsessive-Compulsive and Related Disorders”, specifically the BFRB disorders subsection
[7]. Onychotillomania has received less attention in the psychiatric literature compared to similar self-induced dermatological disorders, including trichotillomania and excoriation disorder
[8]. Nail picking is frequently omitted from BFRB questionnaires and participants with onychotillomania have been excluded from studies measuring validation of skin picking on a reward scale
[1][9]. Onychotillomania is underrecognized and underreported, likely because it is not uniformly recognized as a diagnosis in the medical literature.
4. Associated Disorders
Psychiatric disorders are often comorbid with onychotillomania, namely depression, anxiety, and psychosis. In 29 onychotillomania cases, eight were associated with depression with or without psychosis
[10][11][12][13][14][15][16], four with general anxiety disorder, adjustment disorder, or specific phobias
[6][17][18], and two with psychosis and hypochondrial delusions
[19][20]. In one case, there were no psychiatric comorbidities, and for the remaining 14 cases no psychiatric evaluations were performed
[21][22][23][24][25].
Nail picking is also associated with high levels of dissociation where patients have fragmented or no memory of their self-inflicted trauma. Higher levels of dissociation have been linked to more severe BFRBs, and onychotillomania has been associated with completed suicide in one case report
[12].
Certain rare congenital disorders have also been associated with onychotillomania. Smith–Magenis syndrome is a neurodevelopmental disorder characterized by developmental delay, intellectual deficiency, dysmorphic facial features, and behavioral abnormalities, including nail picking, finger and hand biting, head banging, and aggression
[3][26]. Onychotillomania can also be seen in patients with Lesch–Nyhan syndrome, an X-linked recessive disorder caused by a deficiency in the HPRT enzyme, which is responsible for purine recycling. Absence of the enzyme results in uric acid accumulation, leading to intellectual disability and self-injurious behavior
[3].
Dermatitis artefacta (DA) is a factitious disorder defined by self-inflicted injury with the intention of assuming a sick role without any external rewards
[8]. Individuals with Munchausen syndrome may have coexisting DA; however, nail and skin involvement are rarely seen in Munchausen syndrome
[27]. Patients with DA present with self-induced lesions that can mimic a variety of dermatologic disorders, including onychotillomania. The lesions are typically geometric and surrounded by normal-appearing skin
[8]. DA should be considered when patients present multiple times for the same problem, clinical findings are atypical in distribution and morphology, or the lesions do not respond to standard treatment
[8][28].
5. Clinical History
The diagnosis of onychotillomania is made clinically. Patients may report feelings of tension before and relief after nail picking. For some, nail picking is an unconscious behavior, leading many patients to deny their habits from poor insight
[6][1]. Patients who are fully aware of their nail picking behavior usually report multiple prior attempts to stop and are apologetic about their unwanted habits
[29]. Nail picking is rarely seen as the primary complaint and patients are often diagnosed incidentally during routine inspection of the nails
[3]. Patients with coexisting psychiatric conditions (i.e., obsessive compulsions, delusions of infestation) may be diagnosed a psychiatrist and referred to a dermatologist for their nail changes. Understanding the patient’s awareness of their nail-picking behavior, as well as psychiatric history, can direct the approach to treatment.
6. Physical Exam
A full examination of all twenty nails, skin, scalp, and hair is warranted in patients with a suspected diagnosis of onychotillomania and to assess for other coexisting BFRBs. For patients who are not aware or deny nail picking, careful observation for nail picking during the visit can provide evidence for the diagnosis
[3]. An abbreviated psychiatric examination is also recommended, as onychotillomania is associated with coexisting depression, anxiety, and psychosis. The clinical manifestations of onychotillomania are primarily depicted in case reports with limited definitions for symptoms and signs of disease
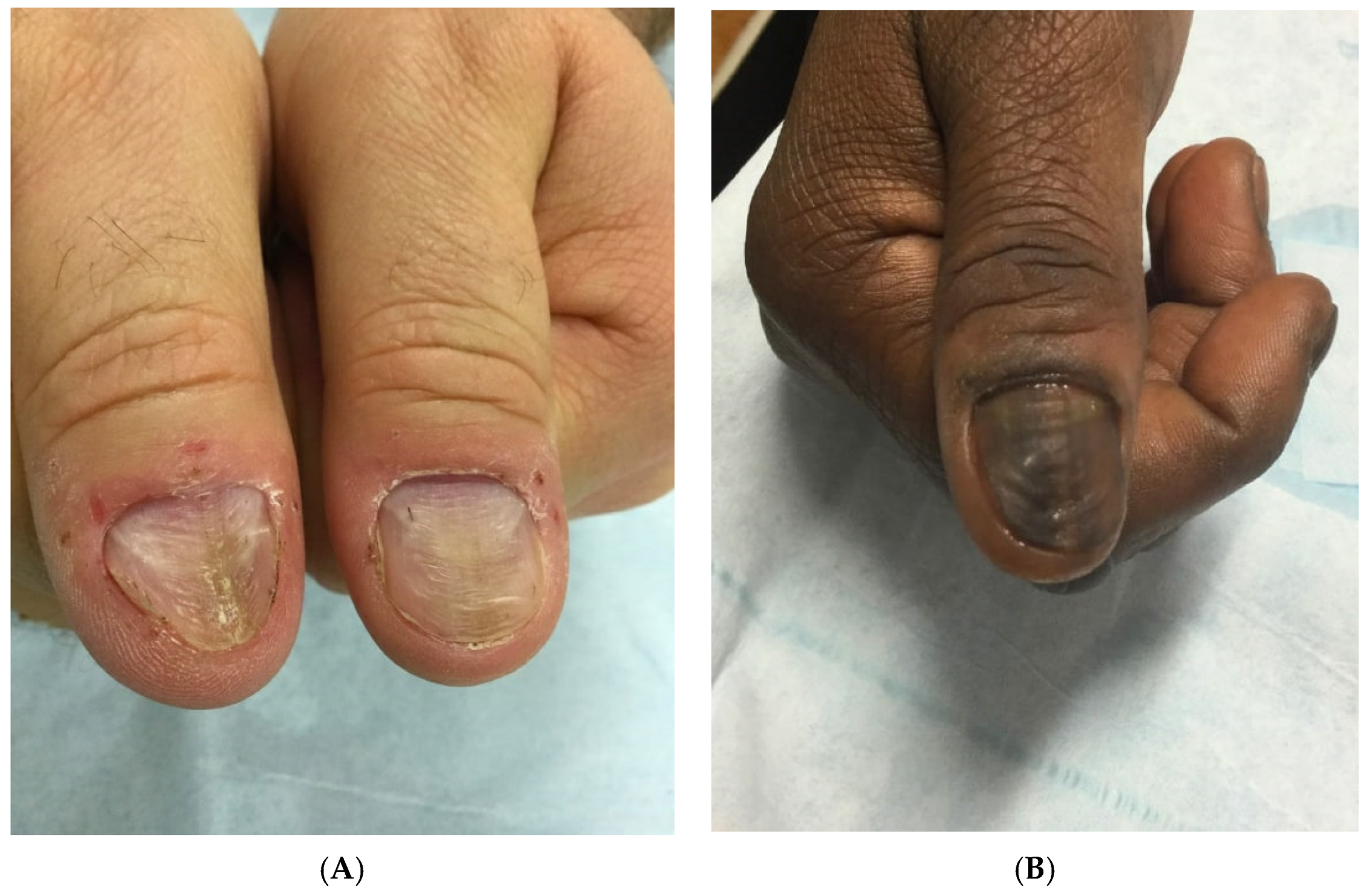
[30]. Clinical findings are often asymmetric, nonspecific, and bizarre-appearing. Common nail plate abnormalities include transverse ridges, thinning, macrolunula, and generalized dystrophy. Repetitive picking of the proximal nail folds can traumatize the nail matrix, resulting in nail plate ridging. A characteristic nail finding associated with onychotillomania is the habit tic deformity, characterized by multiple parallel transverse grooves, most commonly affecting the thumbnails (
Figure 1)
[8]. The periungual skin, particularly the nail folds and cuticles, can also be affected and can appear erythematous and tender, with crusts and erosions
[1].
Figure 1. (A) A 58-year-old nail picker with habit tic deformity of the bilateral thumbnails. There are parallel transverse grooves in the nail plate. (B) A 54-year-old nail picker with transverse grooves in the nail plate (habit tic deformity) and longitudinal melanonychia from chronic nail picking.
Dermatoscopic evaluation is helpful in distinguishing onychotillomania from other nail conditions. In a study characterizing the most common dermatoscopic features of onychotillomania in 36 patients, 69.4% had wavy lines (uneven longitudinal lines in different planes with a wavy appearance from uneven nail plate growth), 63.9% obliquely oriented nail bed hemorrhages, and 47.2% nail bed gray discoloration. These changes were not seen in nail lichen planus, nail psoriasis, or onychomycosis
[30].
A nail biopsy with histopathological analysis is rarely required for diagnosis for onychotillomania. However, it may be necessary in cases of severe onychodystrophy, without historical clues. Differential diagnoses include onychophagia, nail lichen planus, nail psoriasis, onychomycosis, acute and chronic paronychia, 20-nail dystrophy, and epidermolysis bullosa aquita
[8][3]. Pathological findings are often nonspecific, but can rule out other nail conditions. There is typically epithelial hyperplasia, acanthosis, and hyperkeratosis
[1][3]. Lichen simplex chronicus, or a thickening of the skin from repetitive rubbing or scratching, may also be seen
[21].
7. Complications
Long-term picking and manipulation of the nail unit can result in permanent nail dystrophy. Trauma to the proximal nail folds can cause melanocytic activation of nail matrix melanocytes, resulting in longitudinal melanonychia. These changes are usually permanent and do not reverse with the cessation of nail-picking behavior
[25]. Onychotillomania can be complicated by bacterial and viral infections, including acute bacterial paronychia, herpes simplex virus, and human papilloma virus
[3]. Chronic paronychia may also result from frequent manipulation of the nail unit. In severe cases of nail picking, pterygium, or anonychia, or complete loss of nail, can occur
[1][10].
8. Non-Pharmacological Treatment
Onychotillomania can be managed non-pharmacologically or pharmacologically. Supportive measures for treating onychotillomania are typically recommended as first-line therapy. Use of band aids and occlusive dressings have been efficacious in some cases
[23][24]. However, patients may find these bandages socially unacceptable or burdensome and therefore noncompliant. Another option is cyanoacrylate adhesive, also known as ‘super glue’. The product is applied once or twice a week over the cuticles of the affected nails, which serves as a protective barrier and a reminder to stop picking. In a case report of two patients using cyanoacrylate adhesives to treat onychotillomania, both patients ceased nail picking within three to six months and achieved normal-appearing nails
[31].
Behavioral modification using cognitive behavioral therapy (CBT) may increase awareness of nail picking
[32]. Since CBT has been used successfully to treat BFRBs, it may also be helpful for onychotillomania treatment. For example, in a clinical trial (
n = 16) using a CBT protocol originally designed for trichotillomania to treat skin picking disorder, 63% and 52% patients improved with individual and group CBT treatment, respectively
[33]. Another behavioral therapy used to treat onychotillomania is HRT. In one case report of a patient with onychotillomania treated with HRT, there was a reduction in nail-picking frequency from 8–10 h/day to 0–5 min/day, increased nail length, improved finger sensitivity, and less shame and embarrassment after 21 weekly sessions.
[11].
Given the potential comorbid psychiatric illnesses with onychotillomania, referral to a psychiatrist may be necessary. Dermatologists should inquire about intrusive thoughts, compulsions, and impact on QoL to determine if further psychiatric evaluation is warranted
[1]. A multidisciplinary approach to treatment can benefit patients who experience significant psychological distress.
9. Pharmacological Treatment
Results of pharmacologic treatment for onychotillomania are limited to a few case reports, as no large randomized controlled studies have been performed. NAC, which has not been studied for onychotillomania, is helpful for other BFRBs, so may be considered for onychotillomania management. Psychotropic drugs, including SSRIs, TCAs, and typical antipsychotics have been successful in treating nail picking; however, patients had comorbid psychiatric illness such as depression, OCD, or psychosis.
SSRIs and TCAs are not first-line treatments for nail picking, but may be beneficial in cases of comorbid depression or anxiety. In a case of onychotillomania with coexisting depression, one patient was treated with sertraline 150 mg/day. After four weeks, the patient’s depressive symptoms improved, with decreased nail picking, and resolution of both conditions at six weeks
[13]. Amitriptyline 50 mg/day improved nail picking in a patient with depressive neurosis after an unknown period of time
[15].
Antipsychotics can be used to treat nail picking in patients with comorbid psychosis. One patient with nail picking and comorbid trichotillomania and delusions of infestation was treated successfully with 200 mg/day thioridazine. After one month of treatment, the patient had significant improvement in both psychiatric conditions and onychotillomania
[15]. In a patient with onychotillomania and fixed hypochondrial delusions that she had an unknown nail disease, pimozide (Orap) successfully treated the delusions, resulting in normal-appearing nails after seven months
[19].
In one case report, a 19-year-old woman with onychotillomania was treated with monthly intramatrical nail injections of triamcinolone acetonide (0.2 mL of 5 mg/mL) for 3 months, followed by bimonthly injections for 6 months and daily topical calcipotriol/betamethasone dipropionate. Nail appearance improved after three months, with completely normal nail folds, cuticles, and nail plates by eight months
[17].