1000/1000
Hot
Most Recent

There are HA-based scaffolds that can be used in wound healing as potential bioactive dressings such as bandages, topical gels, microspheres, nanoparticles, hydrocolloids, foams, transdermal/matrix patches, etc. Hussain et al. reported HA-functionalized nanoparticles for the co-delivery of resveratrol and curcumin for chronic diabetic wound treatment.
Some known factors that contribute to chronic wounds include diabetes, prolonged bed rest, obesity, smoking, age, etc. These wounds include leg ulcers, diabetic foot ulcers, etc. It is reported that the burden of treating chronic wounds contributes to an increase in healthcare costs worldwide. It occurs in four sequential stages: hemostasis phase, inflammatory phase; proliferation phase; and maturation phase, which is the final stage of wound healing [1][2].
There are several wound dressing materials that can be used for the treatment of wounds. Some of the dressings employed for wound healing include hydrogels [3][4][5][6][7][8][9][10], sponges [2][11], films [12][13][14][15], nanofibers [16][17], bandages [18][19][20][21][22], membranes [23][24][25][26][27][28][29], hydrocolloids [30], etc. There is no single wound dressing that is suitable for wound care of all wound types. Wound dressings can be encapsulated with bioactive agents to enhance their therapeutic outcomes on wound healing.
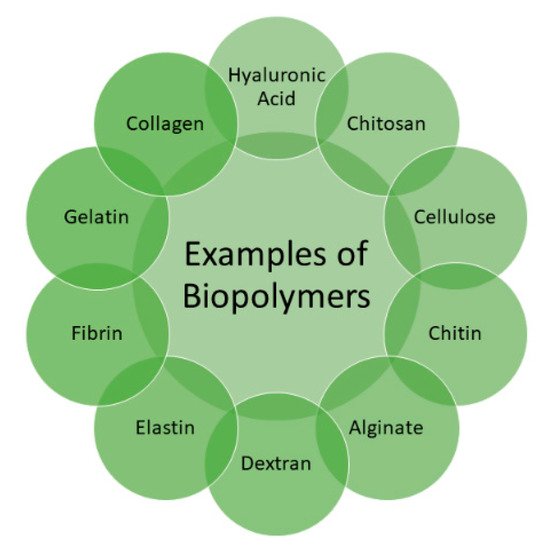
Several biopolymers (Figure 1) are utilized for the preparation of bioactive wound dressings, including hyaluronic acid (HA), cellulose, chitin, chitosan, fibrin, alginate, elastin, dextran, collagen, and gelatin [30], etc. These polymers possess excellent properties that can be significantly beneficial in wound healing, such as non-toxicity, biodegradability, biocompatibility, readily availability, and non-immunogenicity [31]. The factors that must be considered in the preparation of wound dressings include their capability to stop bleeding, combat infections, be easily sterilized, absorb wound exudates, accelerate wound healing and wound debridement, non-toxicity, gas permeability, good water vapor, ease of use, and biodegradability [32].
HA is known as the simplest glycosaminoglycan and it is a constituent of extracellular matrix (ECM) with distinct biological properties, wound healing potential, and physicochemical features. It is found and extracted from rooster combs, synovial fluid, umbilical cord, and vitreous humor [33]. It is biocompatible, non-toxic, biodegradable, exhibits hydrophilic property, non-allergic, and naturally lacks immunogenicity with a broad range of applications [34]. It possesses many essential physiological properties, such as lubrication, space-filling, and structural properties, retention abilities, and ECM water sorption [35].
Hyalosafe® is a transparent film utilized in the wound care and treatment of second-degree burns [36]. The biodegradation of this wound dressing significantly results in the release of HA that promotes epithelial cell proliferation [36]. Hyalomatrix®is a conformable, flexible, and bilayered dermal material that promotes wound closure and dermis regeneration. The transparency of the top layer is necessary to monitor the wound healing process and the therapeutic outcome of Hyalomatrix®in clinical studies.
This wound dressing possesses the capacity to absorb and release a large volume of water, ensuring skin hydration during the wound healing process. It is a gel scaffold and is made up of a mixture of 2.5% sodium hyaluronate and emollients that hinder the dehydration of tissue and support wound healing. There are various types of wounds that can be treated with this gel, including diabetic, leg, and pressure ulcers, and it is suitable for the management of bleeding wounds [37]. It is regularly utilized for the treatment of acute and chronic wounds [38].
It is used for chronic wound management, including diabetic foot ulcers. Although several efforts have been achieved thus far, the clinically and commercially employed HA-based scaffolds used for wound dressings still demonstrate some limitations. Some of the limitations are the possible occurrence of impurities (because of the extraction process employed to get HA), high production costs, low mechanical stability, and limited cell proliferation and adhesion [39]. There are various HA-based scaffolds that are used in wound management (such as hydrogels, sponges, films, foams, membranes) that are currently under development to overcome the shortcomings mentioned above.
It greatly offers a biomimetic and moist environment for the growth of cells. These unique features of hydrogels have attracted their application in the field of wound management. Hydrogels are formulated from natural and synthetic polymers, and they exhibit essential properties that can be advantageous in tissue regeneration. Several strategies are used to overcome these limitations, including crosslinking with synthetic polymers and chemical modification.
formulated gelatin-crosslinked HA-based hydrogels entrapped with recombinant thrombomodulin for wound treatment in diabetic mice [40]. All the HA-based hydrogels exhibited excellent water absorption behavior, which may help absorb wound exudates and promoted good drug absorption at the wound bed. The complete release of thrombomodulin from HA hydrogels occurred in 12 h. The in vivo healing studies on diabetic mice displayed that the hydrogels loaded with thrombomodulin demonstrated significantly more healing effect when compared to plain hydrogels but did not differ from free thrombomodulin solution [40].
FTIR spectra revealed the successful loading of arginine derivative in the hydrogels. The intracellular antioxidant tests using hydrogen peroxide-induced stress damage to the NIH 3T3 cells demonstrated that oxidative stress decreased with increasing concentration of arginine derivative in the hydrogels, which could be advantageous for wound healing. The wound healing experiment in vivo in the rat model displayed that the increase of arginine derivative concentration in hydrogels significantly promotes a faster healing mechanism than the control. Furthermore, the wounds treated with a hydrogel with the highest concentration of arginine derivative showed almost complete healing on day 21 [41].
The antibacterial efficacy of the hydrogel against methicillin-resistantS. aureusshowed that the average zone of inhibition of vancomycin-loaded hydrogels ranged between 5.7 ± 0.6 and 21.4 ± 0.7 mm post overnight culture. These results can be significantly beneficial in wound treatment [42]. formulated conformable HA-based hydrogels loaded with adipose-derived stem cells for burn injury treatment. The in vivo wound healing of the hydrogels on a deep second-degree burn wound murine mice model demonstrated significantly faster closure of the wound and reduced the scar development [43].
This swelling efficiency is beneficial for carrying signal factors and nutrients between cells cultured in the HA hydrogel and cells on the wound, resulting in stimulation of the cell outgrowth. The in vivo healing analysis using full-thickness wound in mice showed that wounds treated with the hydrogels displayed a healing process, which was higher compared to the commercial drug and free collagen hydrogel, HA hydrogel samples because the combination of collagen and HA enhanced the wound healing [44]. designed in situ HA hydrogels encapsulated with plasmid DNA encoding vascular endothelial growth factor for the treatment of burn wounds. The in vivo wound healing studies of the hydrogels using Sprague Dawley mice demonstrated accelerated healing on splinted burn wounds, specifically by hindering inflammation reaction and stimulating microvascular development while being biocompatible [45].
The evaluation of the wound healing mechanism in vivo on a full-thickness skin model revealed a controlled release of EGF from HA hydrogels and excellent healing capacity with respect to angiogenesis, granulation tissue production, and growth factor levels [46]. The rheological evaluation showed that the hydrogels have excellent mechanical properties with gelation temperature near the physiological temperature; hence, they can be simply locally employed on the injured site. Cytotoxicity assay displayed that the HA hydrogels have excellent biocompatibility on L929 cells. The in vitro model of wound healing demonstrated that the AgNPs nanoparticle-loaded hydrogels permit accelerated wound closure and restoration than the control [47].
The in vitro drug release profile of HA hydrogels showed sustained methylene blue release over 48 h. These results revealed that HA hydrogels could be beneficial in wound treatment [48]. The physicochemical properties of hydrogels were confirmed by NMR, FTIR, and gel permeation chromatography (GPC). The cytotoxicity study using MTT assay on the hydrogels demonstrated high cell viability of HFFF2 human fibroblast cells.
designed HA-based spongy hydrogels loaded with human adipose stem cells for diabetic wound treatment. These spongy hydrogels demonstrated improved diabetic wound healing by significantly modulating the inflammatory response and re-epithelialization to stimulate effective neoinnervation [49]. The physicochemical properties of hydrogels were successfully confirmed by 1H NMR, FTIR, and X-ray diffraction (XRD). A hemostatic examination of the HA hydrogels demonstrated excellent hemostatic properties of ZnO-loaded HA hydrogels.
Films are flexible, transparent, and elastic materials made up of polymers-they permit oxygen and carbon dioxide exchange and diffusion of water vapor from the injury site and prevent penetration of bacterial/other microbial pathogens [50]. The transparency of films allows the monitoring of the wound continuously, without removing it [50]. However, films demonstrate a reduced capacity to absorb the wound exudate, making them unsuitable for high exuding wounds and may cause trauma if not removed appropriately [51]. Currently, HA films are developed by incorporating bioactive molecules (such as natural product extract, growth factors, inorganic compounds, and antibiotics) to improve their biological application.
formulated HA-based films incorporated with curcumin for wound healing [52]. The swelling analysis showed that curcumin-loaded films and plain films swelled rapidly within 15 min and reached a swelling equilibrium at 2 h, demonstrating that all the hydrogels have outstanding water absorption. The cytotoxicity study of free curcumin and curcumin grafted films on the L929 cells using MTT assay showed no adverse effect within 72 h. The hemolysis test demonstrated no significant hemolysis with concentrations of films reaching up to 15 mg/mL, revealing that the curcumin-loaded HA films have excellent biocompatibility.
prepared sodium-alginate crosslinked HA films loaded with AgNPs and sulfadiazine as topical bioactive wound dressings [53]. The SEM images exhibited crosslinked films that were homogeneous with no phase cracks. The drug release kinetics in vitro showed that the release of sulfadiazine was higher at pH 4.1 compared to pH 7.2, revealing a diffusion of sulfadiazine from a swelled film structure at pH 4.1 compared to the compact structure of the film at pH 7.2. The in vitro antibacterial analysis showed that a combination of sulfadiazine (as an antibiotic) with silver nanoparticles in the films results in more enhanced antimicrobial properties.
FTIR and XRD spectrums confirmed successful encapsulation of ZIF-8 in HA films, while SEM images demonstrated appropriate dispersion of frameworks in HA material. Analysis of the mechanical properties of the films showed Young’s modulus of 176 K Pa and decreased water contact angle of 27.7, showing improvement in hydrophilicity. The cytotoxicity test of plain films and ZIF-8 on L929 cells showed a high cell viability of more than 98%. The antibacterial results from the disc diffusion method confirmed better growth inhibition for the films loaded with ZIF-8 compared to the free films againstE. coliandS. aureus.
prepared transparent bilayered films based on HA and Polyvinylpyrrolidone (PVP). The in vitro drug release at physiological conditions demonstrated a drug release reaching almost 100% within the initial 24 h. The antibacterial results showed that bilayered films formed a zone of inhibition of 30.6 (±1.9), 42.9 (±3.2), 39.5 (±2.0) mm againstS. aureus,P. aeruginosa, andE. coli, respectively, revealing their good antibacterial activity. The in vivo biocompatibility and bioresorption studies of the films in a full-thickness wound on mice model showed no observable side effects.
Michalska-Sionkowska et al. designed thin films that are based on HA, chitosan, and collagen. The contact angle analysis showed that the hydrophilicity of film decreased when gentamicin was added. The water vapor transmission analysis showed that the presence of gentamicin in thin films resulted in increased water vapor permeability. The in vitro antimicrobial results revealed that the films based on HA and other biopolymers encapsulated with gentamicin inhibited the growth ofP. aeruginosa,S. aureus, andE. coli.
They were loaded with glutathione for enhanced wound treatment [54]. The porosity analysis utilizing ethanol as a hydrophilic solvent demonstrated that the addition of glutathione increased the porosity of plain membrane from 37.53 ± 1.88% to 43.26 ± 2.16%, which is useful for promoting their surface area and the adsorption capacity. The wound healing results in vivo employing a rat model demonstrated rapid wound healing for the drug-loaded membranes. Furthermore, in vivo study results revealed that the membranes loaded with glutathione are an appropriate wound dressing for treating chronic wounds [54].
designed polyvinylidene fluoride–hyaluronic acid membranes loaded with active pharmaceutical ingredient ionic liquids (API-ILs) for wound healing. The SEM analysis showed that the increase in the concentration of polyvinylidene fluoride resulted in spongy region development, which can contribute to more polymeric chains and higher viscosity. The uptake analysis revealed that the shape, size, and interconnectivity of pores affected the membrane uptake of API-ILs. Cell adhesion of fibroblasts on HA-based membrane surfaces and cell viability evaluation confirmed enhanced viability and adhesion of fibroblasts on the membranes.
Figueira formulated polycaprolactone-HA electrospun bilayer nanofibrous membrane encapsulated with salicylic acid for tissue regeneration [55]. The physicochemical properties of the nanofibrous bilayer membrane loaded with salicylic acid were evaluated, and the achieved results demonstrated that the formulated electrospun scaffolds exhibited suitable mechanical properties, ideal porosity, controlled water loss, and a significant salicylic acid drug release mechanism. The antimicrobial analysis showed higher growth inhibition againstS. aureus. The results reveal that these membranes displayed suitable properties to be employed in wound treatment [55].
Sponges are wound dressings that can absorb large quantities of wound exudates, and they provide a moist environment for the wound because of their high porosity, swelling profile, and biodegradability [56]. Generally, sponges are non-adhesive and require secondary wound dressing or bandages/tapes to keep them at the wound site [57]. The FTIR spectrum showed the expected functional groups of biopolymers and confirmed the successful encapsulation of nanoparticles in the sponges. Furthermore, endothelial cells loaded on the sponges were well proliferated and demonstrated capillary-like tube development, which is a significant process in wound healing angiogenesis.
The swelling analysis showed a swelling percentage of 217 ± 11%, thus revealing a high efficiency of the sponges to absorb wound exudates. The cytocompatibility analysis of sponges showed that the VEGF released from the sponges was active in promoting the proliferation of HUVEC cells, and the cell viability was not affected by the presence of VEGF in the plain sponges [58]. They were loaded with platelet lysate for the treatment of chronic wounds. The results from this study revealed that platelet lysate stimulates keratinocyte epithelialization and controls fibroblast matrix deposition, offering a molecular basis for the capability of such hemoderivative to heal chronic wounds.
The porosity analysis of the sponges demonstrated that the loading of the nanoparticles significantly increased the porosity of sponges from 83.5% to porosity that ranges between 90.3% and 94.1%. The antimicrobial analysis of sponges showed that the addition of Ag nanoparticles increased the size of the inhibition zone in a concentration-dependent mode againstE. coliandS. aureus. The in vitro cytotoxicity examinations of the sponges using MTT assay demonstrated cell viability that was more than 80% on L929 cells. The in vivo healing analysis of sponges on full-thickness skin wounds using rabbits revealed healing on the third day, with slight inflammation and approximately 47% wound closure for the plain sponges, 69% for the sponges loaded with Ag nanoparticles, and only 5% wound contraction for the control (gauze)
prepared antimicrobial chitosan-HA sponges loaded with nanosilver for wound healing of infected diabetic foot ulcers. These sponges are potential wound dressings suitable for managing diabetic foot ulcers infected with antimicrobial-resistant bacteria [59]. Anisha and co-workers designed chitosan–HA composite sponge loaded with chondroitin sulfate nanoparticles. HA-based sponges exhibited a porosity of 67% and displayed improved blood clotting ability and swelling capacity.
Nanofibers are promising materials suitable for rapid and complete wound healing of chronic wounds, including burns, providing significantly enhanced outcomes more than the conventional wound dressings. There are several distinct properties of nanofibers, such as nanoscale structure, porosity, and large surface area. These features play vital roles in cell proliferation and attachment [16]. Nanofibers designed by electrospinning have triggered great interest in different applications such as drug-delivery systems, wound-dressing materials, and bio-nanotextiles because of their large surface-area-to-volume proportion [60][61].
The physicochemical properties and successful embedding of nanoparticles in the nanofibers were confirmed by UV-vis spectroscopy, FTIR, and Raman spectroscopy. The SEM analysis of nanofibers demonstrated an approximate average size diameter between 244 nm and 326 nm. The SEM and TEM results confirmed the electrospinning process of nanofibers embedded silver nanoparticles. The antibacterial assessments showed that nanofibers loaded with silver nanoparticles possessed high efficacy againstB. subtilis,E. coli,
The wound healing studies of nanofibers revealed the absence of abscess development or hypertrophic scars. These results showed the wound contracting capability of the silver nanoparticle-loaded nanofibers and free nanofiber treated groups. In contrast, the Garamycin®cream and control group epithelization occurred after more than 2 weeks. The nanoparticle embedded nanofibers and the plain nanofibers treated groups displayed important wound healing efficacy compared to other groups treated with Garamycin®cream and control group excision wound model [62].
There are HA-based scaffolds that can be used in wound healing as potential bioactive dressings such as bandages, topical gels, microspheres, nanoparticles, hydrocolloids, foams, transdermal/matrix patches, etc. reported HA-functionalized nanoparticles for the co-delivery of resveratrol and curcumin for chronic diabetic wound treatment [63]. The release analysis at pH 7.4 and 37 °C revealed the release of both drugs loaded followed biphasic release mode where a first burst release of both drugs occurred in the first 8 h followed by slower and sustained drug release. These results and properties confirmed that these nanoparticles could be very suitable for chronic diabetic wound treatment [63].
Abdel-Mohsen and co-workers formulated silver nanoparticle-loaded HA-based fabrics for chronic wound management. The resultant fabrics loaded with nanoparticles displayed consistent dispersion throughout the HA-based fabrics from SEM analysis, TEM and DLS analysis, demonstrating an outstanding distribution of silver nanoparticles with 25 ± 2 nm. The XRD results showed that the silver nanoparticles increased the crystallinity of the formulated fabrics as well as the thermal stability. In vivo wound healing analysis using non-diabetic/diabetic rat models showed that the formulated fabrics loaded with silver nanoparticles displayed strong healing efficacy compared to the free HA fabrics and significantly accelerated the wound healing process [64].
The analysis of mechanical properties of these wound dressings showed the tensile strength ranging between 4.91 ± 0.5 and 3.07 ± 1.1 MPa while the elongation at break ranged between 379.8 ± 23 and 453.6 ± 38.5 MPa. The mechanical properties showed that these nanofibrous scaffolds are appropriate for wound dressing. The antimicrobial analysis showed that propolis-incorporated nanofibrous scaffolds caused significant inhibition zones againstE. coliandS. aureus. The wounds treated with the propolis loaded nanofibrous scaffolds closed on day 14, whereas the wounds treated with the free polyurethane and control groups were still open [65].
Fahmy and co-workers formulated chitosan-HA non-woven fabric wound dressing incorporated with silver nanoparticles. The elemental analysis of the dressings loaded with nanoparticles confirmed the presence of Ag NPs in the non-woven fabric wound dressing. formulated Antibacterial HA-based foams incorporated with zinc oxide nanoparticles. The foams loaded with 3% cephalosporin revealed only half of the same reduction rate.
formulated a 3-dimensional dermal matrix based on HA loaded with resveratrol for diabetic wound treatment [66]. The water uptake analysis showed the water uptake capacity of more than 80% arising from the porous material of the dermal matrix, resulting in good absorbent characteristics. The in vivo wound healing analysis of the 3-dimensional dermal matrix loaded with resveratrol on wounded diabetic rats showed that the wounds were fully healed at the end of 2 weeks compared to those treated with resveratrol solution and the plain dermal matrix [66]. ) × 1014 kg/(s m Pa)), which make them potentially appropriate for the treatment of different wound types at various wound healing phases [67].