Precision oncology is an emerging approach in cancer care. It aims at selecting the optimal therapy for the right patient by considering each patient’s unique disease and individual health status.
1. Breast Cancer: Why Precision Oncology?
Precision medicine, also called personalized medicine, is an emerging approach for disease treatment and prevention that takes into account genetics, epigenetics, metabolism, environment, and lifestyle of each individual person with the goal to select the optimal therapy for the right patient. In oncology, tumor molecular profiling leads to the identification of patient specific alterations that could inform about the optimal treatments and maximize patient’s survival.
For several years breast cancer (BC) has been seen as a single clinical entity and treated with one general approach. However, now it has become extremely clear that BC has to be considered a highly heterogeneous disease with different subclasses. The discovery of endocrine receptors, and the understanding that endocrine therapy significantly improves outcomes in patients with hormone receptor-positive disease, marks the beginning of the target therapy for patients with BC
[1][2][3]. By the late 1990s, it was discovered that a subgroup of breast tumors (15–20%) overexpresses the HER2 receptor or have HER2 gene amplification. HER2-positive disease had a dismal outcome until the development of targeted agents, which has significantly improved outcomes in both the (neo)adjuvant
[4][5][6][7][8] and the metastatic setting
[9][10]. The more recent gene-expression assays allow clinicians to assess the risk of recurrence in early breast cancer (EBC)
[11][12][13], as well as to predict potential benefit from adjuvant chemotherapy
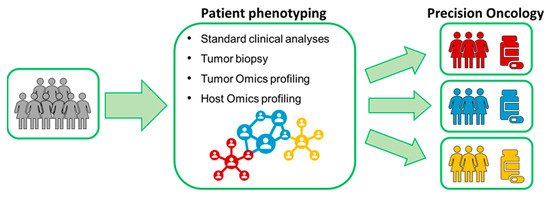
[14][15][16][17]. In many patients found to have a disease with favorable gene-expression profile, chemotherapy could be avoided; however, a significant population of EBC patients may still be overtreated. Precision oncology aims at identifying the optimal treatment for each patient, specifically tailored to each unique cancer profile and to each individual health status in order to maximize survival and quality of life. Omics sciences are instrumental for this aim ().
Figure 1. Precision oncology in a nutshell.
Metabolomics, one of the latest -Omic sciences, entails the comprehensive characterization of the ensemble of endogenous and exogenous metabolites presents in a biological specimen. Metabolites simultaneously represent the downstream output of the genome, the transcriptome, and the proteome, as well as the upstream input from various external factors such as environment, lifestyle, diet, and drug exposure [18]. As a consequence, in the last few years, metabolomic phenotyping has been extensively applied in biomedical research.
Nuclear Magnetic Resonance spectroscopy (NMR) and mass spectrometry are the two most widely used analytical platforms for metabolomics. These two techniques can be considered complementary, since the weaknesses of one platform are compensated by the strengths of the other [19]. In contrast to the approach typically adopted in mass spectrometry, which is focused on target metabolites of interest, NMR metabolomics is usually performed using a high-throughput, untargeted approach, which provides a complete picture of all metabolites present or quantifiable in the sample above the NMR detection limit (concentrations >1μM) [19][20]. To date, NMR metabolomics are increasingly used for successful patient stratification in various diseases, and it provided unique insights into the fundamental causes of several physiological and pathophysiological conditions [18][19][20][21][22][23][24][25][26][27][28][29][30][31][32].
3. Translation of NMR-Based Metabolomics in Clinics
BC is the most common type of cancer and the second most common cause of death in women worldwide
[33]. Early detection and prompt treatment has been associated with a significantly improved prognosis observed over time in patients with BC.
The serum tumor markers, CEA and CA 15.3, are routinely used in therapy monitoring and follow up of patients with BC; conversely, their sensitivity and specificity for early diagnosis are poor
[34]. Mammography is considered the gold standard in BC screening, however it has a sensitivity of 86.9% with relevant variability depending on tissue density and age
[35].
Malignant tumors are characterized by increased gluconeogenesis, glycolysis, and fat mobilization, and decreased protein synthesis. The results described in the original article show that these metabolic changes peculiar to malignant neoplastic change can be detected by metabolomics. Metabolomics is able to discriminate between cancer and normal breast tissue from the same patient with accuracy, sensitivity, and specificity around 90%
[36]. Moreover, the metabolite analysis of blood and urine samples from BC patients differs significantly from healthy controls
[37][38][39][40][41][42][43]. This evidence offers potential for the use of metabolomics, a minimally invasive technique, for early diagnosis of BC in the general population
[44].
BC is a heterogeneous disease with high variability in prognosis and response to treatment driven by genetic, epigenetic, and phenotypic differences. The identification of the mechanisms underpinning this heterogeneity support the development of new drugs targeted to specific subgroup of patients, with the final aim to improve patient outcome. Transcriptomics and proteomics have attempted to classify breast tumors according to gene expression (intrinsic molecular subtypes—
[45]) and protein expression (RPPA subtypes—
[46]). Metabolomics can provide additional information to these -omics, leading to a deeper tumor characterization. ER and HER2 status are well estimated by metabolite analysis
[47]. In addition, metabolomics can identify metabolic clusters within breast tumors, not reflecting the intrinsic molecular subtypes, but presenting significant differences in gene expression and protein expression profiles, and unique susceptibility to metabolically targeted drugs
[48].
Neoadjuvant chemotherapy is commonly used to treat BC, not only for downsizing tumors, but also for the potential to monitor individual drug response. Moreover, in selected molecular subtypes, the achievement of a pCR after neoadjuvant treatment correlates with excellent long-term outcomes and a lower risk of disease recurrence
[49]. Currently HER2 positivity, triple negative subtype, high Ki67, and the presence of tumor infiltrating lymphocytes (TILs) are the biomarkers most frequently used in recommending neoadjuvant chemotherapy. Predicting response to chemotherapy can spare patients with unresponsive disease from unnecessary side effects. Metabolomics was shown to play a role in predicting response to NAC.
Metabolomic profiling of serum samples collected before neoadjuvant chemotherapy was able to predict response in two small cohorts of patients. The first cohort was unselected for molecular subtype
[50], while the second included only HER2-positive breast tumors
[51]. The potential role of metabolomics in predicting response to treatment was also evaluated on breast tumor tissue. This analysis demonstrated that tumor metabolism changed significantly in response to neoadjuvant treatment. Metabolomic analysis on post-treatment tissue samples was able to discriminate between patients who experienced disease response to treatment and those who had non-responsive cancer. However, metabolomic analysis of pre-treatment tumor biopsies was not predictive probability of response to chemotherapy
[52][53][54].
Developing prognostic biomarkers is one of the focuses of metabolomics in BC. Clinicopathological features are used to predict the risk of recurrence or development of metastatic disease. More recently, gene-expression assays such as Oncotype DX and Mammaprint have been introduced in clinical practice to refine risk estimation and prediction from adjuvant chemotherapy. However, these assays are time consuming, expensive, and can overestimate the risk of recurrence
[55]. In addition, they are estimated on the primary tumor tissue and cannot identify the presence or absence of occult micro-metastases. Metabolomics can contribute to overcoming these limitations. As already detailed in the above paragraphs, our group developed a metabolomic score that classified patients as high or low risk of recurrent disease on the basis of the degree of metabolomic similarities with MBC fingerprints
[56][57]. A high metabolomic score correlates with increased risk of recurrence and worse disease-free survival. Moreover, this metabolomic risk score can be used to sub-stratify the three Oncotype DX risk categories
[58].
However, how far are we now from adopting NMR-based metabolomics as a population-wide screening method? The conceptual distance from the present situation to this ambitious goal is still wide, but it can be bridged by working in two directions: first it is necessary to standardize both the pre-analytical and the analytical procedures. Indeed, the biochemical composition of biospecimens is affected by how samples are collected, stored, prepared, and analyzed, and consequently differences in these steps can be particularly detrimental in multi-center studies
[59]. Specifications for pre-examination processes for metabolomics in urine, venous blood serum and plasma have been already published by CEN (CEN/TS 16945:2016)
[60]; however, these recommendations are still not universally employed. Secondly, to increase the robustness and the reliability of the results already provided, well-planned, large-scale, multicenter, population-based studies in which all heterogeneous BC patient groups are well represented are needed. NMR-based metabolomics is a fast, high-throughput, robust, and reproducible technique, thus moving from the analysis of hundreds to thousands of samples is realistically an approachable target
[61][62].